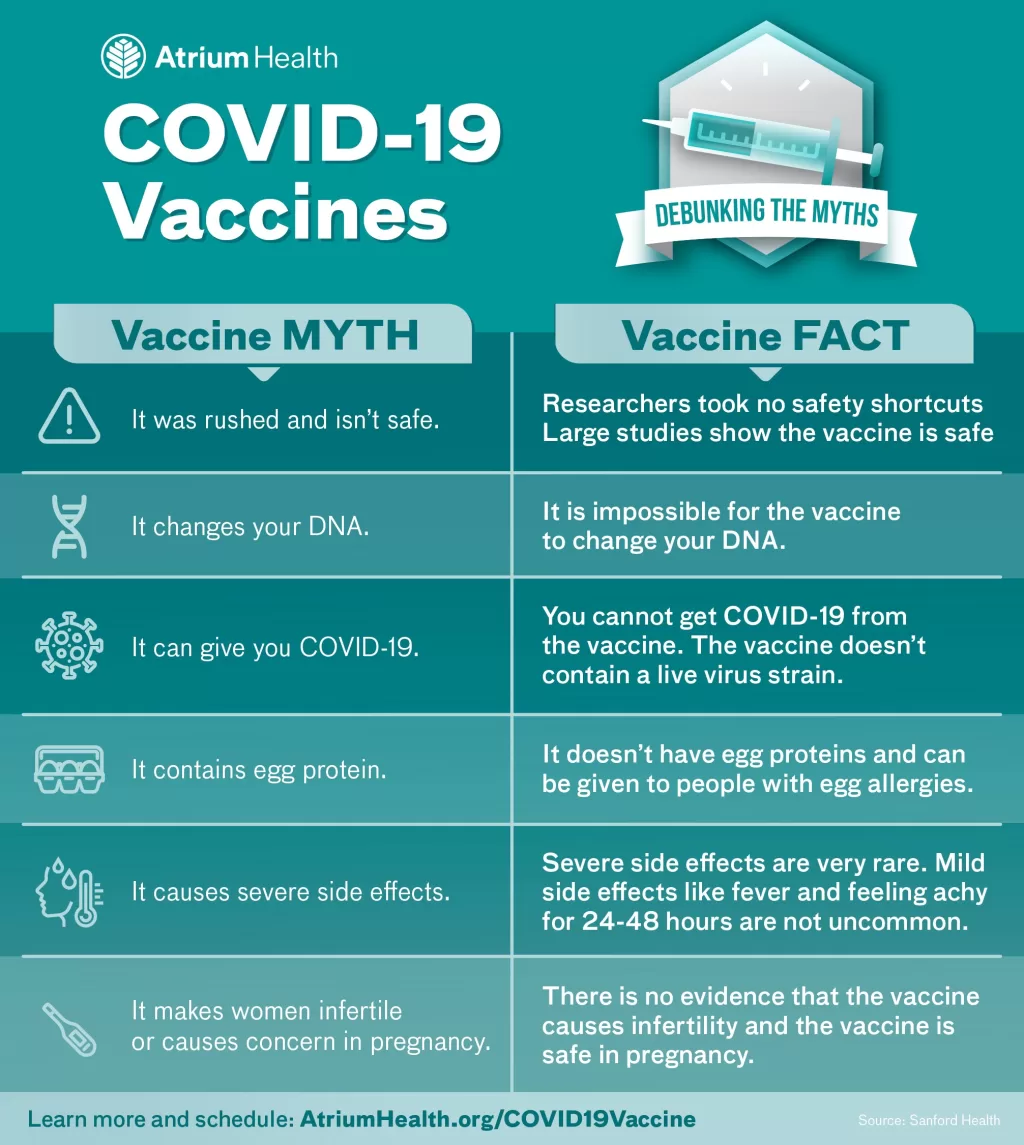
Vaccine myths have become a pervasive issue, especially evident during recent measles outbreaks that have sparked public concern and misinformation. These myths often stem from unfounded beliefs about vaccine safety and efficacy, particularly within marginalized communities. For instance, some narratives suggest that racial differences necessitate alternative vaccination schedules, despite scientific evidence debunking such claims. Misconceptions about vaccines can lead to hesitancy, which contributes to a decline in childhood vaccination rates and, consequently, outbreaks of preventable diseases like measles. Addressing these myths through effective health communication strategies is crucial for public health, as they play a vital role in combating misinformation and fostering trust in vaccines.
The widespread falsehoods surrounding vaccinations, often referred to as immunization misconceptions, significantly impact public health initiatives. This phenomenon has gained attention particularly during measles outbreaks, where misinformation has led to increased vaccine hesitancy among parents. Many of these misleading beliefs are rooted in outdated or debunked studies, which create confusion and fear regarding vaccine safety. Furthermore, the dialogue surrounding health communication has shifted towards fostering open discussions rather than merely fact-checking, aiming to engage communities more effectively. With emerging technologies and platforms, such as AI chatbots in healthcare, there is an opportunity to improve the dissemination of accurate health information and counteract these harmful myths.
