Vaccine myths have circulated for decades, often fueled by fear and misinformation rather than fact. One of the most pervasive myths is the unfounded belief that vaccines cause autism, despite rigorous research debunking this notion. Many parents encounter vaccine misinformation that claims vaccines are unsafe or that their side effects are more harmful than the diseases they prevent. The conversation surrounding vaccines and autism continues to spark confusion and anxiety for parents, who want nothing but the best for their children. By actively engaging in debunking vaccine myths, we can pave the way for informed choices grounded in scientific evidence and proven vaccine safety.
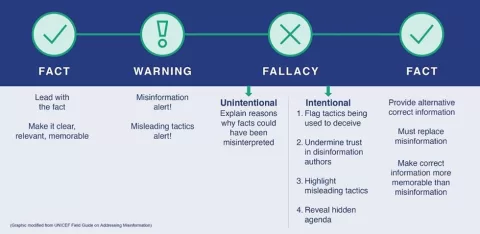
When discussing immunization misconceptions, many alternative terms come into play, such as vaccine fallacies and vaccine conspiracy theories. These misconceptions often stem from unverified anecdotes and anecdotal evidence that mislead the public. Instead of recognizing the overwhelming scientific consensus on vaccine safety, individuals may rely on outdated or manipulated claims. This dialogue reflects deeper societal issues around trust in experts and a growing disconnection from empirical evidence. Understanding the nuances of vaccination debates is crucial for dispelling myths that endanger public health.
Debunking Vaccine Myths: The Myth of Vaccines and Autism
One of the most tenacious myths surrounding vaccines is the claim that they cause autism. This misconception largely stems from a discredited 1998 study by Andrew Wakefield, which falsely linked the MMR (measles, mumps, and rubella) vaccine to autism spectrum disorders. Despite numerous large-scale studies disproving this connection, including an extensive review by the Institute of Medicine, the myth persists due to the emotional weight it carries for parents. Because autism symptoms typically manifest during the early years of life, coinciding with vaccination schedules, this temporal association fuels unwarranted fear and speculation.
Attempts to blame vaccines for autism have also shifted focus over the years, initially targeting thimerosal, a mercury-containing preservative, and later emphasizing the number of vaccines administered in early childhood. Each hypothesis has failed under scientific scrutiny. Public health experts continuously stress that rigorous studies, investigating millions of children, consistently show no link between vaccination and autism. The persistence of this myth highlights the critical need for clear communication and education about vaccine safety, steering discussions away from emotion and towards evidence-based conclusions.
Vaccine Safety: Understanding Risks and Evidence
Another common myth is the belief that vaccines cause severe diseases such as sudden infant death syndrome (SIDS), autoimmune disorders, or even cancer. These claims often emerge from a misunderstanding of correlation versus causation. SIDS, for instance, peaks at the same age that children receive several vaccinations, leading some to mistakenly attribute the cause. However, extensive research reveals that SIDS rates have decreased significantly thanks to changes in sleep recommendations, independent of vaccination history. It’s essential to approach these discussions with data that underscore the rigorous testing vaccines undergo prior to approval.
Additionally, vaccine safety is continuously monitored even after approval. Scientific institutions like the CDC and the FDA conduct ongoing research to assess any long-term consequences of vaccines. Such thorough evaluations consistently find that the benefits far outweigh the risks. Public health campaigns must reinforce this narrative, using factual data and transparent dialogue to combat the myths surrounding vaccine safety. Misinformation can undermine vaccine confidence, but educating communities about the actual evidence can empower parents to make informed choices.
The Misuse of VAERS: A Critical Perspective
The Vaccine Adverse Event Reporting System (VAERS) has become a focal point for misinformation regarding vaccine safety. This system allows anyone to report adverse reactions post-vaccination, leading some to conclude that these reports serve as proof of vaccines causing significant harm. However, VAERS reports are not verified for causality, making them unreliable for substantiating claims about vaccines leading to severe outcomes or fatalities. Public understanding of VAERS needs clarity: it is a tool for identifying potential safety signals, but it is not definitive proof that vaccines cause harm.
Scientific reviews are essential to interpreting VAERS data. For example, during the 2014-2015 measles outbreak, claims circulated that the MMR vaccine resulted in multiple deaths, which were refuted upon thorough investigation of the actual medical records and circumstances surrounding reported deaths. These efforts showed no causal link between the vaccine and deaths, reiterating the importance of informed scrutiny. Engaging in transparent discussions about the limitations of VAERS can help demystify the data and mitigate unwarranted fears stemming from misinformation.
