Extended-Spectrum β-lactamase Klebsiella pneumoniae has emerged as a significant public health concern due to its robust antibiotic resistance capabilities. This opportunistic pathogen, often found in healthcare settings, poses a serious risk not only in hospitals but also within the food supply, as indicated by recent findings in Switzerland. The presence of ESBL Klebsiella pneumoniae in both human clinical samples and food raises alarming questions about food safety in Switzerland, suggesting that everyday consumer products could harbor this dangerous bacterium. The World Health Organization has recognized ESBL-producing Klebsiella pneumoniae as a critical priority, emphasizing the urgent need for enhanced surveillance and control measures. As we delve deeper into the genetic clusters and transmission routes, understanding the implications of antibiotic resistance becomes crucial for safeguarding public health against emerging threats.
The emergence of ESBL-producing strains such as Klebsiella pneumoniae highlights an urgent global health challenge marked by increased antibiotic resistance. This bacteria, which can rain havoc in medical settings and potentially contaminate food sources, is fueling concern among health professionals and researchers alike. Under various names, including Klebsiella pneumoniae risk and ESBL Klebsiella pneumoniae, these pathogens are highlighting vulnerabilities within our healthcare and food systems. With their ability to resist conventional treatments, the implications for public health are profound, prompting critical discussions around food safety Switzerland and the necessary safeguards to mitigate such public health hazards. As we analyze these trends, the intersection of human health, environmental factors, and effective management strategies needs to be prioritized to combat the spread of resistant bacteria.
Understanding Extended-Spectrum β-lactamase Klebsiella pneumoniae
Extended-Spectrum β-lactamase (ESBL) Klebsiella pneumoniae represents a significant challenge in the field of infectious diseases due to its antibiotic resistance. This strain of bacteria is able to produce enzymes that dismantle commonly used beta-lactam antibiotics, rendering them ineffective. The emergence of ESBL-producing strains can be attributed to various factors including selective pressure from antibiotic overuse, which has escalated their prevalence in both human healthcare settings and the food supply chain. In particular, the genetic cluster of ESBL Klebsiella pneumoniae observed in Switzerland highlights the urgent need for surveillance and effective control measures to curb its spread across different environments, from hospitals to agricultural sectors.
The public health implications of Extended-Spectrum β-lactamase Klebsiella pneumoniae cannot be overstated. Infections caused by these bacteria often lead to prolonged hospital stays, increased medical costs, and, in some cases, heightened mortality rates due to treatment failure. Moreover, this situation poses a significant risk not only to patients who are already vulnerable but also to public health at large, as these resistant strains can spread quickly through contaminated food sources and the environment, demanding urgent attention from healthcare authorities.
In recent years, the focus on screening methodologies has gained traction given the emergence of genetic clusters of ESBL-producing Klebsiella pneumoniae in diverse reservoirs such as food samples. This indicates an alarming trend where food sources may act as reservoirs for bacteria capable of causing serious infections. The research conducted in Basel, Switzerland, elucidates this interconnectedness and underscores the need for enhanced food safety regulations, particularly in the harvesting and processing segments to minimize contamination risks. Safe food handling practices are crucial in preventing the transmission of resistant bacteria like K. pneumoniae from food to humans.
To comprehensively tackle the public health threats posed by ESBL Klebsiella pneumoniae, an integrated approach that encompasses clinical vigilance, robust food safety protocols, and thorough microbiological assessments is paramount. Continuous monitoring and, ideally, a strict regulatory framework can help mitigate these risks, ensuring that both patients and the broader population can be safeguarded against the threats of antibiotic resistance.
The Role of Food Safety in Controlling Klebsiella pneumoniae Risks
Food safety plays a pivotal role in controlling the risks associated with Klebsiella pneumoniae, especially in the context of antibiotic-resistant strains like those producing ESBL. The findings from the Basel study indicate that contaminated food, particularly items like alfalfa-cress, can act as conduits for these resistant bacteria, enabling their transmission into the human population. This situation calls for a concerted effort from food safety authorities, producers, and consumers alike to uphold stringent hygiene standards throughout the food supply chain. Enhanced practices such as regular microbial testing and improved sanitation can significantly reduce the risk of ESBL-producing Klebsiella pneumoniae infiltrating the food system.
