Extensively Drug-Resistant Neisseria gonorrhoeae has emerged as a dire public health concern, particularly in Canada, where recent reports reveal troubling rates of resistance to conventional treatments. This strain of gonorrhea, characterized by ceftriaxone and azithromycin resistance, signifies a critical moment in the fight against sexually transmitted infections (STIs). Public health data indicates that gonorrhea cases have surged dramatically, underscoring the urgent need for effective gonorrhea treatment protocols in Canada. With the World Health Organization categorizing these resistant strains as bacterial priority pathogens, health authorities are pressed to address the challenges posed by XDR N. gonorrhoeae. As resistance levels rise, understanding the implications and finding alternative treatments becomes crucial to public health management.
The alarming rise of extensively drug-resistant strains of gonorrhea, particularly seen in cases like XDR N. gonorrhoeae, highlights an escalating threat in the realm of infectious diseases. Known for its resistance to vital antibiotics such as ceftriaxone and azithromycin, this variant poses significant challenges for health professionals aiming to manage and treat gonorrhea infections effectively. As reports of ceftriaxone resistance become more common, it raises critical questions about current gonorrhea treatment options in Canada and the broader implications for sexually transmitted infections. This situation emphasizes the importance of vigilance in monitoring and addressing the emergence of high-level resistant pathogens. Effectively combating this public health issue will require collaboration among healthcare providers, researchers, and policymakers to identify innovative treatment strategies and bolster surveillance efforts against such resistant strains.
Understanding Extensively Drug-Resistant Neisseria gonorrhoeae
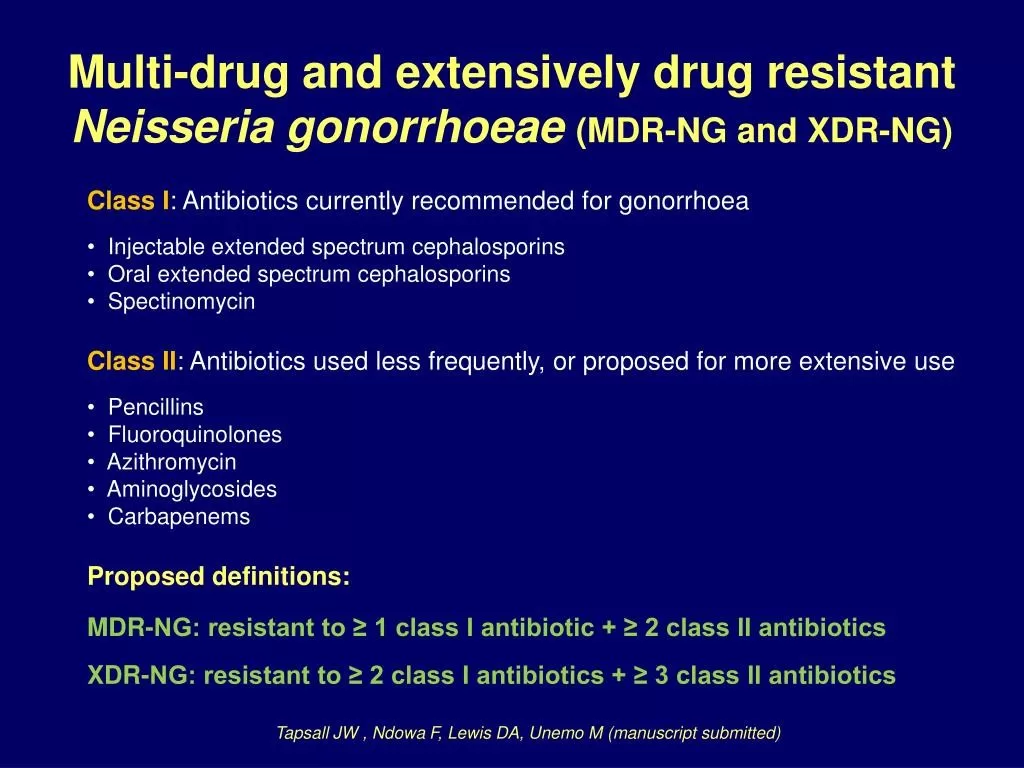
Extensively drug-resistant (XDR) Neisseria gonorrhoeae presents a significant public health challenge, particularly in Canada where cases have surged due to rising antibiotic resistance. This strain of gonorrhea is characterized by its resistance to ceftriaxone, cefixime, and high-level azithromycin, rendering conventional treatments ineffective. The identification of such strains emphasizes the need for urgent updates to therapeutic guidelines and the adoption of alternative treatment strategies in response to this growing resistance.
The XDR N. gonorrhoeae strain isolated from a patient highlights the importance of understanding the genetics behind antibiotic resistance. The penA 60.001 allele linked to ceftriaxone resistance, as well as the A311V and 23S rRNA A2059G mutations associated with azithromycin resistance, are critical factors that healthcare providers must consider when treating infected individuals. As resistance patterns evolve, clinicians must stay informed about the latest research to effectively address and control gonorrhea outbreaks.
