Salmonella Dublin is emerging as a critical health concern not only in cattle but also in humans, largely due to its rising levels of antimicrobial resistance. This zoonotic pathogen is frequently linked to severe foodborne diseases, emphasizing the interconnectedness of livestock health and human safety. Recent studies highlight that Salmonella Dublin poses significant threats to both cattle health and public health through outbreaks associated with contaminated food products like raw milk and undercooked beef. Understanding its genetic evolution through a One Health approach is essential, as it enables researchers to track strain transmission across humans, animals, and environmental sources. As the situation evolves, prioritizing antimicrobial stewardship becomes vital for mitigating the risks posed by this resilient pathogen.
The term Salmonella Dublin encompasses a particular subtype of the Salmonella bacterium notorious for causing serious infections. This pathogen serves as a bridge between cattle health and human safety, illustrating the critical nature of addressing antimicrobial resistance in both domains. Often regarded as a zoonotic threat, Salmonella Dublin is implicated in numerous foodborne illness outbreaks, spotlighting the everyday implications of its presence in the food supply. With increasing concerns, adopting a holistic One Health perspective becomes imperative, aligning efforts from veterinary, environmental, and human health sectors. Tackling such multi-faceted challenges necessitates a collaborative approach focused on enhancing food safety and controlling pathogen spread.
The Emerging Threat of Salmonella Dublin
Salmonella Dublin is a concerning subtype of the Salmonella bacterium that has increasingly garnered attention due to its rising antimicrobial resistance (AMR). This zoonotic pathogen not only affects cattle but also poses significant risks to human health, especially through contaminated food products. Recent studies have demonstrated that S. Dublin is the most predominant Salmonella serovar in clinical cases involving cattle, leading to invasive infections, particularly in calves. Understanding the epidemiology of this pathogen is crucial, as it may lead to severe foodborne disease outbreaks stemming from products like raw milk and undercooked beef.
The implications of S. Dublin’s spread are profound, going beyond individual cases to impact public health and food security on a national scale. As researchers analyze genomic data from various sources—both clinical and environmental—it is evident that the ability of S. Dublin to adapt and thrive in different reservoirs complicates control efforts. An urgent focus on antimicrobial stewardship and effective management strategies is necessary to mitigate the potential threat posed by this resilient strain.
Understanding Antimicrobial Resistance in Salmonella Dublin
The rising levels of antimicrobial resistance (AMR) detected in Salmonella Dublin highlight the urgent need for enhanced surveillance and control measures. This strain displays a concerning ability to acquire resistance genes, particularly against common antibiotics used in both human and veterinary medicine. The study conducted by researchers from Penn State emphasizes the presence of multiple resistance genes within strains sourced from cattle, underscoring the critical need for effective antimicrobial stewardship to curb the proliferation of resistant bacteria in agricultural settings.
Moreover, the interconnectivity of S. Dublin across human and animal populations necessitates a One Health approach to combatting AMR. This perspective recognizes the links between animal health, environmental factors, and human health, advocating for integrated strategies that address the emergence and spread of resistant pathogens like S. Dublin. By understanding the multifaceted dynamics of this pathogen, health officials can develop more targeted interventions and promote practices that enhance food safety, thereby reducing the risk of foodborne illnesses associated with this dangerous strain.
