Vancomycin-resistant Enterococcus faecium (VREF) is an alarming pathogen that poses a significant threat to public health due to its increasing prevalence in healthcare settings. Recent genomic analyses have shed light on the alarming genomic evolution of VREF, particularly during the ongoing VREF outbreak in Shenzhen, China. The emergence of antimicrobial resistance genes among VREF strains has raised concerns about their ability to adapt and spread rapidly. Whole-genome sequencing has unveiled two distinct subpopulations within the dominant sequence type 80 lineage, underscoring the complex nature of Enterococcus faecium resistance. To effectively combat this healthcare challenge, it is crucial to enhance genomic surveillance and monitor the evolving characteristics of VREF in hospital environments.
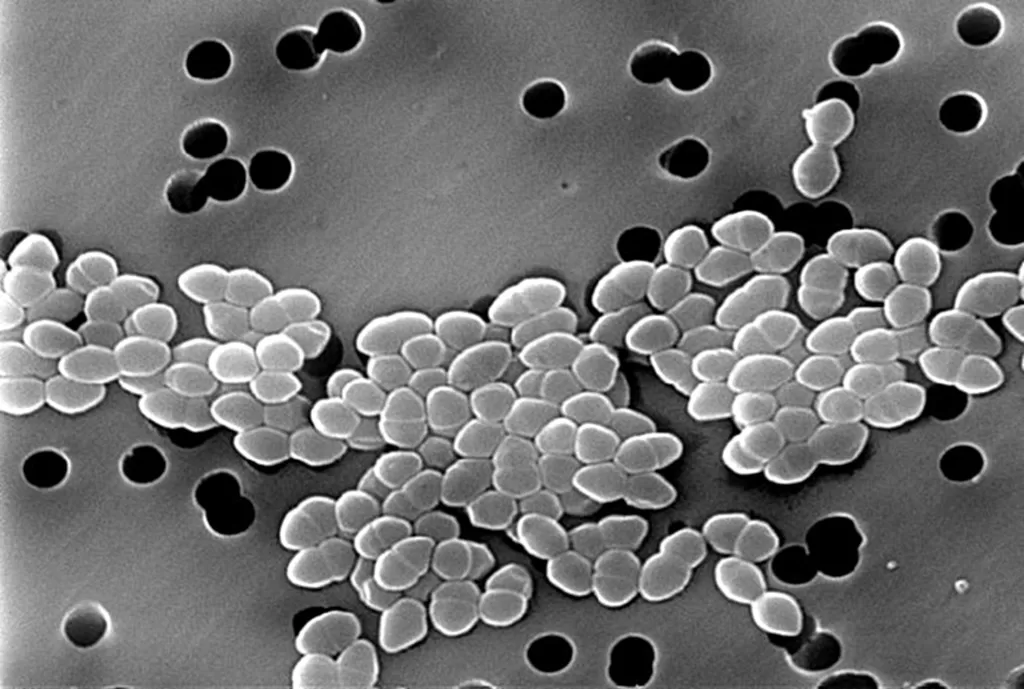
The rise of vancomycin-resistant Enterococcus faecium (often referred to as VREF) illustrates a growing challenge in the realm of antimicrobial resistance. This gram-positive bacterium, notorious for its prevalence in hospital-acquired infections, has shown remarkable adaptability due to genetic changes driven by recombination and acquisition of resistance genes. Recent studies have highlighted the genomic evolution of VREF during outbreak scenarios, particularly through whole-genome sequencing efforts that reveal new clonal variations. Understanding the dynamics of Enterococcus faecium resistance is essential for developing effective infection control strategies in healthcare settings. As researchers continue to document VREF outbreaks, the need for vigilant monitoring and intervention strategies becomes increasingly urgent.
Understanding vancomycin-resistant Enterococcus faecium (VREF)
Vancomycin-resistant Enterococcus faecium (VREF) is an opportunistic pathogen that poses a major challenge in healthcare settings due to its resistance to multiple antibiotics, especially vancomycin. This resistance complicates treatment regimens for infections that may arise post-surgery or in immunocompromised patients. In recent years, the prevalence of VREF has surged, largely attributed to the rapid emergence of new clones that adapt through horizontal gene transfer. This adaptability allows VREF to thrive in hospital environments, where it often resides in the gastrointestinal tract of healthy individuals, subsequently leading to nosocomial infections.
