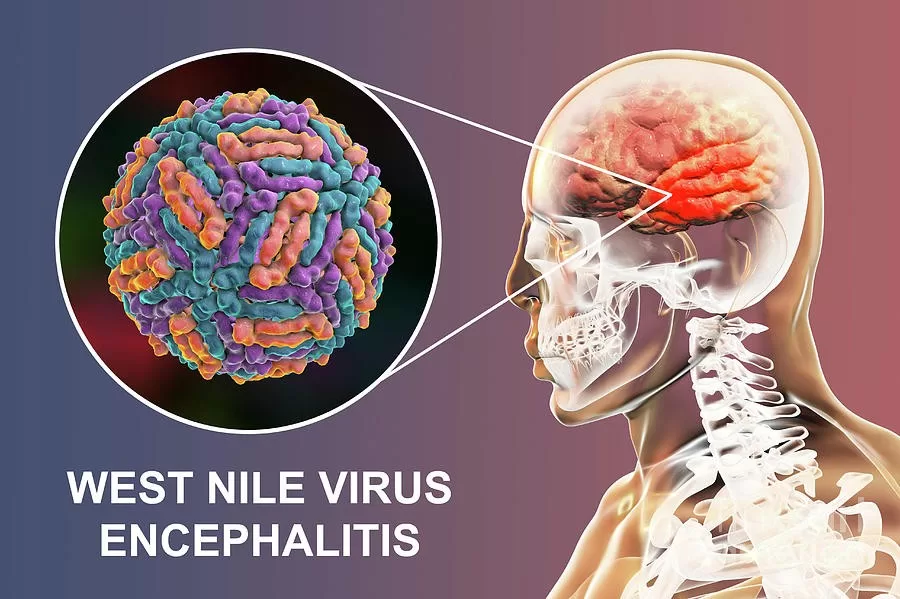
West Nile virus encephalitis is a serious neuroinvasive disease caused by the West Nile virus (WNV), which is primarily transmitted through mosquito bites. Recent reports from France indicate a worrying trend, with autochthonous WNV cases emerging in regions such as Paris, raising public health concerns. As mosquito-borne diseases continue to affect more populations, understanding the encephalitis symptoms associated with WNV becomes crucial for early diagnosis and treatment. The rise in such cases signals the potential for increased transmission, particularly as Culex and possibly Aedes types of mosquitoes flourish in urban areas. With the growing presence of West Nile virus in Europe, vigilance and preventive measures are necessary to mitigate the risks associated with this vector-borne illness.
The emergence of West Nile virus encephalitis, a severe form of viral infection affecting the brain, highlights the expanding influence of mosquito-borne pathogens in Europe. Known for causing varying degrees of illness, including encephalitis, the West Nile virus poses significant risks, particularly for those living in endemic regions like France. The recent identification of local transmission cases emphasizes the need for heightened awareness of symptoms that could indicate infections, such as fever and neurological changes. As healthcare systems adapt to these evolving threats, understanding the broader implications of neuroinvasive West Nile virus is essential in preventing further spread and protecting public health.
Understanding West Nile Virus Encephalitis Symptoms
West Nile virus encephalitis manifests through various symptoms that can vary from mild flu-like conditions to severe neurological complications. Common signs include fever, headache, and altered mental status, which can escalate to more advanced symptoms such as seizures or coma in severe cases. Individuals may also experience neck stiffness and a sudden onset of confusion, which are critical indicators of possible central nervous system involvement, often leading to hospitalization.
In the two recent cases in Paris, patients presented with febrile lymphocytic meningitis and subsequent evidence of encephalitis. The symptoms experienced by these patients are crucial for early diagnosis and intervention, especially considering the neuroinvasive nature of West Nile virus. Prompt recognition of these clinical signs can significantly impact patient outcomes, potentially mitigating the high mortality rates associated with severe neurological manifestations.
The Rise of Autochthonous West Nile Virus Cases in France
Recent data indicates an alarming rise in autochthonous West Nile virus cases within France, with notable instances reported in 2025. The two cases in Paris mark a significant concern for public health as they suggest that the virus may no longer be confined to southern regions like Camargue and Var. This could signify a broader geographical spread of the virus, driven by environmental factors conducive to mosquito breeding in northern France.
