Neisseria meningitidis urethritis is emerging as a significant public health concern, particularly in Bangkok, Thailand, where reports from STD clinics indicate a troubling rise in cases from 2017 to 2023. This rise corresponds with the global expansion of the antimicrobial-resistant clonal complex 11 (CC11) strain of N. meningitidis, known for its potential to cause urethral infections. Surveillance efforts have become increasingly crucial as this clonal group has exhibited capabilities for asymptomatic colonization, complicating prevention and treatment strategies. With antimicrobial resistance posing a growing challenge, understanding the dynamics of this urethritis cluster is essential for effective public health responses. As researchers focus on unraveling the complexities of N. meningitidis, the need for coordinated monitoring and intervention strategies becomes ever more pressing in combating this urethral infection crisis.
Urethritis caused by Neisseria meningitidis, often referred to simply as N. meningitidis, has recently gained attention due to its association with increasing cases of antimicrobial resistance, particularly within specific clonal groups like clonal complex 11 (CC11). This condition, typically linked to sexually transmitted diseases, has been notably prevalent in regions like Bangkok, highlighting a distinct urethritis cluster detrimental to public health. Identifying and understanding this strain’s dissemination is vital for effective intervention strategies against urethral infections. As the landscape of antimicrobial resistance evolves, the focus on STD clinics and their surveillance efforts becomes critical in managing these outbreaks. Researchers are now tasked with developing comprehensive monitoring systems to address the complexities within this urethritis context.
Overview of Neisseria meningitidis Urethritis
Neisseria meningitidis is primarily recognized for causing severe conditions such as meningitis and septicemia. However, recent findings have spotlighted its role in urethritis, especially in regions such as Bangkok, Thailand. The rise in cases between 2017 and 2023 has led to increased attention toward this pathogen’s adaptation and resilience in clinical environments. This emerging trend suggests that healthcare providers need to be vigilant in recognizing urethritis caused by N. meningitidis, which has typically been overlooked in favor of more traditional sexually transmitted diseases.
Urethritis caused by N. meningitidis presents unique challenges, not only due to its clinical presentation but also because of its association with antimicrobial resistance. As reported cases escalate, it is essential for STD clinics in Bangkok to adopt comprehensive screening practices to effectively identify and manage N. meningitidis urethritis. Awareness raising among healthcare workers about this condition will help mitigate the risk of further outbreaks and will facilitate timely and appropriate treatments.
Antimicrobial Resistance in Neisseria meningitidis
The emergence of antimicrobial-resistant strains of Neisseria meningitidis, particularly the clonal complex 11 (CC11), raises significant concerns for public health. During the study period, numerous isolates demonstrated resistance to commonly used antibiotics, complicating treatment regimens. Specifically, increased resistance to ciprofloxacin has been noted, prompting a reevaluation of standard therapeutic approaches for managing infections caused by this organism.
The phenomenon of antimicrobial resistance in N. meningitidis underscores a broader issue seen in many infectious pathogens: the ability to adapt and survive in the face of antibiotic pressure. Ongoing surveillance and genomic analysis are necessary to track the evolution of resistance patterns, particularly in high-risk populations such as men attending STD clinics in Bangkok. The data collected can contribute to developing new treatment guidelines that effectively address these resistance trends while ensuring patient care remains robust.
Urethritis Cluster Trends in Thailand
The emergence of a urethritis cluster linked to Neisseria meningitidis in Thailand is a phenomenon requiring urgent public health response. Between 2017 and 2023, STD clinics in Bangkok observed a notably high prevalence of this infection, particularly among men, which raises questions about transmission dynamics and social factors influencing these trends. Studies indicate that ongoing surveillance efforts must include the monitoring of sexual behavior patterns that contribute to the spread of urethritis in this demographic.
In addition to improving disease surveillance, health authorities need to focus on education and prevention strategies that inform the public about the risks associated with untreated urethritis caused by N. meningitidis. This knowledge can empower individuals to seek timely medical attention and encourage responsible sexual practices. By addressing both the clinical and societal aspects of this cluster, we can better manage the impact of urethritis in Thailand.