Combating Race-Based Vaccine Myths During Measles Outbreaks
The resurgence of measles outbreaks in various regions, particularly in Texas, has coincided with a troubling increase in race-based vaccine myths. These myths often mislead the public into believing that vaccination schedules should differ based on race, a notion without scientific backing. Despite data suggesting that individuals of African descent may show a different immune response to certain vaccines, it is essential to emphasize that race is a social construct. The scientific community has consistently reiterated that no evidence supports the need for race-specific vaccine schedules. This misinformation not only confuses parents but also contributes to vaccine hesitancy, which can lead to increased infection rates among vulnerable populations.
Social media plays a significant role in spreading these vaccine myths, often amplifying voices that promote misinformation. For instance, during Senate hearings, claims regarding race-based vaccine schedules gained traction, which sparked a wave of reactions online. Influential figures, such as Senator Angela Alsobrooks, have attempted to counter these narratives by sharing factual information and expressing concerns about the implications of such myths. Unfortunately, the debate often sees individuals clinging to long-debunked misconceptions, which further complicates public understanding. To combat this, health communication strategies must focus on engaging communities in meaningful dialogues that clarify the misconception surrounding vaccine safety and efficacy.
The Evolution of Health Communication Strategies
In light of the ongoing misinformation surrounding vaccines, health communication strategies are evolving to foster more effective engagement with the public. Traditional methods often relied on fact-checking, which, while important, may not resonate with individuals harboring doubts or fears about health interventions. Emerging approaches, such as ‘bypassing’, aim to present accurate information in a way that acknowledges people’s concerns without directly confronting their beliefs. This method encourages health professionals to frame discussions around the benefits of vaccines rather than simply denying false claims. By sharing relatable narratives, these strategies can help shift public sentiment toward a more informed perspective.
Moreover, there is a growing recognition that health communication should not only focus on conveying facts but also on understanding the emotional and social contexts in which people make health decisions. For instance, when addressing vaccine hesitancy, it is crucial to engage with parents’ fears about their children’s health, and provide clear, empathetic explanations that can resonate with their experiences. Utilizing storytelling techniques and community outreach can bridge gaps in understanding and build trust, ultimately leading to better health outcomes. As researchers continue to explore these innovative communication methods, the goal remains to enhance public health literacy and counteract harmful misinformation.
Challenging Established Science: New Public Health Journal
The emergence of the Journal of the Academy of Public Health has stirred controversy in the scientific community, particularly for its challenge to widely accepted scientific consensus. Co-founded by individuals with political ties, this journal has begun publishing articles that question established findings, such as the efficacy of COVID-19 vaccines and the role of masks in schools. While the journal’s open-access model allows for a broader range of voices, critics argue that its potential biases could undermine public trust in scientific research. This raises important questions about the credibility of publications that diverge from mainstream scientific thought, especially in a field where misinformation can have dire consequences.
The journal’s approach may appeal to those who feel disenfranchised by conventional public health narratives, particularly among certain political factions. However, this also highlights a critical need for transparency and rigorous peer review in scientific publishing. As public health journals grapple with the balance between diverse perspectives and maintaining scientific rigor, the integrity of research is paramount. Ensuring that studies published in such journals adhere to high standards can help prevent the spread of misinformation that could jeopardize public health, especially during health crises.
Heart Attack Misconceptions and Their Consequences
Despite ongoing education efforts, misconceptions surrounding heart attack treatment and prevention remain prevalent, particularly in older populations. One common myth is the belief in ‘cough CPR’, which suggests that coughing can help maintain blood flow during a heart attack. Health experts have categorically debunked this notion, clarifying that CPR is intended for cardiac arrest scenarios and that coughing cannot effectively restart a heart. Misunderstandings like these can lead to dangerous delays in seeking appropriate medical care, emphasizing the need for clear communication about the realities of heart health.
Additionally, outdated practices, such as the routine use of aspirin for heart attack prevention, continue to confuse many. While past guidelines recommended daily low-dose aspirin for all adults, recent research has shown that this practice is not advisable for everyone, particularly older adults who may be at risk for gastrointestinal bleeding. Surveys indicate a significant portion of the population still believes in the benefits of aspirin for prevention, showcasing the gap between updated medical advice and public understanding. To mitigate these misconceptions, targeted health campaigns must focus on providing accurate, evidence-based information that empowers individuals to make informed decisions about their heart health.