The presence of endemic Culex mosquitoes, along with invasive species like Aedes albopictus, raises additional alarms. The capability of these species to transmit the virus effectively increases the risk of outbreaks, especially during peak mosquito activity in the warmer months. As the climate continues to evolve, proactive monitoring and increased surveillance in urban areas like Paris are essential to manage and potentially prevent the spread of this mosquito-borne disease.
Implications of Neuroinvasive WNV for Public Health
The implications of neuroinvasive West Nile virus infection extend beyond individual cases to affect public health initiatives. Affected individuals may experience long-lasting neurological effects, emphasizing the need for comprehensive healthcare strategies. In light of the recent cases in Paris, healthcare providers should remain vigilant for symptoms indicative of encephalitis, particularly in patients presenting with fever and altered mental status. Enhanced testing protocols for West Nile virus should be prioritized during the mosquito season.
Furthermore, the emerging trend of neuroinvasive WNV cases demands increased public awareness and education. Understanding the risks associated with mosquito bites and the potential for severe outcomes can empower communities to take preventive measures. Public health campaigns should focus on reducing mosquito habitats, promoting personal protective measures, and informing the public about the symptoms of West Nile virus encephalitis to mitigate the impact of these mosquito-borne diseases.
Seasonal Spread of West Nile Virus in Northern France
The seasonal characteristics of West Nile virus transmission imply that the risk of infection will peak during the summer months, when Culex mosquitoes are most active. The recent confirmation of autochthonous cases during this period in Paris indicates that the virus is not only a southern threat but is now emerging in northern regions as well. This warrants a need for adaptive public health responses that enhance vector monitoring and control efforts, particularly in urban environments where mosquito breeding conditions can flourish.
In 2018, Europe experienced a significant WNV outbreak, underscoring the necessity for seasonal preparedness against mosquito-borne diseases. The spread of West Nile virus in northern France could lead to increased incidence among previously unaffected populations, necessitating vigilant epidemiological studies and public health interventions to limit potential outbreaks and safeguard public health.
Laboratory Confirmations of West Nile Virus Infection
Laboratory confirmation of West Nile virus infection is critical in the clinical management of suspected cases. The two cases reported in Paris were diagnosed through rigorous testing methods, including PCR assays that revealed the presence of the virus in both blood and cerebrospinal fluid samples. These diagnostic tools are vital for distinguishing WNV from other viral meningitides to ensure appropriate treatment and care.
Improving access to rapid diagnostic testing for West Nile virus can enhance clinical outcomes by facilitating timely treatment decisions. As the cases in Paris illustrate, the acute nature of symptoms related to neuroinvasive WNV infections requires healthcare teams to act quickly. Public health labs must be equipped to handle increased testing demands to respond effectively to potential outbreaks, thereby strengthening the overall healthcare response to these mosquito-borne diseases.
Preventive Measures Against Mosquito-Borne Diseases
Preventive measures play a pivotal role in controlling the spread of mosquito-borne diseases like West Nile virus. Community education regarding the elimination of standing water, the use of insect repellent, and the installation of screens on windows can significantly reduce mosquito populations and, subsequently, the incidence of WNV infections. Local health departments must engage in outreach programs that emphasize these practices to ensure broadened community participation.
Additionally, strategic mosquito control programs, including larviciding and adulticiding, should be implemented, particularly in urban areas experiencing a rise in autochthonous WNV cases. A collaborative approach involving public health agencies, environmental services, and community volunteers can create a robust framework for reducing mosquito-borne disease transmission within affected regions.
Travel and West Nile Virus Awareness
With the rise of autochthonous West Nile virus cases, it becomes increasingly important for travelers within France to be aware of the risks associated with mosquito exposure. Whether living or traveling in regions where the virus is reported, locals and visitors alike must remain informed about the symptoms of West Nile virus infection and take appropriate preventative measures. This awareness is crucial to reduce transmission risks, particularly during peak mosquito activity times.
Travel advisories should include information about the prevalence of West Nile virus in various regions, encouraging both awareness and behavioral changes to mitigate exposure. For instance, educating travelers to wear long sleeves, apply mosquito repellents, and avoid outdoor activities during peak mosquito hours can significantly reduce the likelihood of infection, particularly in regions like northern France experiencing shifts in WNV activity.
