US flu activity has shown a notable decline over the past week, with the rates of influenza-like illness (ILI) sinking further below the baseline levels. According to the latest CDC flu report, the number of pediatric flu deaths has tragically risen to 198, highlighting the ongoing severity of this influenza season. Meanwhile, outpatient visits for ILI and respiratory illnesses only dipped slightly, decreasing from 2.5% to 2.4%. Hospitalization rates have also fallen, but with 4,639 patients hospitalized for the flu, the cumulative rate remains at its highest since the 2010-11 season. Alongside flu statistics, COVID-19 updates show that infection levels continue to decrease, presenting a complex yet hopeful picture for public health as we navigate through this respiratory illness season.
The recent trends regarding flu activity in the United States reflect a broader concern for public health and safety as winter approaches. With signs of decreasing instances of influenza and related health issues, the dynamics of seasonal respiratory illnesses such as influenza and other viral infections are becoming increasingly pertinent. Recent data, including pediatric flu fatalities and hospital admission statistics, reveal a pressing situation that poses challenges for healthcare providers nationwide. It’s essential to monitor these developments closely, as flu hospitalization rates and the ongoing situation with COVID-19 and RSV also play a significant role in public health discourse. Understanding these developments through reliable sources like the CDC’s reports can guide us in addressing the multifaceted challenges of this flu season.
Current Trends in US Flu Activity
In the latest report from the CDC, US flu activity has shown a noticeable decline, with rates of influenza-like illness (ILI) falling below baseline levels. This downward trend is a positive indicator for public health, suggesting that the peak of the flu season may have passed for some areas. Specifically, outpatient visits for flu-related symptoms decreased from 2.5% to 2.4%, confirming that fewer individuals are seeking medical attention for these illnesses. While this is encouraging news, public health officials remain vigilant as they analyze patterns and prepare for potential fluctuations in virus activity.
Despite the overall decline in flu activity, there has been a concerning increase in pediatric flu deaths, now totaling 198 this season according to the CDC. This statistic highlights the severe impact influenza can have on children, particularly during this season characterized by high hospitalization rates. As healthcare professionals monitor these trends, it becomes essential to encourage vaccination and preventative measures, especially for vulnerable populations, to mitigate these tragic outcomes.
The Impact of Pediatric Flu Deaths
The rise in pediatric flu deaths reported by the CDC underscores a critical area of concern for healthcare providers and parents alike. With a total of 198 deaths this season, the focus has shifted to understanding the strains responsible for these fatalities. Most new pediatric deaths were attributed to influenza A, specifically the H1N1 and H3N2 subtypes, which have shown significant transmission rates this year. The disparity in deaths compared to flu seasons in the past reinforces the urgency of vaccination campaigns aimed at protecting children during the high-risk flu season.
Efforts to educate parents on the importance of flu vaccinations for their children are paramount in preventing further fatalities. Health experts stress the significance of early intervention and monitoring symptoms to ensure timely treatment. As reported, the hospitalization rate for this flu season has reached 125.6 per 100,000 population, the highest since the 2010-11 season, reinforcing the need for increased awareness and proactive measures to safeguard children against these potentially fatal outcomes.
Flu Hospitalization Rates and Public Health Implications
The decline in flu hospitalization rates, with current figures showing 4,639 patients hospitalized compared to 6,448 the previous week, indicates a potential easing of strain on healthcare systems. However, despite this reduction, the cumulative hospitalization rate remains alarmingly high, prompting health officials to maintain vigilance. The significant hospitalization numbers suggest that although ILI rates have dropped, there are still many individuals affected by severe flu cases, necessitating continued public health messaging around flu prevention and control.