The genomic analysis of VREF isolates indicates that specific sequence types, particularly the sequence type 80 (ST80), have outpaced other lineages globally. Understanding the genetic makeup and transmission dynamics of VREF requires advanced tools like whole-genome sequencing (WGS), which provide insights into its evolutionary mechanisms. Continuous monitoring and research are essential not only to track the spread of VREF but also to develop targeted interventions to reduce its impact in clinical settings.
The Role of Whole-Genome Sequencing in Tracking VREF Outbreaks
Whole-genome sequencing (WGS) plays a pivotal role in the surveillance of vancomycin-resistant Enterococcus faecium (VREF) outbreaks. By providing detailed insights into genetic variations and evolutionary pathways, WGS enables researchers to identify specific strains associated with outbreaks. For instance, during the ongoing VREF outbreak in Shenzhen, WGS identified the emergence of ST80 as the dominant lineage linked to increased resistance. Furthermore, WGS facilitates the mapping of transmission routes by comparing the genomes of isolates collected from different patients and locations.
In addition to tracking outbreaks, WGS helps researchers understand how antimicrobial resistance genes spread among different strains. The insertion of antimicrobial resistance genes often occurs through mechanisms such as plasmid transfer or mobilization via insertion sequences. This genomic understanding underlies the need for prompt responses to emerging threats posed by rapidly evolving VREF strains.
Genomic Evolution of Vancomycin-Resistant Enterococcus faecium
The genomic evolution of vancomycin-resistant Enterococcus faecium (VREF) has significant implications in understanding and controlling bacterial outbreaks. In the outbreak context, VREF demonstrates both vertical and horizontal gene transfer, which together facilitate rapid genetic change. Research has shown that during the outbreak periods, specific lineages such as SC11 demonstrate a primary reliance on recombination, which surpasses traditional mutation rates. Notably, studies revealed that insertion sequence-mediated recombination is a key factor in the emergence of new, resistant variants.
As WGS studies continue to evolve, they illuminate genomic traits unique to specific VREF subpopulations. The emergence of distinct subpopulations, such as the SC11 subset found in Shenzhen, reflects not only the evolutionary pressure applied by the clinical environment but also highlights the significance of genetic innovation in facilitating enhanced virulence and adaptability. Understanding these mechanisms is critical for developing strategies against potential future outbreaks.
Emergence and Spread of the ST80 Lineage
The ST80 lineage of vancomycin-resistant Enterococcus faecium has emerged as a dominant strain in various global regions over the last decade, particularly in healthcare settings. Capturing 40%-67.1% of VREF isolates in places like Denmark and Spain, this lineage thrives in high-density hospital environments where transmission rates can explode. In recent outbreaks, particularly in Guangdong Province, there is growing concern regarding the rapid dissemination of this lineage, which warrants intensive genomic surveillance to map its spread.
The distinction between subpopulations within ST80 has been identified through WGS, categorizing them based on their virulence factors and resistance profiles. For example, some variants have shown enhanced abilities to acquire additional antimicrobial resistance genes, illustrating an evolutionary advantage in persistently colonized environments. This adaptability underscores the importance of ongoing research to understand the evolutionary pressures influencing ST80’s predominant position among VREF lineages.
Features of Antimicrobial Resistance in VREF
Antimicrobial resistance in vancomycin-resistant Enterococcus faecium (VREF) is a growing concern in clinical microbiology. The landscape of resistance is constantly changing as strains acquire various resistance genes. The presence of the VanA operon, which confers resistance to vancomycin, is well-documented, but newer isolates are also documenting the acquisition of resistance genes like VanM. These developments complicate treatment options and necessitate a global approach to resistance surveillance.
The rise of plasmid-mediated mechanisms for acquiring resistance contributes to the rapid evolution of VREF strains. Whole-genome sequencing has demonstrated that accessory gene variations, including those for antibiotic resistance, significantly impact how these bacteria adapt to selective pressures in hospital environments. This adaptability emphasizes the pressing need for actionable responses to manage VREF effectively in healthcare settings.