The Rise of Gonorrhea Treatment Challenges in Canada
In Canada, the rise in gonorrhea cases—reported at 92.34 per 100,000 in 2022—correlates with the increasing emergence of strains resistant to first-line treatments. The significant 146.2% increase since 2010 serves as a warning signal regarding the challenges faced by health authorities in clinical management. Healthcare professionals are now constantly adapting their practice to address treatment failures caused by strains of N. gonorrhoeae that exhibit novel antibiotic resistance mechanisms.
One key aspect of treating gonorrhea in Canada involves understanding the roles of different antibiotics and their current efficacy against resistant strains. Ceftriaxone has long been considered a cornerstone in gonorrhea treatment; however, the growing incidence of ceftriaxone resistance necessitates the exploration of alternative therapeutic options. Comprehensive strategies that include continuous surveillance of antibiotic resistance patterns are essential in mitigating treatment challenges and preventing further public health crises.
Bacterial Priority Pathogens and Gonorrhea
The World Health Organization designates extensively drug-resistant Neisseria gonorrhoeae as a high priority on the Bacterial Priority Pathogens List for good reason: its potential to cause considerable morbidity and complicate public health efforts. As resistance to third-generation cephalosporins like ceftriaxone intensifies, healthcare systems globally face the dire possibility of untreatable gonorrhea, which necessitates immediate action on multiple fronts, including research, policy reform, and improved patient education.
By addressing the threat posed by bacterial priority pathogens such as XDR N. gonorrhoeae, public health officials can enhance their response frameworks for sexually transmitted infections. Focusing on prevention, promoting safe sexual practices, and increasing access to early detection and treatment through STI screening are critical components of any strategy aimed at combating these resistant strains effectively.
Treatment Protocol Adjustments for Gonorrhea
The treatment of gonorrhea in Canada has undergone significant changes due to the emergence of drug-resistant strains. The case of a patient treated unsuccessfully with standard therapies underscores the need for healthcare providers to rethink treatment protocols continually. The adjustments include not only higher doses of ceftriaxone but also potential combinations with other antibiotics to maximize treatment effectiveness against extensively drug-resistant N. gonorrhoeae.
Such treatment protocol changes call for enhanced healthcare professional training to ensure that they are equipped with the knowledge to identify resistant strains promptly. Additionally, the incorporation of recent research findings into clinical guidelines can facilitate timely and effective treatment interventions, significantly impacting patient outcomes and curbing the further spread of resistant infections.
Surveillance and Public Health Response to Gonorrhea
Continuous surveillance of antimicrobial resistance is crucial in managing the threat posed by strains like XDR N. gonorrhoeae. Public health agencies must implement robust monitoring systems to track resistance patterns, ensuring that healthcare providers have access to the most current data to inform treatment decisions. This can help identify emerging trends in resistance and allow for proactive educational campaigns targeting at-risk populations.
Moreover, understanding local epidemiology helps tailor interventions for at-risk communities, fostering collaborative efforts among healthcare providers, public health authorities, and patient advocacy groups. Enhancing awareness and response mechanisms ensures that appropriate measures are in place to address future outbreaks effectively and minimize treatment failures.
Travel-Related Gonorrhea Infections
Travel-related infections present a significant concern when it comes to the management of gonorrhea. As demonstrated by the case of the patient who contracted extensively drug-resistant N. gonorrhoeae while traveling in Cambodia, the risk of exposure to antibiotic-resistant strains is an emerging trend that healthcare providers cannot ignore. Global travel has made the spread of resistant bacteria easier, necessitating that clinicians inquire about patients’ travel histories during consultations.
To mitigate the risk of importation of drug-resistant gonorrhea strains, effective travel health advisories and patient education before departure are paramount. Health professionals should emphasize the importance of safer sexual practices while traveling and encourage individuals to seek STI testing upon their return, enhancing the early detection and treatment of potentially resistant infections.
Handling Treatment Failures in Gonorrhea Cases
Addressing treatment failures in gonorrhea cases involves a multi-faceted approach that emphasizes timely identification and management of resistant strains. As seen with the case of the Canadian patient treated unsuccessfully with cefixime and azithromycin, implementing second-line agents and backup treatments is critical for managing resistant infections. In instances where initial therapies fail, clinicians must be prepared to adapt quickly, as was done with the subsequent administration of a higher dose of ceftriaxone.
Improving communication between healthcare providers regarding treatment outcomes and resistance profiles can enhance collective knowledge and interventions. Ensuring that healthcare systems share best practices for handling treatment failures fosters resilience against rapidly emerging antibiotic-resistant pathogens and contributes to comprehensive public health strategies.
Community Outreach and Education on Gonorrhea
Community outreach and education play a vital role in combating the rise of gonorrhea infections, particularly in light of increasing antibiotic resistance. Awareness campaigns targeted at high-risk populations can equip individuals with the knowledge of safe sex practices, STI testing, and the importance of seeking medical help upon presenting symptoms. This proactive education can significantly reduce the incidence of gonorrhea and other STIs.
