Recent reports indicate an alarming surge in US malaria cases, with the CDC highlighting the first instances of locally transmitted malaria in over two decades. From May to September 2023, ten individuals across Florida, Texas, Arkansas, and Maryland fell victim to this mosquito-borne illness, raising concerns among public health officials. These locally transmitted cases, attributed to the ever-persistent Anopheles mosquitoes, present a serious reminder of the potential for malaria outbreaks in the US, especially as climate change continues to create conducive conditions for vector proliferation. In light of these troubling developments, the CDC report on malaria emphasizes the need for robust malaria prevention strategies to mitigate future risks. As imported malaria cases hit record highs in 2023, vigilance in preventing further transmission has never been more crucial.
The recent increase in malaria incidents in the United States marks a pivotal moment in public health, particularly in relation to mosquito-borne diseases. Known for its connection to regions with high humidity and temperatures, malaria was previously considered eradicated in the US, with the last documented local cases dating back to 2003. With the recent emergence of locally acquired cases, particularly those involving the *Plasmodium spp.* parasites transmitted by *Anopheles* mosquitoes, authorities are on high alert. This resurgence underlines the urgent necessity for effective malaria control measures and public awareness campaigns to bolster prevention efforts. A comprehensive approach incorporating surveillance, education, and active monitoring is vital to ensure that the threat of malaria does not reestablish itself in the American landscape.
Understanding the Surge of US Malaria Cases
Recent reports indicate a concerning rise in locally transmitted malaria cases across the United States, specifically highlighting ten cases identified in just a few months. The occurrences, particularly in states like Florida, Texas, Arkansas, and Maryland, mark the first homegrown malaria cases in two decades, raising alarms about public health preparedness for mosquito-borne diseases. Notably, the increased mobility of people between malaria-endemic regions and the presence of *Anopheles mosquitoes*, the primary carriers of the malaria parasite, contribute to the growing risk of transmission in the US.
According to a CDC report, factors such as the spiraling numbers of imported malaria cases and exceptionally hot weather in the summer of 2023 may underlie this upsurge. The paper emphasizes that while significant efforts led to malaria’s elimination from the US in 1951, the persistence of *Anopheles* species means the threat of local transmission has not disappeared. With malaria still posing a severe health risk globally, vigilance and robust prevention strategies in the US are more critical than ever.
CDC Report on Malaria Outbreaks and Public Health Response
The CDC’s examination of the recent outbreaks reveals critical insights into the epidemiology of malaria in the United States. The report outlines the specifics of the individual cases, including geographical clustering in Sarasota County, Florida, which accounted for a majority of the local transmission instances. Public health actions were necessary, involving targeted insecticide spraying and community outreach, aimed at both controlling mosquito populations and informing residents about malaria prevention strategies. Alarmingly, all patients had spent considerable time outdoors during the nighttime, which aligns with peak activity periods for *Anopheles mosquitoes*, elevating their risk of transmission.
In response to the outbreaks, immediate actions were taken to ensure timely treatment and recovery of the affected individuals. Notably, the report highlights the significance of educational initiatives to equip healthcare providers with the skills to diagnose and manage malaria cases reliably. As local cases remain a concern, healthcare officials stress the importance of reporting and public communication, ensuring that vigilance against this mosquito-borne illness is maintained across communities.
The Role of Anopheles Mosquitoes in Malaria Transmission
Anopheles mosquitoes are crucial vectors in the transmission of malaria, acting as carriers of the parasite *Plasmodium spp*. Following the recent malaria cases in the US, studies revealed that *Anopheles crucians* mosquitoes captured in the affected regions were found to harbor *P. vivax* DNA, suggesting recent human infections. This highlights a significant gap in understanding the local *Anopheles* populations and their dynamics in transmitting malaria. Specifically, mosquito behavior patterns, demographics, and the ecological impacts of climate change must be studied further to grasp their role in malaria transmission effectively.
The effectiveness of prevention strategies hinges on understanding how local *Anopheles mosquitoes* interact with human populations and the environment. CDC efforts should involve comprehensive research into habitat mechanics and the efficacy of sprays or repellants in particular regions. Public awareness campaigns should also educate communities about mosquito behaviors to help mitigate exposure during mosquito peak activity times. Importantly, effective control strategies against local *Anopheles* populations can significantly reduce the risk of malaria transmission in both urban and rural settings.
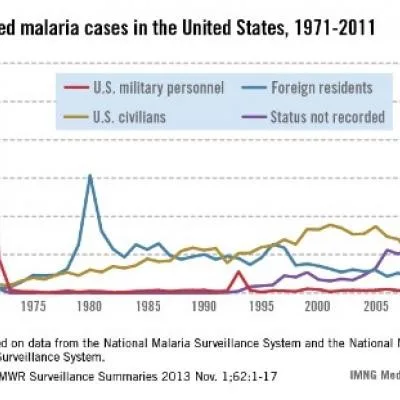
Imported Malaria Cases: A Growing Concern for the US
The rising trend of imported malaria cases in the United States poses a significant challenge to public health initiatives. Preliminary data for 2023 indicated a record high of 2,205 imported cases, primarily derived from travelers returning from malaria-endemic regions. States such as Florida, Texas, and Maryland, where recent locally transmitted cases were reported, are also among those experiencing the highest rates of imported malaria. These statistics signify an urgent need for enhanced screening and treatment options for travelers and returnees.