Adaptive Mechanisms of VREF: The Role of Insertion Sequences
Insertion sequences (IS) play a crucial role in the genomic adaptability of vancomycin-resistant Enterococcus faecium (VREF). These elements facilitate the movement of genetic material within the bacterial genome, contributing to the horizontal gene transfer of antimicrobial resistance traits. In the context of the SC11 lineage, increased activity of IS elements has been correlated with enhanced resistance and metabolic capabilities, positioning certain subpopulations at a competitive advantage in clinical settings.
The high frequency of IS-mediated events allows VREF to rapidly adapt to changing environmental pressures, enhancing its survival even in heavily monitored hospital environments. Understanding the dynamics of IS elements provides insights into potential intervention points to disrupt transmission pathways and is a focal point for future research in controlling VREF outbreaks effectively.
Implication of Pangenomic Studies in VREF Research
Pangenomic studies provide a comprehensive view of the genetic makeup of vancomycin-resistant Enterococcus faecium (VREF) populations. By analyzing both core and accessory genes, researchers can delineate patterns of genetic diversity and understand the accessory gene variations that contribute to VREF’s survival and adaptability in healthcare settings. Such studies reveal not only the essential genes for basic survival but also highlight those associated with antimicrobial resistance and virulence.
Investigating the pangenome, researchers uncovered a significant ratio of accessory to core genes that reflects VREF’s evolutionary potential. The identification of genetic modules linked to virulence and antibiotic resistance underscores the need for continued genomic surveillance in clinical contexts to adapt and inform treatment decisions. Moreover, these analyses are pivotal in tracking the emergence of novel variants, ensuring preparedness in responding to VREF outbreaks.
Healthcare Strategies for Combatting VREF Infections
Effective strategies for combatting vancomycin-resistant Enterococcus faecium (VREF) infections in healthcare settings revolve around increased surveillance and preventative measures. Utilizing data from pangenomic and WGS studies can help healthcare professionals develop targeted interventions to mitigate the dissemination of VREF. Hospitals particularly need to implement strict infection control measures, which can include isolating infected patients and optimizing antibiotic stewardship programs to reduce unnecessary use of vancomycin.
Incorporating continuous genomic surveillance not only aids in identifying emerging VREF strains but also enhances our understanding of the evolving antimicrobial resistance landscape. By establishing databases of VREF genomic data, public health officials can coordinate responses to outbreaks more effectively, ultimately controlling the spread of this formidable pathogen in clinical environments.
Future Directions in VREF Research and Management
Future research on vancomycin-resistant Enterococcus faecium (VREF) will likely center around advancing our understanding of its genomic characteristics and resistance mechanisms. The continuous evolution of this pathogen necessitates an adaptive and proactive approach in healthcare research and management practices. Enhanced genomic surveillance methods, including WGS, will enable scientists to track VREF more effectively, while further investigations into the horizontal transmission of resistance genes will be essential to combat this public health threat.
Additionally, the exploration of novel therapeutic solutions, including phage therapy and new antibiotic classes, is imperative to restore effective treatments against VREF infections. By integrating genomic data with clinical insights, researchers can develop strategies that not only address current VREF strains but also anticipate future variants, fostering a more resilient healthcare approach to managing antimicrobial resistance.
Frequently Asked Questions
What is vancomycin-resistant Enterococcus faecium (VREF) and its significance in public health?
Vancomycin-resistant Enterococcus faecium (VREF) is a strain of Enterococcus faecium that has developed resistance to vancomycin, an important antibiotic used to treat severe infections. VREF poses a significant public health threat as it is responsible for many hospital-acquired infections globally, making infection control essential in healthcare settings.
How does whole-genome sequencing help in understanding VREF outbreaks?
Whole-genome sequencing (WGS) provides detailed genetic information about vancomycin-resistant Enterococcus faecium (VREF) strains during outbreaks. WGS helps identify specific sequence types, track the genomic evolution of VREF, and understand transmission patterns, which are crucial for outbreak management and prevention.
What are the key findings from genomic studies on VREF in Shenzhen, China?
Genomic studies in Shenzhen revealed two distinct subpopulations of sequence type 80 vancomycin-resistant Enterococcus faecium (VREF) diverging through recombination. These studies indicated that one subpopulation has gained additional antimicrobial resistance and carbohydrate metabolism genes, highlighting the ongoing genomic evolution of VREF that contributes to its spread.