AI Chatbots in Healthcare: Navigating Research Gaps
The integration of artificial intelligence (AI) in healthcare represents a transformative shift, yet it also raises critical questions about accuracy and reliability. As AI chatbots become more prevalent in providing medical advice, the lack of standardized research frameworks to evaluate their effectiveness poses significant challenges. A systematic review of studies examining large language models (LLMs) revealed that many did not disclose essential details about their functionality or the ethical implications of their use. This opacity can lead to misinformation being disseminated under the guise of authoritative health advice, potentially compromising patient safety.
Moreover, the variability in study designs assessing AI chatbots highlights the urgent need for consensus on research standards. Without rigorous evaluation methods, it is difficult to ascertain which AI systems are genuinely beneficial and safe for public use. To address this gap, researchers and policymakers must collaborate to develop comprehensive guidelines that ensure AI chatbots are held to high standards of accuracy, transparency, and ethical responsibility. This will not only enhance trust in AI technologies but also protect patients from the risks associated with inadequate or misleading health information.
Frequently Asked Questions
What are some common vaccine myths related to measles outbreaks?
Vaccine myths associated with measles outbreaks often include false claims about race-based vaccine schedules, suggesting that children of different races require different vaccination regimens. This misconception has been fueled by misinformation, despite scientific evidence showing that vaccines are safe and effective for all children, regardless of race.
How do heart attack misconceptions relate to vaccine myths?
Heart attack misconceptions can parallel vaccine myths in that both can lead to harmful health behaviors. For instance, the false belief that coughing can help during a heart attack may delay critical care, similar to how vaccine myths can deter individuals from getting vaccinated, leading to increased vulnerability to diseases like measles.
Why is health communication important in combating vaccine myths?
Effective health communication is vital in combating vaccine myths, as it fosters open dialogue and helps individuals understand the benefits and risks of vaccines. By addressing misconceptions directly and providing clear, evidence-based information, health professionals can build trust and encourage informed decision-making about vaccinations.
What role do public health journals play in addressing vaccine myths?
Public health journals play a crucial role in disseminating accurate information about vaccines and countering myths by publishing peer-reviewed research. They provide a platform for scientists to address misconceptions and promote evidence-based practices, which is essential in maintaining public trust in vaccination programs.
How can AI chatbots in healthcare help reduce vaccine myths?
AI chatbots in healthcare can help reduce vaccine myths by providing accurate, instant answers to vaccine-related questions. However, it is crucial to ensure that these chatbots are designed with high research standards to avoid spreading misinformation and to enhance public understanding of vaccine safety and efficacy.
What are some misconceptions about vaccines and autism that fuel vaccine myths?
Misconceptions linking vaccines to autism, particularly among Black children, often stem from retracted studies and flawed research. These myths, which falsely claim a connection between the MMR vaccine and autism, can lead to vaccine hesitancy and contribute to outbreaks of vaccine-preventable diseases like measles.
How can communities improve health communication to combat vaccine myths?
Communities can improve health communication by fostering discussions that emphasize empathy and understanding. By moving beyond simple fact-checking and engaging individuals with relatable narratives about vaccine benefits, communities can effectively counter vaccine myths and encourage higher vaccination rates.
What impact do vaccine myths have on public health during measles outbreaks?
Vaccine myths can significantly impact public health during measles outbreaks by reducing vaccination rates. Misinformation contributes to vaccine hesitancy, leading to decreased herd immunity and increased risk of disease transmission, thereby exacerbating outbreaks and public health crises.
| Key Points | Details | |
|---|---|---|
| Race-Based Vaccine Myths | Misinformation about vaccines, particularly concerning Black children and vaccine schedules, is influencing public perception amid measles outbreaks. | |
| Measles Outbreaks | Recent outbreaks in Texas have intensified the spread of race-based vaccine myths, mainly through social media and public figures. | |
| Heart Attack Misconceptions | False beliefs persist about heart attack treatment and prevention, including the myth of ‘cough CPR’ and outdated aspirin guidelines. | |
| Health Communication Shifts | Health communication is moving from fact-checking to fostering open dialogue and presenting facts to counter misinformation. | |
| New Public Health Journal | A new journal questions established science, raising concerns about bias and the credibility of its findings. | |
| AI in Healthcare | Research gaps exist in evaluating AI chatbots used in healthcare, particularly in terms of transparency and safety. | |
Summary
Vaccine myths continue to pose significant challenges to public health, particularly during outbreaks of diseases like measles. Misinformation surrounding race-based vaccine schedules and false claims linking vaccines to autism have gained traction, despite overwhelming scientific evidence debunking these narratives. As health communication strategies evolve to address these myths, fostering open dialogue and presenting facts in relatable terms are emerging as crucial approaches. By addressing these vaccine myths head-on, public health initiatives can work towards rebuilding trust and improving vaccination rates among communities.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.