Salmonella Dublin: A Zoonotic Pathogen of Concern
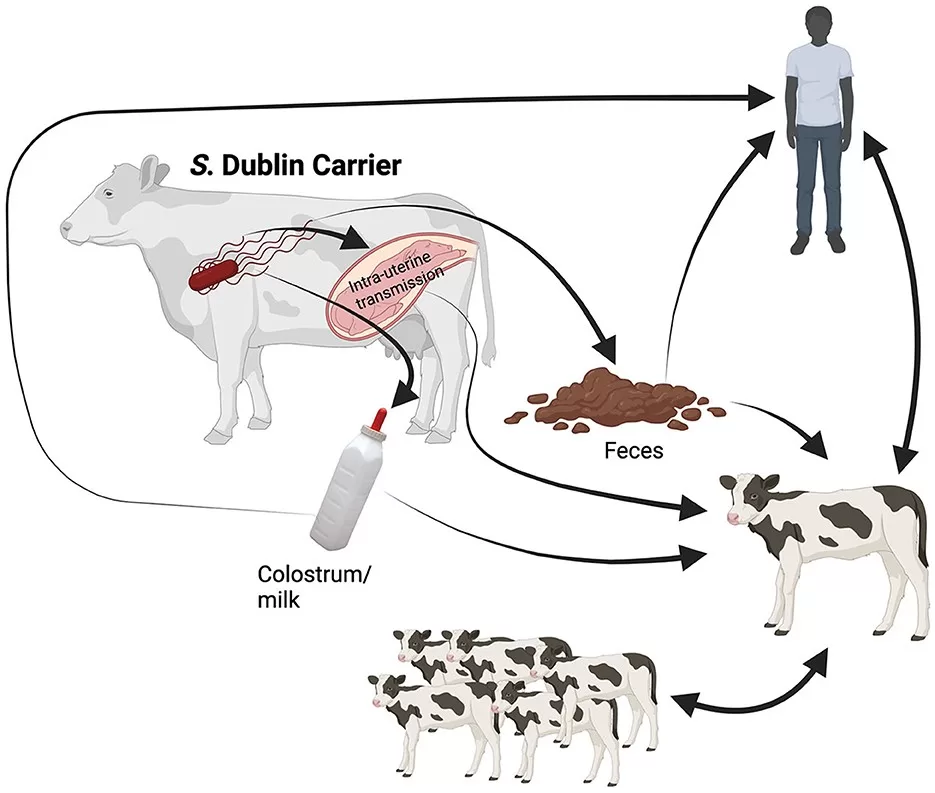
Zoonotic pathogens such as Salmonella Dublin exemplify the intricate relationship between animal health and human disease. This strain’s adaptation to cattle, specifically in dairy and beef industries, reinforces the need for vigilance in monitoring animal health and biosecurity practices. As highlighted in recent analyses, S. Dublin has been linked to severe disease outbreaks, pointing to its importance as a foodborne pathogen and emphasizing the necessity of effective control measures within cattle management operations.
Public awareness of the risks posed by zoonotic pathogens like Salmonella Dublin is equally essential for enhancing food safety protocols. As consumers increasingly demand transparency and safety in their food supply, producers must adopt best practices to safeguard against contamination. Through education and a commitment to sustainable farming practices, the beef and dairy industries can play a pivotal role in reducing the incidence of zoonotic infections, ultimately protecting both animal and human populations from potential health threats.
Cattle Health and the Rise of Salmonella Dublin
Maintaining cattle health is paramount not only for the agricultural economy but also for public health, given the role of livestock as reservoirs for pathogenic bacteria such as Salmonella Dublin. This strain poses significant challenges for veterinarians and farmers, as infections can lead to widespread morbidity in calves and increase the risk of transmission to humans through contaminated food sources. The emergence of AMR in S. Dublin underlines the need for proactive health management strategies that prioritize antibiotic stewardship in cattle farming.
Furthermore, enhancing cattle health through vaccination and biosecurity measures can diminish the prevalence of Salmonella Dublin in livestock populations. By implementing monitoring systems and routine testing for this pathogen, producers can swiftly identify and address infections, ultimately contributing to the reduction of AMR emergence. It is essential for stakeholders in the cattle industry to recognize the critical link between animal health and food safety, driving a collaborative effort towards improved practices that minimize the risks associated with this pathogen.
One Health Approach to Managing Salmonella Dublin
The One Health approach is crucial in effectively managing Salmonella Dublin due to the interconnectedness of human, animal, and environmental health. By considering all these facets, researchers and public health officials can devise comprehensive strategies that target the root drivers of Salmonella infections. The recent study from Penn State emphasizes a need for coordinated surveillance and response efforts that span various sectors, acknowledging that pathogens do not adhere to human-imposed boundaries.