Why is genomic surveillance necessary for controlling VREF transmission?
Genomic surveillance is critical for controlling vancomycin-resistant Enterococcus faecium (VREF) transmission as it allows for the identification of circulating strains, their mutation rates, and the emergence of new variants. This proactive approach is essential in predicting and preventing future outbreaks, especially with VREF’s rapid genomic evolution and adaptation.
What role do antimicrobial resistance genes play in vancomycin-resistant Enterococcus faecium?
Antimicrobial resistance genes are crucial for the survival and persistence of vancomycin-resistant Enterococcus faecium (VREF) in healthcare settings. These genes enable VREF to withstand treatment with antibiotics, complicating infection management and increasing the risk of severe, difficult-to-treat infections.
How has the clonal complex 17 of sequence type 80 VREF emerged globally?
Clonal complex 17 of sequence type 80 vancomycin-resistant Enterococcus faecium (VREF) has rapidly emerged as the dominant lineage in various countries, including Denmark and Spain. Its global rise can be attributed to its enhanced ability to adapt and spread within healthcare environments, leading to increasing isolation rates of VREF.
What are the implications of increased VREF isolation rates in Shenzhen since 2021?
The increased isolation rates of vancomycin-resistant Enterococcus faecium (VREF) in Shenzhen since 2021 indicate a growing public health concern, suggesting that the ongoing outbreak and transmission dynamics require urgent attention. This trend necessitates enhanced infection control measures and continuous genomic monitoring to prevent further spread.
What is the significance of insertion sequence-mediated recombination in the evolution of VREF?
Insertion sequence-mediated recombination significantly influences the genomic evolution of vancomycin-resistant Enterococcus faecium (VREF) by facilitating the acquisition of new genes, including antimicrobial resistance traits. This mechanism enhances genetic diversity and adaptability, making VREF a persistent threat in healthcare settings.
How do trends in hospitalization correlate with VREF infections?
Trends in hospitalization among patients with vancomycin-resistant Enterococcus faecium (VREF) infections indicate that individuals often have underlying health conditions, such as hypertension and kidney disease. Understanding these correlations is critical for identifying at-risk populations and implementing adequate preventive strategies.
What are the potential consequences of failing to monitor VREF outbreaks closely?
Failing to monitor vancomycin-resistant Enterococcus faecium (VREF) outbreaks closely can lead to unchecked transmission, the emergence of high-risk clones with increased virulence, and higher rates of hospital-acquired infections. Continuous surveillance is vital to mitigate these risks and improve patient outcomes.
| Key Points | Details |
|---|---|
| Genomic Evolution | Vancomycin-resistant Enterococcus faecium (VREF) underwent genomic evolution with two distinct subpopulations identified during an outbreak in Shenzhen, China. |
| Whole-Genome Sequencing (WGS) | WGS revealed divergence in sequence type (ST) 80 VREF through insertion sequence-mediated recombination. |
| Antimicrobial Resistance | One subpopulation acquired additional antimicrobial resistance genes, contributing to its pathogenic potential. |
| Prevalence Increase | VREF isolation rates in Shenzhen rose from below 6% before 2021 to an average of 11.53% by 2024. |
| Emerging Lineages | An independent lineage (SC11) emerged as a dominant strain during the ongoing outbreak, particularly in Guangdong Province. |
| Population Structure | Two subpopulations of SC11 (SC11-pop I and SC11-pop II) were identified, with differences in transmission and gene acquisition. |
| Importance of Surveillance | Continuous genomic surveillance is crucial to manage and mitigate the spread of VREF. |
Summary
Vancomycin-resistant Enterococcus faecium (VREF) poses a serious global health threat, particularly in hospital settings. This study demonstrated that the outbreak in Shenzhen, China, was characterized by the emergence of distinct genetic subpopulations, highlighting the dynamic nature of VREF evolution and adaptation. Increased surveillance and genomic analysis are essential to track the origins and spread of VREF, particularly the recent rise of sequence cluster 11. Understanding the genetic factors driving resistance and pathogenicity can guide efforts to control and prevent the dissemination of this formidable pathogen.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.