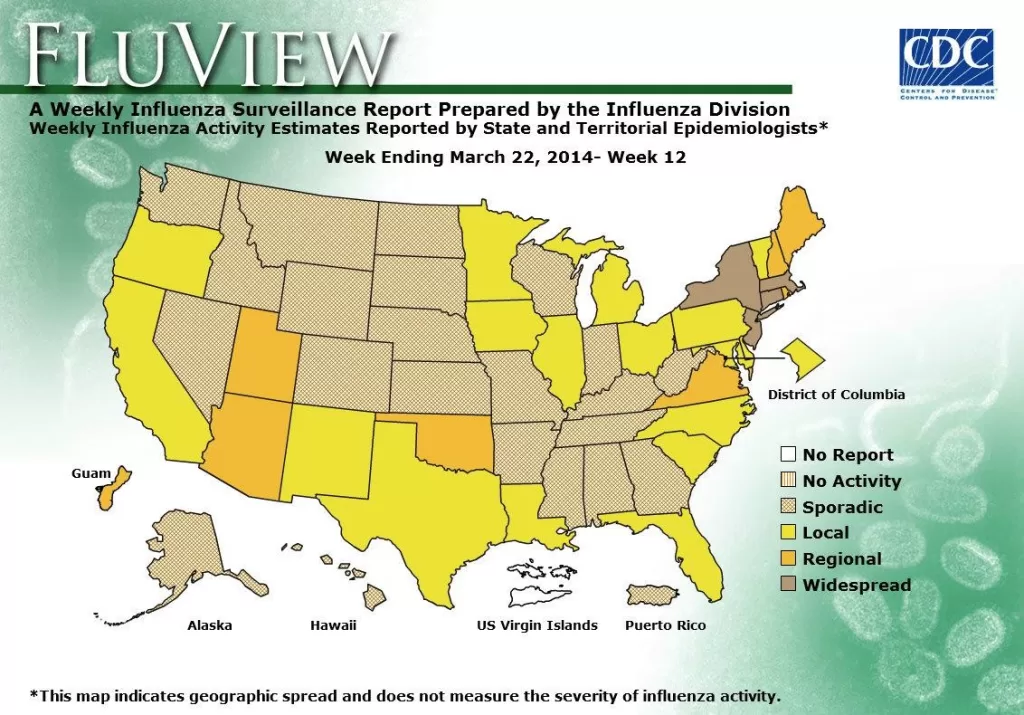
Healthcare systems are encouraged to prepare for the possibility of fluctuating hospitalization rates, especially as flu virus activity has shown variability across different states. Interestingly, while most states report lower ILI activity, New York is experiencing high levels, indicating localized outbreaks that can affect overall hospitalization rates nationwide. This highlights the need for adaptable healthcare strategies tailored to specific regions and situations, ensuring that resources and information are effectively allocated to combat ongoing flu risks.
Flu and COVID-19: An Update on Current Respiratory Illnesses
As flu activity trends downward, COVID-19 cases continue to show a similar pattern of decline, corroborated by recent CDC updates. The overall percentage of deaths caused by COVID-19 for the previous week held steady at 0.7%, which is slightly higher than the 0.5% recorded for flu. This information suggests that while both respiratory viruses pose risks, public health attention may shift toward the emerging understanding of co-infection scenarios, particularly as flu and COVID-19 circulate simultaneously.
The interplay between COVID-19, flu, and respiratory syncytial virus (RSV) further complicates the respiratory health landscape. Current reports indicate test positivity rates for flu at 6.7%, for RSV at 2.5%, and COVID-19 at 3.4%, all showing decreases from the previous week. This reduction is encouraging, yet ongoing monitoring is crucial as public health agencies aim to provide comprehensive strategies to combat these illnesses, particularly during the transitional phases of flu and COVID-19 seasons.
Understanding Influenza-Like Illness Trends
Understanding trends in influenza-like illness (ILI) provides valuable insights into the epidemiology of flu. The reported decrease in ILI, now at 2.4%, reinforces the effective public health interventions that may have played a role in containing the spread of the virus. Various factors contribute to these trends, including vaccination rates, public awareness, and seasonal variations in virus transmission. Continued surveillance is essential to glean information that can influence future strategies for cold and flu prevention.
Moreover, the relationship between ILI and actual influenza cases is crucial for assessing the overall impact of the flu season on public health. Seasonal surveillance methods, such as analyzing outpatient visit percentages and laboratory test results, allow health officials to gauge both the emergence and decline of ILI in distinct populations. This data-driven approach enables more effective communication to the public about mitigating risks associated with influenza outbreaks.
The Role of Vaccination in Flu Prevention
Vaccination remains a vital strategy in preventing flu-related illness and death, especially among high-risk groups such as children and the elderly. With the CDC focusing on vaccination campaigns, it is essential to reinforce public awareness of the importance of flu shots each season. Reducing circulation of flu strains through widespread vaccination can significantly lower hospitalization and death rates, particularly during peak flu activity periods.
Furthermore, healthcare providers play a crucial role in encouraging vaccination and addressing any hesitancy that may exist within communities. Direct engagement with patients to discuss the benefits and safety of vaccines helps build trust in public health measures. As flu season progresses, continued emphasis on vaccination can be a key factor in minimizing the risk of severe flu outcomes, including hospitalizations and fatalities.
Monitoring Flu Hospitalization Rates: What It Means for Public Health
Monitoring flu hospitalization rates provides essential data for understanding the severity and impact of influenza each season. Currently, hospitalization rates stand at their highest levels for over a decade, prompting health authorities to evaluate healthcare responses and allocate necessary resources. Tracking these rates helps identify trends and patterns that could guide public health interventions, such as increased staffing or funding for healthcare facilities in high-burden areas.
Moreover, these hospitalization statistics are used to inform the broader public about the flu’s impact on communities. High hospitalization rates signal the public health need for robust educational campaigns, urging individuals to seek vaccination and stay alert to symptoms. By maintaining a focus on these critical metrics, health officials can respond more effectively to the evolving landscape of respiratory illnesses.