Furthermore, educating food handlers and consumers about the dangers of cross-contamination and the importance of cooking food thoroughly can diminish the likelihood of transmission. Public awareness campaigns highlighting the significance of food safety in mitigating the spread of antibiotic-resistant bacteria are essential. As part of this, guidelines should be drawn up for food establishments and home kitchens alike to ensure that food products are safe for consumption, especially in regions noted for high prevalence of such pathogens.
In addition to preventive measures, the role of governmental and non-governmental organizations in promoting food safety cannot be overlooked. Regulatory frameworks must be established to monitor the prevalence of antibiotic-resistant bacteria in food products and to enforce compliance with safety standards. This comprehensive oversight can aid in identifying points of failure in food safety practices, facilitating timely interventions to prevent outbreaks of infections caused by ESBL Klebsiella pneumoniae.
By focusing on food safety as a critical factor in managing Klebsiella pneumoniae risks, communities can proactively address the public health hazards posed by antibiotic resistance. Through collaboration among healthcare providers, food safety regulators, and the public, it is possible to create a multifaceted approach that not only prevents contamination but also promotes healthier environments for all.
Public Health Hazards of Antibiotic Resistance
The rise of antibiotic resistance has emerged as one of the most pressing public health hazards of the 21st century, with Extended-Spectrum β-lactamase Klebsiella pneumoniae being a prime example. As bacteria evolve to withstand commonly used antibiotics, the treatment landscape for various infections becomes increasingly complex and fraught with risks. The widespread presence of antibiotics in agriculture, coupled with their over-prescription in clinical settings, contributes to this alarming trend. Awareness of antibiotic resistance among healthcare professionals and the public is critical for fostering responsible antibiotic use and reducing further resistance development.
The implications are severe; patients infected with antibiotic-resistant strains often experience prolonged illnesses and may require more expensive, complex treatments that may not guarantee recovery. The economic burden on healthcare systems, coupled with the potential for increased mortality associated with these infections, underscores the necessity for robust public health strategies focused on monitoring and mitigating the spread of resistant organisms such as ESBL Klebsiella pneumoniae.
In response to the growing threat of antibiotic resistance, several global health initiatives have been launched aimed at curbing its spread. The World Health Organization has prioritized efforts to tackle antibiotic resistance, particularly in bacteria that pose a significant threat to public health like Klebsiella pneumoniae. These initiatives emphasize the importance of global cooperation, the development of new antibiotics, advanced diagnostic techniques, and greater adherence to infection prevention protocols in healthcare environments.
In Switzerland, the findings of the 2018-2019 study on ESBL Klebsiella pneumoniae highlight how interconnected human health and food safety are in addressing antibiotic resistance. A collaborative approach that involves healthcare providers, food safety experts, and public health officials is essential to unraveling the complexities of antibiotic resistance and implementing effective countermeasures, thereby protecting the health of both individuals and communities.