Genomic Analysis of N. meningitidis Urethritis
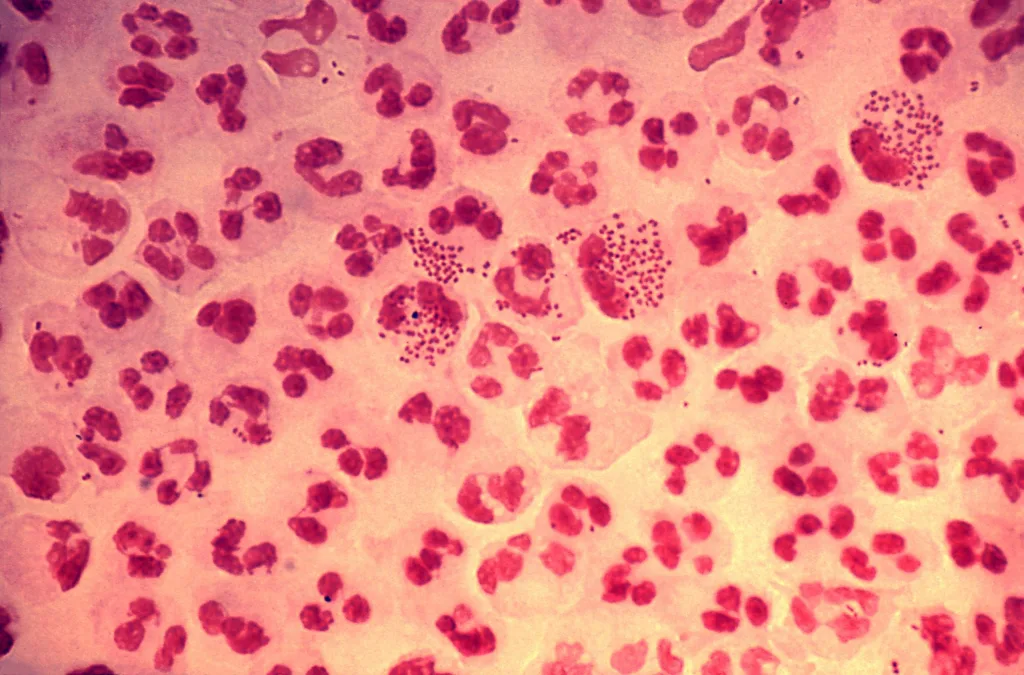
Genomic analyses are pivotal in understanding the clonal structure and evolution of Neisseria meningitidis within the urethritis context. The study showcased an alarming expansion of the non-groupable clonal complex 11, revealing its potential to adapt and spread within various populations. This genetic tracking not only provides insights into the pathogen’s behavior but also assists in identifying risk factors associated with certain clonal lineages.
Implementing genomic insights in clinical practices can significantly enhance the ability to predict outbreaks and manage infections effectively. By developing a comprehensive database of N. meningitidis genomic sequences linked to urethritis, healthcare practitioners can correlate specific strains with resistance profiles, leading to more effective treatment regimens. Continuous efforts in genomic research are essential to combat antimicrobial resistance and promote better public health outcomes.
Clinical Implications for STD Clinics in Bangkok
The recent rise in Neisseria meningitidis-associated urethritis has significant clinical implications for STD clinics in Bangkok. Healthcare providers need to remain vigilant and incorporate the potential for N. meningitidis into their differential diagnoses for urethritis. With cases rising, especially among men, ensuring that clinics are equipped with the latest evidence and treatment protocols is critical in managing this emerging health threat.
Additionally, it is imperative for STD clinics to engage in collaboration with public health authorities to enhance awareness and training among staff about N. meningitidis and its associated conditions. Regular updates on treatment guidelines and resistance patterns can ensure that clinics offer effective care while managing the risk of transmission within the community. The integration of clinical knowledge with patient education will pave the way for better management strategies against urethritis in Thailand.
Public Health Strategies Against N. meningitidis Urethritis
Mitigating the spread of Neisseria meningitidis-associated urethritis in Thailand requires multifaceted public health strategies. These should encompass routine screening in populations at increased risk, such as men visiting STD clinics, along with improved accessibility to testing and treatment. Furthermore, establishing partnerships with local health organizations can facilitate targeted outreach programs that inform at-risk demographics about the symptoms and consequences of urethritis.
Education plays a crucial role in reducing the stigma surrounding sexually transmitted infections, which often deters individuals from seeking help. Public health campaigns should focus on destigmatizing urethritis caused by N. meningitidis, promoting safer sexual practices, and encouraging routine testing. These efforts, combined with a robust surveillance system to monitor infection trends and resistance patterns, will enhance efforts to control the spread of this disease in Bangkok and beyond.
Future Directions in N. meningitidis Research
Research into Neisseria meningitidis, particularly its role in urethritis and antimicrobial resistance, is increasingly critical. Future studies should prioritize understanding the genetic basis of resistance in clonal complex 11 strains and their mechanisms of pathogenicity. Insights gained will not only inform clinical practices but also foster the development of novel therapeutic approaches aimed at improving outcomes for affected individuals.
Moreover, collaborative research initiatives that include a variety of stakeholders—from academic institutions to public health bodies—will be essential in developing comprehensive strategies to combat N. meningitidis urethritis. Establishing biobanks for N. meningitidis isolates, coupled with extensive epidemiological studies, can provide a wealth of data that informs future interventions and policies, ensuring better preparedness against this evolving public health challenge.