Natural Immunity vs. Vaccine-Induced Immunity
The argument that natural immunity is superior to immunity acquired from vaccination persists despite overwhelming evidence to the contrary. Natural infections, such as measles, can lead to severe complications, including encephalitis and long-term immune system damage, which vaccines are designed to prevent. The disruption to immune memory caused by diseases like measles significantly increases susceptibility to other infections, thereby questioning the safety and efficacy of relying on natural immunity alone. Vaccination provides a safer, controlled method of developing immunity, significantly reducing hospitalizations and deaths.
Additionally, viruses like influenza mutate rapidly, complicating the immunity acquired from natural infections. Immunity from such infections does not guarantee complete protection against future strains, creating a heightened risk of recurrent illness. Vaccines are regularly updated to tackle these evolving viruses, ensuring that public health remains protected. Promoting understanding of vaccine science over the allure of natural immunity narratives is crucial in establishing a community that values vaccine efficacy and safety.
mRNA Vaccines: Separating Fact from Fiction
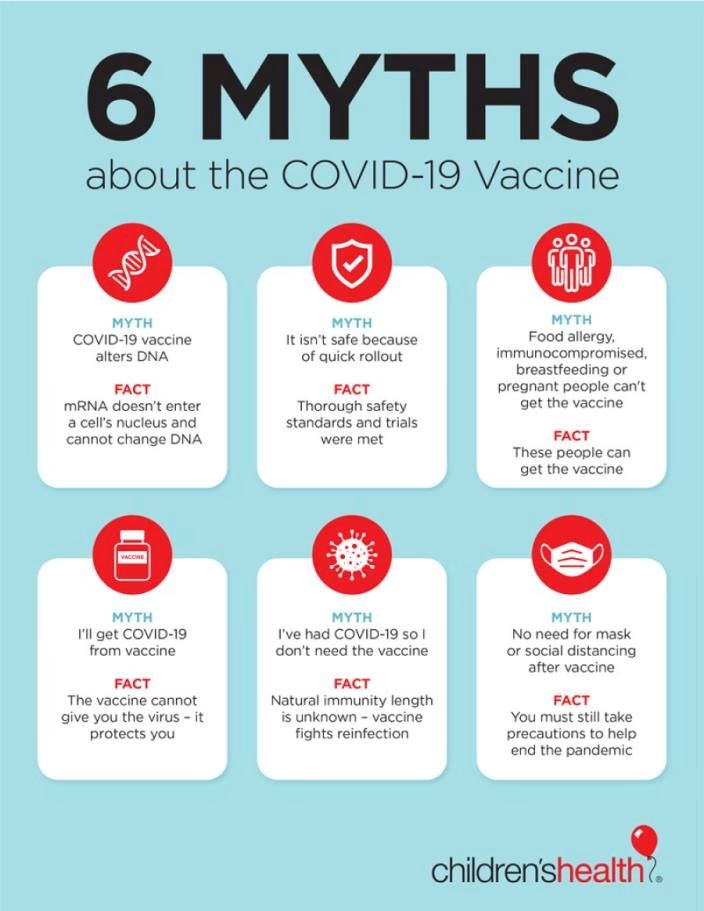
In the wake of the COVID-19 pandemic, the emergence of mRNA vaccines has led to widespread confusion, with claims that they function as gene therapy or induce aggressive cancers. This misconstrues the essential mechanisms of how mRNA vaccines work; they do not alter DNA or integrate into the genome. Instead, they utilize a naturally occurring process to instruct cells to produce proteins that stimulate an immune response. Understanding this fundamental difference can assuage fears surrounding the safety and efficacy of mRNA technology in vaccination programs.
The narrative associating mRNA vaccines with ‘turbo cancers’ is equally unfounded. Extensive studies following vaccination campaigns have not revealed unusual cancer patterns, which contrasts sharp claims made by skeptics. The immune response initiated by mRNA vaccines enhances the body’s ability to recognize and combat pathogens, including potential tumor cells. Comprehensive communication and public engagement with the scientific community are crucial to dispelling these myths while promoting confidence in mRNA technology as a significant advancement in modern medicine.