As the incidence of AMR in S. Dublin increases, the One Health perspective also promotes interdisciplinary collaboration among healthcare professionals, veterinarians, and environmental scientists. This integrated approach can help ensure that interventions are holistic, addressing the multiple transmission routes of the pathogen. Additionally, it encourages shared responsibility for public health outcomes, fostering a culture of vigilance and proactive engagement in managing zoonotic diseases.
Foodborne Diseases and Salmonella Dublin Risk
Foodborne diseases remain a significant public health concern, with Salmonella Dublin being one of the notable pathogens responsible for serious illness in humans. Its association with raw milk and beef products highlights the critical need for stringent food safety measures across the food production chain. Understanding the risks associated with S. Dublin not only informs better practices for food handling and preparation but also emphasizes the importance of regulatory frameworks that protect consumers from foodborne pathogens.
The increasing prevalence of Salmonella Dublin in food systems necessitates a shift towards preventative measures rather than reactive responses. Engaging in regular inspections, promoting food safety education among consumers, and investing in research to improve pathogen detection methods are vital steps in reducing the burden of foodborne diseases. By prioritizing these initiatives, we can make significant strides in safeguarding public health against the threats posed by resistant strains like S. Dublin.
Impacts of Antimicrobial Resistance on Public Health
The rise of antimicrobial resistance (AMR) in pathogens such as Salmonella Dublin poses serious implications for public health. As traditional treatments become less effective against resistant strains, the potential for longer-lasting infections and increased healthcare costs rises sharply. This scenario underscores the need for renewed focus on antimicrobial stewardship across both human and veterinary medicine, ensuring that antibiotics are used judiciously to preserve their efficacy for future generations.
Public health strategies must prioritize the monitoring of AMR trends in zoonotic pathogens, as this knowledge directly impacts healthcare provisioning and disease prevention efforts. By understanding the factors driving resistance, including the overuse of antibiotics in agriculture, health officials can implement targeted policies that aim to reduce AMR emergence and mitigate its associated risks. Collaborative efforts among clinicians, researchers, and agricultural stakeholders will be essential in forming a cohesive front against the growing threat of antimicrobial resistance.
Strategies for Controlling Salmonella Dublin Outbreaks
Effective control of Salmonella Dublin outbreaks requires a multifaceted approach that incorporates surveillance, biosecurity measures, and public education. Implementing a robust surveillance system is key to detecting and responding to infections early, particularly in cattle populations that serve as reservoirs for the pathogen. By identifying potential outbreaks before they expand, health officials can mitigate risks to both animal and human health, ensuring food safety remains intact.
Alongside surveillance, biosecurity protocols on farms are critical in preventing the introduction and spread of Salmonella Dublin. Educating farmers about hygiene practices, appropriate use of antimicrobial applications, and regular health monitoring of cattle can significantly decrease the likelihood of infections occurring. Additionally, fostering partnerships between agricultural producers and public health agencies can enhance information exchange and streamline response efforts in the event of an outbreak.
Future Directions for Research and Policy
As the landscape of foodborne diseases evolves, ongoing research into Salmonella Dublin and other zoonotic pathogens will be vital in understanding their dynamics and developing effective interventions. Future studies should focus on exploring the mechanisms of antimicrobial resistance in S. Dublin and its transmission across different environments, which can inform policy and practice in both public health and agriculture. Innovations in testing and monitoring technologies will play an essential role in bolstering our defenses against this resilient pathogen.
Policymakers must also take proactive measures to address the growing threat of Salmonella Dublin and similar pathogens. This includes advocating for strict regulations on antibiotic use in livestock, promoting sustainable farming practices, and investing in education programs aimed at improving food safety awareness among consumers. By aligning research efforts and policy initiatives, stakeholders can collaboratively work toward a healthier future free from the burdens of foodborne diseases.