Cross-Virus Surveillance: The Intersection of Flu and COVID-19
Cross-virus surveillance captures the dynamic interplay between influenza, COVID-19, and other respiratory viruses, illustrating the need for coordinated health responses. The CDC’s current updates showing decreased positivity rates for both flu and COVID-19 indicate a shift in the respiratory illness landscape, yet caution is paramount. As similar viruses circulate, maintaining vigilance in surveillance ensures that spikes in illness are promptly detected and addressed before they escalate.
Additionally, understanding the patterns of co-infection between flu and COVID-19 helps healthcare providers develop targeted strategies for testing and treatment. Communication between public health officials and healthcare systems ensures that response strategies are aligned, enhancing patient care during overlapping respiratory illness seasons. Continued research and monitoring will be crucial in comprehensively addressing the complexities surrounding these viruses.
Preparing for Future Flu Seasons: Insights and Recommendations
As this flu season progresses, insights from current data can inform preparations for future seasons. The CDC’s ongoing analysis of flu activity provides a roadmap for understanding expected patterns of illness. Preparing healthcare systems for both anticipated peaks in flu activity and potential co-infections with COVID-19 emerges as a primary focus of public health recommendations.
Recommendations for next flu season include enhancing vaccination outreach efforts and maintaining public education surrounding flu symptoms and prevention strategies. Collaborative strategies across healthcare systems will strengthen community resilience against seasonal respiratory illnesses, ultimately contributing to reduced morbidity and mortality rates. Through proactive planning and comprehensive education, we can better navigate the challenges presented by upcoming flu seasons.
Frequently Asked Questions
What are the current US flu activity trends and statistics?
US flu activity has shown a steady decline, with rates of influenza-like illness (ILI) falling to 2.4%. The number of flu hospitalizations decreased to 4,639, while test positivity for flu is now at 6.7%. Despite the overall decline, the CDC reported a total of 198 pediatric flu deaths this season.
How many pediatric flu deaths have been reported in the US this season?
As of the latest CDC flu report, there have been 198 pediatric flu deaths reported this season. This number is lower than the 207 deaths reported during the entire previous flu season.
What impact does the current flu activity have on hospitalizations in the US?
Flu hospitalization rates in the US have decreased significantly, with 4,639 patients hospitalized for flu last week, down from 6,448 the previous week. The cumulative hospitalization rate of 125.6 patients per 100,000 is the highest recorded since the 2010-11 flu season.
Is the flu activity in the US higher in any specific states?
Currently, New York is experiencing high influenza-like illness (ILI) activity, while other states show either moderate or low activity. The CDC’s weekly update indicates that only one state has high ILI activity this week.
How do pediatric flu deaths compare to COVID-19 deaths in the US?
This past week, the percentage of deaths caused by flu was 0.5%, slightly lower than the 0.7% for COVID-19. The impact of flu-related deaths, particularly among pediatric cases, remains concerning as flu fatalities continue to be reported.
What should the public know about flu activity and COVID-19 updates?
As of the latest reports, flu activity is declining, with lower test positivity and hospitalization rates. COVID-19 levels are also low and continue to decrease, indicating a potentially more manageable public health landscape for these respiratory illnesses.
How do the 2023 flu hospitalization rates compare to previous seasons?
The current hospitalization rate of 125.6 per 100,000 population is notably the highest since the 2010-11 flu season, indicating that while the recent trends show a decline in US flu activity, the overall toll of flu this season is significant.
What strains of influenza are being reported this flu season?
Among the pediatric flu deaths reported, nine were attributed to influenza A and one to influenza B. Of the influenza A cases tested, five were identified as the H1N1 strain and three as H3N2.
| Key Point | Details |
|---|---|
| Flu Activity Decline | Flu activity declined steadily, with ILI rates below baseline levels. |
| Pediatric Deaths | Total flu-related deaths in children increased to 198 this season. |
| Hospitalization Rates | Patients hospitalized for flu decreased to 4,639 from 6,448. |
| State-Specific Activity | New York reported high ILI activity, while two states have moderate activity. |
| Test Positivity | Flu test positivity decreased to 6.7% from 7.6% last week. |
| Comparison with Other Illnesses | COVID-19 and RSV levels remain low, with flu slightly higher in mortality. |
Summary
US flu activity has shown a notable decline, indicating a positive trend in public health as the rates of influenza-like illness continue to fall. While pediatric flu-related deaths have increased, the overall hospitalization rates are decreasing, suggesting that the peak of this season may be behind us. Nevertheless, monitoring will continue as specific states still exhibit high ILI activity. It’s imperative to remain vigilant as we move through the flu season.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.