The Role of Antimicrobial Surveillance in Urethritis Management
Ongoing antimicrobial surveillance forms a crucial backbone in effectively managing Neisseria meningitidis urethritis. By routinely monitoring resistance patterns among pathogens in clinical settings, healthcare providers can adapt treatment protocols to avoid the pitfalls associated with ineffective therapies. This proactive approach is essential in not only containing existing cases but also in preventing future outbreaks within communities.
Furthermore, integrating surveillance findings into clinical education and training ensures that healthcare providers are aware of the most effective treatment options available. Regular updates regarding emerging resistance trends, particularly for clonal complex 11 strains, will enhance the ability to tailor interventions appropriately and improve patient outcomes in STD clinics across Bangkok and similar environments.
Educational Initiatives for Healthcare Providers and Communities
Implementing robust educational initiatives targeting both healthcare providers and the community is essential in combating the rise of Neisseria meningitidis-associated urethritis. For healthcare professionals, increased training on identifying symptoms, understanding resistance patterns, and employing effective treatment strategies can substantially enhance clinical responses to urogenital infections. Workshops, seminars, and continuing education courses should be utilized to equip providers with up-to-date information on the pathogen and its implications.
Equally important is fostering awareness in the general community about the symptoms and risk factors associated with urethritis. Public health campaigns that inform individuals, particularly those frequenting STD clinics, about safe practices, testing availability, and treatment options can lead to earlier interventions. By creating an informed public, the rates of infection can potentially decrease, leading to healthier communities.
Frequently Asked Questions
What is Neisseria meningitidis urethritis and how is it related to antimicrobial resistance?
Neisseria meningitidis urethritis is an infection of the urethra caused by the bacterium Neisseria meningitidis. This organism is particularly concerning due to its emerging strains of antimicrobial-resistant clonal complex 11, which have been identified in clusters, such as those in Thailand. These resistant strains complicate treatment options and necessitate careful monitoring in affected populations.
How has the clonal complex 11 Neisseria meningitidis impacted urethritis cases in Thailand?
The clonal complex 11 Neisseria meningitidis has significantly impacted urethritis cases in Thailand, especially from 2017 to 2023. An increase in infections linked to this complex was documented in STD clinics in Bangkok, where genomic studies revealed resistance patterns, particularly towards antibiotics like ciprofloxacin, emphasizing the necessity for ongoing surveillance.
What are the current treatment challenges for Neisseria meningitidis urethritis in STD clinics in Bangkok?
Current treatment challenges for Neisseria meningitidis urethritis in Bangkok’s STD clinics include the emergence of strains resistant to common antibiotics. While ceftriaxone remains effective against the majority of isolates, resistance to other treatments, such as ciprofloxacin among clonal complex 11 strains, poses a risk for treatment failure and highlights the need for tailored therapeutic approaches.
What public health measures are recommended for monitoring Neisseria meningitidis urethritis infections?
Recommended public health measures for monitoring Neisseria meningitidis urethritis infections include enhanced surveillance in high-prevalence areas like Thailand, genomic tracking of clonal complex 11 strains, and routine screening in STD clinics. This approach aims to quickly identify antimicrobial resistance patterns and adapt treatment guidelines accordingly.
What factors contribute to the asymptomatic colonization of Neisseria meningitidis in the population?
Approximately 10% of the population may experience asymptomatic colonization of Neisseria meningitidis, which can be attributed to its ability to exist in the host without causing symptoms. Factors such as genetic predispositions, immune response variations, and environmental conditions can facilitate this asymptomatic presence, posing challenges for early detection and treatment.
| Key Point | Details |
|---|---|
| Rising Cases | Increased incidences of Neisseria meningitidis-associated urethritis reported in Bangkok between 2017 to 2023. |
| Genomic Analysis | The non-groupable clonal complex 11 (CC11) lineage has shown global expansion and linkage to previous outbreaks. |
| Antimicrobial Resistance | Resistance identified particularly to ciprofloxacin; all isolates effectively treated with ceftriaxone. |
| Public Health Implications | Ongoing surveillance is crucial for monitoring antimicrobial-resistant strains and preventing outbreaks. |
Summary
Neisseria meningitidis urethritis has emerged as a significant public health concern, particularly in Bangkok, where cases have increased from 2017 to 2023. The discovery of antimicrobial-resistant strains highlights the need for effective treatment and thorough surveillance to contain these infections. As antimicrobial resistance continues to evolve, it is essential for health authorities to adapt and monitor treatment protocols, ensuring positive health outcomes.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.