The Role of Climate in WNV Transmission
Climate plays a significant role in the transmission dynamics of West Nile virus, directly influencing mosquito populations and their breeding habits. Warmer temperatures and increased rainfall create favorable breeding conditions for mosquitoes, which may elevate the risk of WNV transmission to humans. Understanding these climatic patterns is essential for predicting potential outbreaks and implementing preventative health strategies effectively.
The recent emergence of West Nile virus in northern France can be attributed, in part, to climatic changes that favor the proliferation of mosquito vectors. Monitoring local climate trends and their correlation with WNV activity can aid public health officials in developing risk assessments and response strategies. As climate change continues to alter environmental conditions, vigilance in understanding its impact on mosquito-borne diseases like West Nile virus will become increasingly critical.
Long-Term Health Effects of West Nile Virus Infections
The long-term health effects associated with neuroinvasive West Nile virus infections can be profound and vary widely among patients. While some individuals may fully recover from symptoms, others may experience lingering issues such as cognitive impairment, fatigue, and motor difficulties that can significantly affect quality of life. Understanding these potential complications underscores the importance of early detection and comprehensive follow-up care for WNV patients.
As the two cases encountered in Paris emphasize, there is a pressing need for awareness among healthcare providers about the potential for chronic sequelae from West Nile virus infections. Increased monitoring, research into rehabilitation options, and support for affected individuals can contribute to better health outcomes and improved management of long-term effects, enhancing patient care for those impacted by this mosquito-borne disease.
Frequently Asked Questions
What is West Nile virus encephalitis and how does it relate to mosquito-borne diseases?
West Nile virus encephalitis is a severe neuroinvasive disease caused by the West Nile virus (WNV), primarily transmitted through the bites of infected mosquitoes, particularly from the Culex species. It represents one of the serious outcomes of mosquito-borne diseases, which can lead to inflammation of the brain and significant neurological complications.
How common are autochthonous West Nile virus cases in France?
Autochthonous West Nile virus cases have been increasingly reported in France, especially in regions like the Camargue and the Var and Aquitaine regions. Recent cases in Paris suggest that the virus is spreading northward, raising awareness about the risks associated with local transmission.
What are the typical encephalitis symptoms associated with West Nile virus infection?
Symptoms of West Nile virus encephalitis can include fever, headache, neck stiffness, altered mental status, and other neurological symptoms. In severe cases, it can lead to more significant complications, including seizures and coma, particularly in older adults or those with weakened immune systems.
What is neuroinvasive WNV and why is it a concern?
Neuroinvasive West Nile virus (WNV) refers to cases where the virus invades the central nervous system, leading to conditions such as encephalitis or meningitis. This form of infection often results in more severe health outcomes and higher mortality rates, making it a significant public health concern, especially in newly affected areas like northern France.
How does the spread of West Nile virus in France impact public health?
The spread of West Nile virus in France poses serious public health implications, including increasing rates of encephalitis cases and the potential for blood or organ donations to transmit the virus. The emergence of cases in areas previously considered low-risk highlights the need for enhanced surveillance and vector control measures.
What actions can be taken to prevent West Nile virus encephalitis?
Preventive measures against West Nile virus encephalitis include reducing mosquito breeding sites by eliminating standing water, using insect repellents, wearing protective clothing, and avoiding outdoor activities during peak mosquito activity times. Public awareness campaigns are crucial for educating communities about the risks and protective strategies.
| Aspect | Details |
|---|---|
| Location | Paris, France; cases occurred in 2025 |
| Key Findings | Two cases of West Nile virus encephalitis leading to febrile lymphocytic meningitis were reported. |
| Transmission | Primarily Culex spp. mosquitoes; potential involvement of Aedes albopictus in Paris. |
| Patient 1 | 64-year-old male, symptoms included headache and altered mental status, tested positive for WNV after travel to eastern France. |
| Patient 2 | 25-year-old female, presented with fever and neck stiffness, tested positive for WNV without traveling outside Paris. |
| Implications | High mortality risk for neuroinvasive WNV; need for increased awareness in healthcare. |
| Spread | WNV may be spreading northward in France, alarming for future outbreaks and blood donations. |
Summary
West Nile virus encephalitis is becoming a growing concern in France, particularly evident from the two recent cases reported in Paris. This disease, primarily transmitted by mosquitoes, has demonstrated a troubling expansion beyond its known endemic areas, indicating that West Nile virus encephalitis may pose significant health risks even in urban settings. Health authorities must remain vigilant and adapt their preventative measures as WNV continues to spread.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.