Monitoring and Surveillance of ESBL-Producing Klebsiella pneumoniae
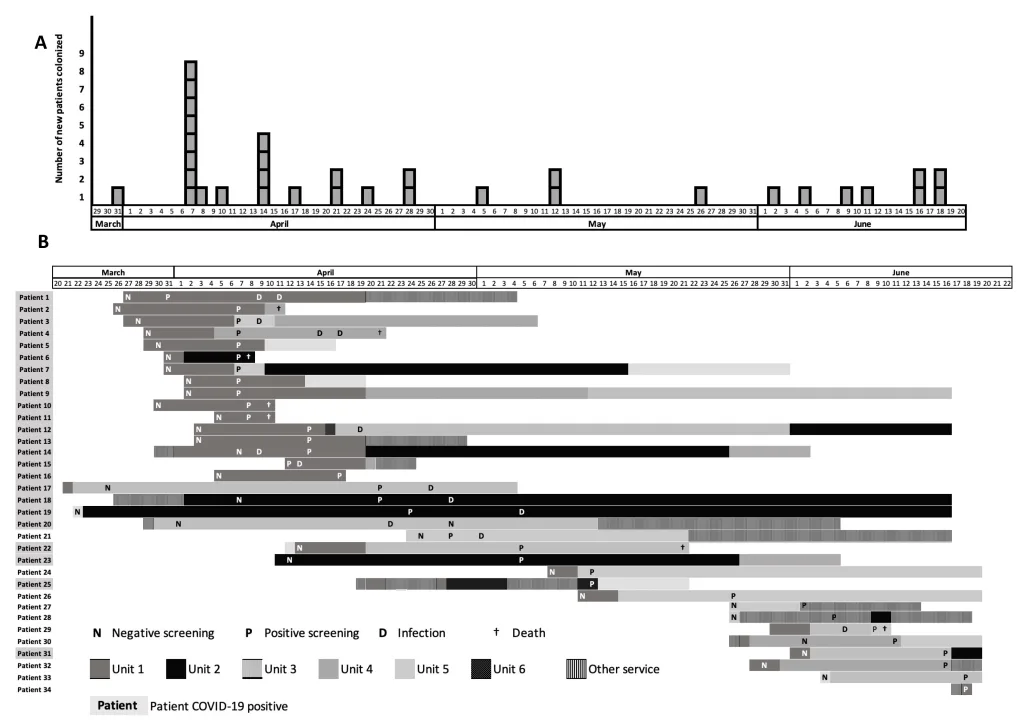
Monitoring and surveillance are crucial components in the fight against infections caused by ESBL-producing Klebsiella pneumoniae. Continuous tracking of these bacteria across various environments, including healthcare facilities and food sources, enables health authorities to understand transmission dynamics and identify potential outbreak sources. The study conducted in Basel, Switzerland, illustrates the relevance of integrating food safety and clinical surveillance to paint a comprehensive picture of the spread of these resistant organisms. Regular sampling and genomic analyses can uncover critical insights regarding the genetic makeup of ESBL Klebsiella pneumoniae, helping to inform prevention strategies and response plans.
Moreover, establishing robust surveillance systems can facilitate effective communication among different sectors, including agriculture, food safety, and public health. This integrated approach not only helps in detecting and controlling outbreaks but also aids in developing informed policies that can reduce the incidence of infections caused by antibiotic-resistant bacteria. By prioritizing monitoring efforts at all levels, communities can enhance their preparedness and responsiveness to the challenges posed by ESBL-producing Klebsiella pneumoniae.
In addition to traditional surveillance methods, innovative technologies such as whole-genome sequencing are proving invaluable in understanding the evolution and spread of antibiotic resistance. With the ability to analyze bacterial genomes, researchers can track mutations, assess virulence factors, and determine transmission paths more effectively than ever before. This data-driven approach allows for quicker response times to outbreaks and can inform targeted interventions, including the development of vaccines and novel therapeutic strategies against resistant strains.
As antibiotic resistance continues to evolve, the implementation of effective monitoring and surveillance systems will remain a cornerstone of public health efforts. Ensuring that robust frameworks are in place not only protects public health but also plays a pivotal role in shaping future research and clinical practices addressing the ongoing challenges posed by ESBL-producing Klebsiella pneumoniae.
The Importance of Hygiene Practices in Food Handling
Hygiene practices in food handling are critical in the battle against the spread of antibiotic-resistant bacteria, particularly Extended-Spectrum β-lactamase Klebsiella pneumoniae. The findings of the Basel study emphasize that improper food handling can lead to the spread of these resistant organisms from food to humans, underscoring the need for improved hygiene protocols in agricultural and culinary operations. Basic practices such as thorough washing of hands, proper sanitation of kitchen tools, and careful cooking of food can significantly mitigate the risk of bacterial contamination. Training food handlers on these practices is essential to ensure adherence and promote a culture of food safety within communities.
Furthermore, the implementation of Hazard Analysis and Critical Control Points (HACCP) systems in food processing environments can enhance the safety of food products. By identifying points of contamination and establishing critical control measures, such systems help in monitoring food safety more proactively. Making hygiene a priority at all levels of food production and preparation can dramatically reduce the chances of Extended-Spectrum β-lactamase producing bacteria entering the food chain.
