Ceftriaxone-resistant Salmonella Typhi poses a significant public health threat, especially in countries like Bangladesh, where the incidence of typhoid fever remains alarmingly high. This emerging strain of Salmonella enterica, identified in recent outbreaks, is notable for its genotype 4.3.1.2, which has been linked to the bla CTX-M-15 gene facilitating drug resistance. Such resistance challenges existing treatment protocols and highlights the urgent need for improved surveillance and antimicrobial stewardship. Furthermore, the situation underscores the importance of vaccine implementation to combat the spread of resistant strains. With approximately 70% of global typhoid cases occurring in South Asia, addressing ceftriaxone-resistant strains is crucial for safeguarding public health.
The rise of antibiotic-resistant infections, particularly ceftriaxone-resistant strains of Salmonella Typhi, is becoming a pressing issue worldwide. This particular serovar of Salmonella enterica is notorious for causing severe cases of typhoid fever, impacting communities and healthcare systems, especially in Bangladesh. The emergence of drug resistance, specifically within the 4.3.1.2 genotype, raises alarms among public health officials as it complicates treatment options for infected patients. It is essential to track such resistant strains systematically, considering the potential implications for disease control and public health strategies. Addressing drug resistance in typhoid fever demands a multidisciplinary approach, including better antibiotic use practices and targeted vaccination campaigns.
Understanding Ceftriaxone-Resistant Salmonella Typhi
Ceftriaxone-resistant *Salmonella Typhi* represents a significant public health challenge, particularly in regions like Bangladesh. Identified in the outbreak reported between April and September 2024, this strain is characterized by its resistance to one of the commonly prescribed antibiotics for typhoid fever treatment. As the primary cause of typhoid fever, *Salmonella enterica* serovar Typhi has evolved to resist treatment options, complicating efforts to manage the disease effectively. Increased awareness and understanding of this resistance mechanism are vital for both healthcare professionals and the public.
This resistance is notably associated with specific genetic markers, including the assertion of the bla CTX-M-15 gene found on the pCROB1 plasmid. This genetic component enhances the strain’s survivability against antibiotics, a phenomenon that highlights the urgent need for robust surveillance programs. With a documented rise in resistant cases, particularly those of genotype 4.3.1.2, a comprehensive public health strategy focusing on antibiotic stewardship and vaccination is essential to curb escalating resistance.
Frequently Asked Questions
What is Ceftriaxone-Resistant Salmonella Typhi and why is it significant?
Ceftriaxone-Resistant Salmonella Typhi refers to a strain of the bacterium *Salmonella enterica* serovar Typhi that is resistant to the antibiotic ceftriaxone. This resistance is particularly alarming because ceftriaxone is a critical treatment for severe cases of typhoid fever, a disease endemic in many regions of South Asia, including Bangladesh. The emergence of such strains signifies a growing public health crisis, requiring enhanced surveillance and effective antimicrobial stewardship.
How is ceftriaxone resistance in Salmonella Typhi identified?
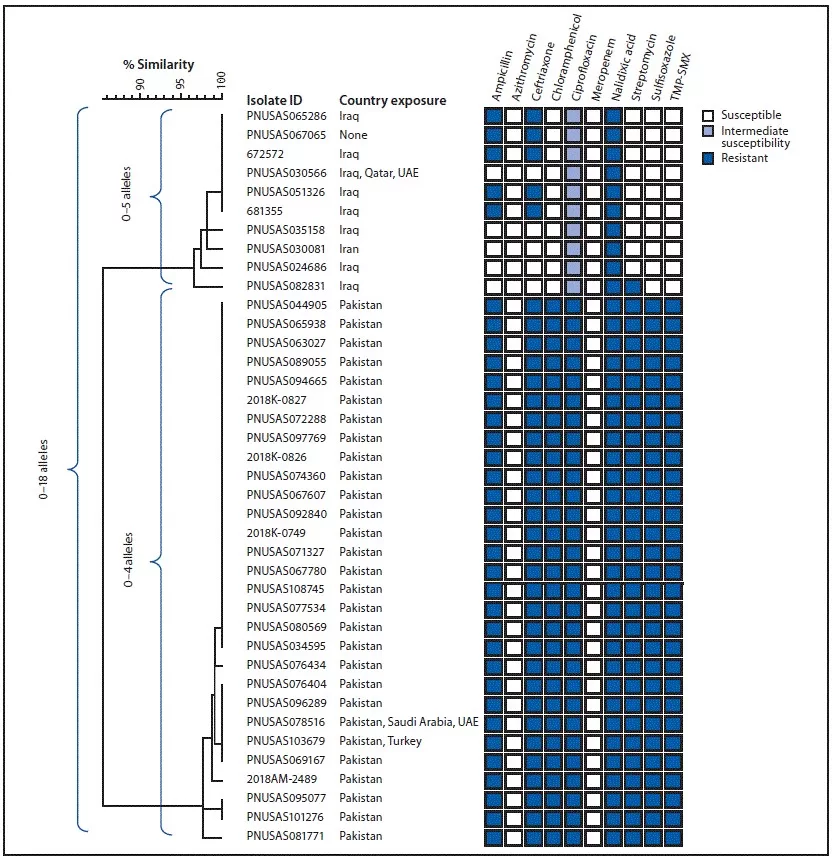
Resistance to ceftriaxone in Salmonella Typhi is typically identified through laboratory testing, such as disc diffusion or broth microdilution methods. These tests help determine the minimum inhibitory concentration (MIC) of ceftriaxone required to prevent bacterial growth. Whole-genome sequencing can further identify specific resistance genes, such as bla CTX-M-15, which are associated with ceftriaxone resistance.