Frequently Asked Questions
What is Salmonella Dublin and why is it a concern for cattle health?
Salmonella Dublin is a zoonotic pathogen that primarily affects cattle, causing severe invasive infections, particularly in calves. It is the most commonly isolated Salmonella serovar from clinical cases in cattle, leading to significant health issues and economic losses in the livestock industry.
How does antimicrobial resistance impact Salmonella Dublin infections in humans?
The increasing antimicrobial resistance (AMR) in Salmonella Dublin is concerning as it leads to more severe infections in humans, often associated with foodborne diseases transmitted through contaminated raw milk and meat products. This resistance complicates treatment and poses a serious public health threat.
What does the One Health approach entail in managing Salmonella Dublin?
The One Health approach in managing Salmonella Dublin involves a comprehensive strategy that considers the interconnections between human, animal, and environmental health. This integrative method is essential for effective surveillance and control of S. Dublin, particularly given its prevalence in cattle and potential to impact human health.
What are the main sources of Salmonella Dublin outbreaks associated with foodborne diseases?
Salmonella Dublin outbreaks have been primarily linked to the consumption of raw milk, soft cheese, and beef. Due to its adaptation to cattle, food products from infected animals pose a heightened risk for foodborne diseases related to this pathogen.
Why is continuous biosurveillance important for Salmonella Dublin?
Continuous biosurveillance of Salmonella Dublin is vital to monitor its evolution and resistance patterns. Understanding how this pathogen spreads between cattle and humans, along with its environmental dynamics, is crucial for developing effective control measures and ensuring food security.
What role do cattle play in the transmission of Salmonella Dublin to humans?
Cattle serve as a primary reservoir for Salmonella Dublin, and transmission to humans can occur through contaminated food products. The interconnectedness of food systems highlights the importance of managing cattle health to mitigate risks posed by this antimicrobial-resistant zoonotic pathogen.
What are the challenges in combating Salmonella Dublin’s antimicrobial resistance?
The challenges in combating Salmonella Dublin’s antimicrobial resistance include the high prevalence of resistance genes in cattle strains, the complex interactions within the One Health framework, and the need for coordinated antimicrobial stewardship practices among human and veterinary sectors to reduce resistance and protect public health.
How does Salmonella Dublin compare to other Salmonella serotypes?
Salmonella Dublin is known for causing more severe infections compared to other Salmonella serotypes. Its adaptation to cattle and rising antimicrobial resistance levels make it particularly concerning for both cattle health and foodborne disease outbreaks in humans.
| Key Points | Details |
|---|---|
| Research Findings | Study analyzed over 2,000 samples of Salmonella Dublin from humans, cattle, and the environment between 2002 – 2023. |
| Impact on Cattle | S. Dublin is the most common serovar in cattle, causing severe infections and is linked to outbreaks from raw milk, soft cheese, and beef. |
| Antimicrobial Resistance | Rising levels of AMR in both cattle and human infections, posing a threat to health and food security. |
| Need for One Health Approach | A comprehensive approach is essential to understand and manage S. Dublin across all reservoirs (humans, animals, and the environment). |
| Genomic Analysis | Cattle strains exhibit the highest prevalence of resistance genes and plasmids, indicating greater diversity compared to human strains. |
| Cross-Transmission | High genomic similarity across sources suggests interconnectedness, necessitating cross-sector control efforts. |
| Antimicrobial Stewardship | Cattle accounted for a significant portion of antibiotic sales in the U.S. in 2023, highlighting the need for responsible use. |
Summary
Salmonella Dublin presents a crucial challenge in public health as an increasingly antimicrobial-resistant zoonotic pathogen. This multifaceted organism poses significant risks to both human and cattle health, emphasizing the need for comprehensive management strategies. Ongoing research illustrates the pathogen’s evolution and interconnectedness across various reservoirs, highlighting the importance of adopting a One Health approach to effectively reduce its impact on food safety and health systems.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.