Furthermore, engagement with community leaders and health organizations to address stigma surrounding sexually transmitted infections is crucial. By fostering an open dialogue about sexual health, communities can encourage individuals to take preventive measures, thereby contributing to the overall reduction of diseases such as extensively drug-resistant N. gonorrhoeae within the population.
Advancements in Gonorrhea Treatment Research
Research into new treatment options for gonorrhea is critical, particularly as existing therapies become increasingly ineffective against resistant strains. Innovations in antimicrobial agents, such as new combinations that can bypass established resistance mechanisms, are being actively pursued. The constant evolution of the bacterial genome necessitates that pharmaceutical development stays ahead of the trends observed in resistance patterns.
Collaborative research efforts between academia and healthcare settings can accelerate the realization of novel treatment strategies. Continuous investment in research not only aids in developing effective therapies against strains like XDR N. gonorrhoeae but also enhances understanding of the epidemiology of antimicrobial resistance, paving the way for better public health responses.
Frequently Asked Questions
What is Extensively Drug-Resistant Neisseria gonorrhoeae (XDR N. gonorrhoeae)?
Extensively Drug-Resistant Neisseria gonorrhoeae, or XDR N. gonorrhoeae, refers to strains of the gonorrhea-causing bacteria that are resistant to multiple antibiotics, including ceftriaxone and azithromycin. This resistance complicates treatment options, posing a significant public health threat.
What role does ceftriaxone resistance play in the spread of Extensively Drug-Resistant Neisseria gonorrhoeae?
Ceftriaxone resistance is a critical factor in the proliferation of Extensively Drug-Resistant Neisseria gonorrhoeae. As ceftriaxone is one of the last effective treatments for gonorrhea, resistance to this antibiotic greatly limits treatment options and increases the risk of treatment failure.
How does azithromycin resistance affect the treatment of gonorrhea in Canada?
Azithromycin resistance, particularly in strains of Extensively Drug-Resistant Neisseria gonorrhoeae, significantly affects gonorrhea treatment in Canada by rendering the standard dual therapy less effective. Patients may require alternative treatment regimens, such as higher doses of ceftriaxone or different antibiotic combinations.
What are the recommended gonorrhea treatments in Canada for Extensively Drug-Resistant Neisseria gonorrhoeae?
In Canada, the treatment for Extensively Drug-Resistant Neisseria gonorrhoeae typically involves high doses of ceftriaxone, with recent recommendations suggesting 500 mg as first-line therapy. Healthcare providers may also combine this with other antibiotics based on the resistance profile.
What is the importance of surveillance for Extensively Drug-Resistant Neisseria gonorrhoeae?
Surveillance for Extensively Drug-Resistant Neisseria gonorrhoeae is vital in tracking the emergence and spread of resistant strains. Continuous monitoring helps public health officials assess treatment effectiveness, implement timely interventions, and reduce the overall impact of antibiotic resistance.
How has the incidence of Neisseria gonorrhoeae infections changed in Canada recently?
The incidence of Neisseria gonorrhoeae infections in Canada has seen a dramatic increase, with reported cases rising by 146.2% since 2010, reaching 92.34 cases per 100,000 population in 2022. This rise highlights the urgent need for effective prevention and treatment strategies.
What can individuals do to protect themselves from Extensively Drug-Resistant Neisseria gonorrhoeae?
Individuals can protect themselves from Extensively Drug-Resistant Neisseria gonorrhoeae by practicing safer sex, such as using condoms, limiting the number of sexual partners, and obtaining regular screening for sexually transmitted infections (STIs), particularly if they are in high-risk situations.
Why is XDR N. gonorrhoeae classified as a high priority pathogen by the WHO?
XDR N. gonorrhoeae is classified as a high priority pathogen by the World Health Organization due to its significant resistance to multiple antibiotics, making it increasingly difficult to treat and control. Its potential for widespread prevalence emphasizes the need for urgent action in public health responses.
| Key Points | |
|---|---|
| Identification of a case in Canada | A strain resistant to ceftriaxone, cefixime, and high-level azithromycin was found. |
| Alleles associated with resistance | The strain carries penA 60.001 with A311V and 23S rRNA A2059G polymorphisms. |
| Infection transmission | Infection likely acquired while traveling in Cambodia. |
| Statistics of Neisseria gonorrhoeae in Canada | Reported cases increased 146.2% from 2010 to 2022. |
| Treatment challenges | Initial treatments failed; higher doses of ceftriaxone were eventually effective. |
| WHO Priority | N. gonorrhoeae with cephalosporin resistance is high priority for action. |
| Surveillance importance | Ongoing monitoring of antimicrobial resistance is essential. |
Summary
Extensively Drug-Resistant Neisseria gonorrhoeae represents a significant public health threat due to its resistance to key antibiotics like ceftriaxone and azithromycin. The case in Canada illustrates the urgent need for effective monitoring and treatment strategies, particularly following the report of rising cases and the established link between certain travel destinations and infection rates. Continued efforts in surveillance, research, and revised treatment protocols will be critical in managing this emerging strain of gonorrhea.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.