Addressing Parental Concerns: The Role of Compassion in Vaccine Education
As misinformation about vaccines continues to circulate, it is vital to approach parents and caregivers with understanding and compassion, not condescension. Parents grappling with vaccine hesitancy are often motivated by a genuine desire to protect their children. They deserve clear, evidence-based information that directly addresses their concerns, rather than being dismissed or belittled. Establishing a respectful dialogue can build trust, encouraging them to consider scientific perspectives on vaccine safety and efficacy.
Moreover, education initiatives must emphasize that vaccine misconceptions are often rooted in emotional narratives rather than factual evidence. Utilizing empathetic communication can help address common fears and clarify the overwhelming benefits of vaccinization. Providing accurate resources, ongoing community support, and open forums to discuss vaccines can pave the way for a more informed population. By nurturing an environment that values thoughtful engagement, communities can more effectively counteract vaccine myths.
Understanding the Science Behind Vaccine Development
A common myth regarding vaccines is the misconception that they have not undergone rigorous testing before being administed to the public. In reality, vaccine development involves a multi-phase process that spans years, if not decades. Each stage, from laboratory research to clinical trials, is designed to ensure the safety and efficacy of each vaccine. Regulatory health authorities evaluate not only the resulting data but also the processes behind vaccine development before granting approval.
Post-approval, ongoing surveillance systems monitor millions of vaccinated individuals to assess any long-term side effects and outcomes. This robust oversight framework provides reassurance to public health officials and the general population alike, confirming that vaccines remain safe and effective across diverse demographics. Continuous education about these processes can help demystify vaccine approval and combat unfounded myths that portray vaccines as unchecked medical interventions.
The Role of Evidence-Based Public Health Policy in Vaccine Advocacy
Advocating for vaccines in the face of persistent myths requires concerted efforts using evidence-based public health policies. Data collected from reputable studies representing diverse populations support the argument for widespread vaccination, reflecting the success in disease prevention and control. Policymakers and healthcare professionals must collaborate to convey this information clearly, underscoring the demonstrable reduction in disease incidence due to vaccinations.
Additionally, public health campaigns should focus on addressing vaccine misinformation through strategic messaging and community outreach initiatives. This targeted approach can help foster a more informed public that understands the balance between vaccine risks and their undeniable benefits. Generating robust support for vaccine policies can significantly enhance community resilience against misinformation and contribute to overall public health safety.
The Lasting Impact of Vaccine Myths on Public Perception
Vaccine myths have a profound impact on public perception and behavior, shaping attitudes around concepts of trust, safety, and community health. Understanding these narratives reveals underlying fears related to protecting loved ones, skepticism towards authoritative figures, and the demand for reassurance about personal choices. While these instincts are justified, the misinformation associated with vaccines nurtures a culture of doubt that hinders public health efforts.
To combat this issue, it is critical to actively engage communities in discussions about vaccine efficacy, accessibility, and dispelling common myths. By fostering constructive dialogues that emphasize respect and evidence-based understanding, vaccine advocates can work towards restoring public confidence in vaccination as a fundamental component of health care. The consequences of failing to address these narratives can profoundly impact not only individual families but public health as a whole.
Frequently Asked Questions
What are some common vaccine myths regarding vaccine misinformation?
Vaccine misinformation often revolves around several myths. Common examples include the false belief that vaccines cause autism, the assumption that vaccinated and unvaccinated children have not been properly compared, and the idea that vaccines contain toxic ingredients. These misconceptions persist despite extensive research and studies that debunk them.
How does vaccine safety support debunking vaccine myths?
Vaccine safety is supported by decades of research and monitoring which confirm that vaccines are safe for the vast majority of people. Regulatory agencies like the FDA and CDC have rigorously reviewed vaccine safety data, and studies consistently show no linkage between vaccines and serious side effects like autism or autoimmune diseases, thus debunking prevalent vaccine myths.
What evidence exists to counter the myth that vaccines cause autism?
The claim that vaccines cause autism originated from a flawed study that was later retracted. Since then, numerous large-scale studies have found no causal relationship between vaccination and autism. Research showing no increase in autism rates following the removal of thimerosal from vaccines further debunks this myth.
Can vaccine side effects justify the myths about vaccines being hazardous?