In addition to enforcing hygiene practices among food handlers, it’s equally important to educate consumers about safe food preparation at home. Public awareness campaigns aimed at teaching proper food storage techniques, cooking temperatures, and cross-contamination prevention can empower consumers to take ownership of food safety. Additionally, consumers should be encouraged to stay informed about foodborne pathogens and antibiotic resistance, as this knowledge will contribute to their role in preventing the spread of ESBL Klebsiella pneumoniae. Creating a food safety-conscious society is vital in reducing public health hazards related to antibiotic resistance, ensuring a healthier future for everyone.
Frequently Asked Questions
What is Extended-Spectrum β-lactamase Klebsiella pneumoniae and why is it important?
Extended-Spectrum β-lactamase (ESBL) Klebsiella pneumoniae refers to a type of bacteria that produces enzymes capable of breaking down commonly used antibiotics, thereby leading to antibiotic resistance. This strain has been classified by the World Health Organization as a critical public health priority due to its increasing prevalence in both healthcare and community settings.
How do ESBL Klebsiella pneumoniae infections affect public health?
ESBL Klebsiella pneumoniae poses significant public health hazards as it can lead to severe infections that are difficult to treat. The emergence of antibiotic resistance complicates treatment options, increasing hospitalization rates and mortality, especially among vulnerable populations.
What are the risks associated with Klebsiella pneumoniae in food safety in Switzerland?
Food safety risks associated with Klebsiella pneumoniae stem from its potential presence in food products, which can act as reservoirs for ESBL-producing bacteria. In Switzerland, studies have shown that contaminated food items, such as alfalfa-cress, can transmit these pathogens to humans, necessitating stringent food safety measures.
What strategies can reduce the spread of antibiotic-resistant Klebsiella pneumoniae?
To reduce the spread of antibiotic-resistant Klebsiella pneumoniae, it is crucial to implement strict hygiene practices in food handling, improve antibiotic stewardship in healthcare settings, and conduct regular surveillance of both human and food samples to monitor and control its prevalence.
How did the research conducted in Basel contribute to understanding ESBL Klebsiella pneumoniae?
The prospective study in Basel collected food and wastewater samples to investigate the epidemiology of ESBL Klebsiella pneumoniae. By employing advanced genomic techniques, researchers identified genetic clusters indicating transmission routes, therefore providing valuable insights into how food may contribute to the spread of antibiotic-resistant bacteria.
What measures are being taken internationally to combat ESBL Klebsiella pneumoniae?
Internationally, public health organizations, including the WHO, are working to combat ESBL Klebsiella pneumoniae through enhanced surveillance, stricter regulations on antibiotic usage in both humans and agriculture, and public education initiatives aimed at reducing the risk of transmission from food and the environment.
| Category | Details |
|---|---|
| Title | Genetic Cluster of Extended-Spectrum β-lactamase–Producing Klebsiella pneumoniae in Humans and Food, Switzerland, 2018–2019 |
| Abstract | The study identifies a genetic cluster of ESBL-producing Klebsiella pneumoniae in humans and food, suggesting food may contribute to its spread in Switzerland. |
| Study Objective | To investigate the epidemiology of ESBL-producing Enterobacterales in Basel, focusing on genetic relationships from food and clinical samples. |
| Methodology | Prospective study, monthly collection of food and wastewater samples, genome sequencing, and multilocus sequence typing used to analyze genetic relatedness. |
| Findings | 12 out of 947 food isolates were confirmed as K. pneumoniae with ESBL capabilities. Phylogenetic analysis identified a cluster indicating environmental transmission to humans. |
| Public Health Importance | ESBL-producing Klebsiella pneumoniae is a critical public health threat according to WHO since 2017, necessitating stricter food hygiene practices. |
Summary
Extended-Spectrum β-lactamase Klebsiella pneumoniae poses a significant public health risk due to its potential transmission from food sources to humans. The study conducted in Switzerland highlights the alarming prevalence of genetically related ESBL-producing Klebsiella pneumoniae in both clinical and food samples. Ensuring stringent hygiene protocols in food handling is essential to mitigate the spread of these resistant bacteria, reinforcing the need for ongoing monitoring and public awareness initiatives.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.