What is the public health impact of ceftriaxone-resistant Salmonella enterica in Bangladesh?
Ceftriaxone-resistant Salmonella enterica poses a significant public health threat in Bangladesh, particularly as these bacteria are increasingly responsible for bloodstream infections and typhoid fever cases. The emergence of genotype 4.3.1.2, which carries the bla CTX-M-15 gene, highlights the need for urgent public health interventions, including improved disease surveillance, public awareness on antibiotic use, and widespread vaccination efforts to control the spread of drug-resistant infections.
What steps can be taken to combat ceftriaxone-resistant Salmonella Typhi outbreaks?
To combat ceftriaxone-resistant Salmonella Typhi outbreaks, several strategies are recommended: enhance antimicrobial stewardship programs to manage antibiotic use, improve public education on responsible antibiotic consumption, and reinforce disease surveillance systems to detect and respond to emerging resistant strains quickly. Additionally, promoting immunization with typhoid conjugate vaccines can significantly reduce the incidence of typhoid fever caused by resistant strains.
What are the genetic characteristics of ceftriaxone-resistant Salmonella Typhi?
Ceftriaxone-resistant Salmonella Typhi isolates have been found to belong to genotype 4.3.1.2, and they carry specific resistance genes such as bla CTX-M-15, which is often located on plasmids like pCROB1. These genetic characteristics are crucial for understanding the mechanisms behind drug resistance and for developing targeted interventions to manage outbreaks effectively.
Why has ceftriaxone-resistant Salmonella Typhi emerged in Bangladesh?
The emergence of ceftriaxone-resistant Salmonella Typhi in Bangladesh is largely attributed to the extensive empirical use of ceftriaxone and possibly inadequate antibiotic stewardship practices. These conditions facilitate the selection and proliferation of resistant strains, posing serious challenges to public health and effective disease management in the region.
What is the relationship between Salmonella enterica and typhoid fever in Bangladesh?
Salmonella enterica serovar Typhi is the bacterium that causes typhoid fever, a significant public health issue in Bangladesh. The disease is particularly prevalent among children and can lead to severe health complications. The increasing reports of drug-resistant strains, including ceftriaxone-resistant variants, exacerbate the urgency for effective prevention and treatment strategies.
| Key Point | Details |
|---|---|
| Outbreak Identification | 47 cases of ceftriaxone-resistant Salmonella Typhi reported in Bangladesh from April to September 2024. |
| Genotype | Isolates belong to genotype 4.3.1.2, carrying the bla CTX-M-15 gene. |
| Public Health Response | Urgent need for enhanced surveillance, antimicrobial stewardship, and vaccination strategies. |
| Geographical Concerns | South Asia accounts for approximately 70% of global typhoid cases, raising public health alarm. |
Summary
Ceftriaxone-Resistant Salmonella Typhi poses a significant threat to public health, as evidenced by the recent outbreak in Bangladesh involving 47 identified cases. This emerging resistance highlights the urgent necessity for intensified surveillance and effective public health strategies. To mitigate the risk of widespread infection and resistance, it is essential to enhance antimicrobial stewardship and vaccination efforts, particularly in vulnerable regions where typhoid fever remains prevalent. With the documented increase in ceftriaxone-resistant strains, proactive measures are crucial for protecting global health and preventing further complications related to antibiotic resistance.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.