While some individuals may experience mild side effects from vaccines, such as soreness at the injection site or fatigue, these reactions are typically temporary and considerably less dangerous than the diseases vaccines prevent. Serious side effects are exceedingly rare, and comprehensive research demonstrates that the benefits of vaccination far exceed the risks.
How do researchers debunk the myth that mRNA vaccines alter DNA?
The myth that mRNA vaccines, like the COVID-19 vaccines, can alter DNA is unfounded. mRNA vaccines work by providing instructions to cells to produce a virus protein, prompting an immune response. They do not enter the cell nucleus where DNA is stored and cannot integrate into the genome, reinforcing the narrative that these vaccines are safe and effective.
What are the facts about the myth that vaccines lead to conditions like SIDS and allergies?
Claims linking vaccines to conditions such as sudden infant death syndrome (SIDS) or allergies are based on correlational assumptions rather than causal evidence. Both SIDS and allergies occur naturally in the early stages of life, coinciding with vaccination times, which can mislead parents into mistakenly associating vaccines with these conditions. Studies consistently show no positive correlation between vaccines and these health issues.
Is the Vaccine Adverse Event Reporting System (VAERS) a reliable source for vaccine safety?
While VAERS provides a platform for reporting adverse events post-vaccination, it is not a definitive indicator of vaccine safety because it relies on unverified reports. Investigations into reported events review comprehensive medical data and consistently reveal that most claims do not imply causation between vaccines and reported adverse outcomes.
What does research say about natural immunity versus vaccine-induced immunity?
Research indicates that while natural immunity can occur after infection, vaccine-induced immunity provides a safer alternative with less risk of serious complications like severe illness or death from the actual disease. Also, vaccines offer protection without the drawbacks associated with natural infections, such as long-term health issues.
How can we combat vaccine myths and misinformation effectively?
Combating vaccine myths requires transparent communication, providing evidence-based information, and outreach efforts that respect parents’ concerns. Education that focuses on factual data regarding vaccine efficacy and safety can help correct misconceptions and bolster public trust in vaccination.
| Myth | Explanation | Evidence Against |
|---|---|---|
| Vaccines were never properly tested | Claims that vaccines lack proper testing and trials are unfounded. | Extensive research and multiple studies prove the contrary. |
| Vaccinated and unvaccinated children haven’t been compared | Assertions that there are no comparisons between vaccinated and unvaccinated children are false. | Numerous studies have compared these populations and found no significant differences in key health outcomes. |
| The ingredients are toxic | Arguments that vaccine components are inherently harmful misconstrue their safe, minimal concentrations. | Independent studies confirm the safety of vaccine ingredients at doses used in immunizations. |
| Too many, too soon | Concerns about the timing and number of vaccines are based on misunderstandings of immunology and safety protocols. | Research shows current schedules are safe and effective, preventing more diseases than they cause. |
| Vaccines cause autism | The false connection between vaccines and autism arose from a retracted study with severe methodological flaws. | Extensive investigations have found no evidence supporting any link between vaccines and autism. |
| Vaccines cause SIDS, autoimmune diseases, allergies, and cancer | Attributing early childhood conditions to vaccines is a logical fallacy; it’s not causal. | Correlation does not imply causation; significant evidence refutes these claims. |
| VAERS proves vaccines are killing people | Misinterpretation of VAERS data overlooks that it does not establish causation between vaccines and adverse effects. | Thorough investigation of VAERS reports shows alternative causes, confirming vaccine safety. |
| The flu shot gave me the flu / Natural immunity is better | Claims about flu shots causing illness and preference for natural immunity misrepresent actual vaccine effects. | Flu vaccines cannot cause flu, and natural infections present serious risks, unlike vaccinated immunity. |
| mRNA vaccines are gene therapy that causes turbo cancers | Misconceptions regarding mRNA mechanisms suggest they alter DNA; this is scientifically incorrect. | mRNA does not integrate into DNA and has shown no links to unusual cancer incidences. |
Summary
Vaccine myths continue to thrive despite overwhelming evidence discrediting them. These widespread misconceptions, such as the false association of vaccines with autism or claims that they are responsible for serious health risks like SIDS and cancer, stem from a fundamental misunderstanding of science and a misrepresentation of data. Addressing and debunking these myths is essential to improving public health and ensuring the safety of vaccination programs. By providing accurate, evidence-based information, we can help dispel these persistent vaccine myths and foster a more informed and healthier society.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.