With the integration of global travel, the likelihood of malaria introduction into unaffected areas increases. To combat this, it is imperative for public health officials to reinforce malaria prevention strategies that include prompt diagnosis and prophylactic treatments prior to travel. The emphasis must be placed not only on treatment after manifestation but also on educating those traveling to high-risk regions about potential exposures and preventive measures. Such initiatives are critical in curbing the influx of imported malaria cases, which can lead to local transmission.
Climate Change’s Impact on Malaria Transmission Risks
As the latest CDC report indicates, the summer of 2023 marked one of the hottest periods on record in the United States, greatly influencing malaria transmission dynamics. Rising temperatures can enhance the breeding and survival rates of mosquito populations, particularly *Anopheles mosquitoes*, thus increasing the probability of local malaria outbreaks. Moreover, climate change variables such as precipitation patterns can create perfect breeding grounds for mosquitoes, contributing to the risk of local transmission of malaria.
Research underscores the need to investigate how environmental changes specifically affect malaria’s lifecycle and transmission potential. It is vital for health authorities to adapt their malaria prevention strategies to account for these fluctuations in climate. This includes tracking mosquito populations and adjusting control measures, such as the use of insecticides, based on real-time data regarding mosquito behavior and habitat shifts caused by climate changes.
Community Outreach and Education on Malaria Prevention
Effective response to malaria outbreaks requires not just strategic public health actions but also robust community outreach and education. Community engagement plays a pivotal role in informing individuals about the prevention strategies against mosquito bites and malaria transmission. Health departments can organize informational sessions and campaigns to distribute materials about the risks associated with *Anopheles mosquitoes*, focusing particularly on behaviors conducive to heightened risk, such as outdoor activities at night.
Moreover, providing access to resources such as bed nets and mosquito repellents can empower communities to take proactive stances against local transmission. Tailored educational programs can help raise awareness about the signs and symptoms of malaria, urging residents to seek timely medical advice and report any suspicious illnesses. Ultimately, fostering an informed public is essential for supporting community health initiatives and curbing the incidence of malaria nationally.
Key Malaria Prevention Strategies for Travelers
As highlighted in the recent CDC report on malaria outbreaks, travelers heading to malaria-endemic regions should prioritize proactive malaria prevention strategies. Completing a course of malaria chemoprophylaxis before, during, and after travel is crucial for mitigating the risk of infection. Individuals must consult healthcare professionals for personalized advice about the appropriate medications, considering factors such as destination, duration of stay, and personal health conditions.
In addition to chemoprophylaxis, travelers should also be educated on vector avoidance measures. This includes wearing long sleeves and using insect repellent containing DEET or Picaridin when outdoors, particularly in the evenings when *Anopheles mosquitoes* are most active. Emphasizing these strategies not only protects individual travelers but also reduces the likelihood of introducing malaria back into the United States, thereby safeguarding public health.
Implications of Local Transmission for US Public Health Policies
The recent locally transmitted cases of malaria in the US have significant implications for national public health policies. It is essential to analyze how these events can inform future disease surveillance and response strategies. Policymakers must understand that even with historical successes in eliminating malaria, the potential for re-emergence due to climate change and increased international travel necessitates continuous vigilance. A comprehensive approach that integrates localized mosquito control measures with global health initiatives can strengthen public health resilience.
Policymakers should work closely with the CDC and other health organizations to develop adaptive strategies that can respond to potential malaria outbreaks effectively. This includes expanding resources for training healthcare providers on rapid diagnosis and treatment protocols, enhancing laboratory capabilities for malaria testing, and fostering international collaborations to address global malaria challenges. As malaria cases emerge locally, reinforcing health system capacities becomes paramount for safeguarding communities and preventing possible future outbreaks.
Ongoing Research Needs for Understanding Malaria Dynamics
Continued research is vital to understanding the dynamics of malaria transmission, particularly in the context of recently reported locally transmitted cases. Investigating the genetic makeup of malaria parasites in *Anopheles mosquitoes* can yield insights into their origins and patterns of infection. This knowledge could guide targeted interventions to control and prevent outbreaks effectively. Furthermore, examining environmental factors contributing to the life cycle of *Anopheles mosquitoes* can enable public health officials to better predict and mitigate transmission risks.
Investing in research initiatives focused on local mosquito populations will aid in designing effective control strategies tailored to specific geographical areas. Expanding our knowledge in these areas could not only improve domestic malaria prevention but also contribute to global efforts in malaria eradication. Partnerships between universities, public health agencies, and international organizations can facilitate necessary studies on the impact of climate change, human behavior, and socio-economic factors on malaria transmission, ensuring that preventive measures remain effective in a changing world.
Frequently Asked Questions
What are the recent trends in locally transmitted malaria cases in the US?
Recent reports indicate a resurgence of locally transmitted malaria cases in the United States, particularly highlighted in a CDC report. For the first time in 20 years, 10 cases of malaria were documented from May to September 2023 across Florida, Texas, Arkansas, and Maryland, raising concerns among public health officials.
How does the CDC report malaria outbreaks in the US?
The CDC reports malaria outbreaks in the US by monitoring both imported and locally transmitted malaria cases, emphasizing rapid public health responses. The latest CDC report details 10 cases of locally transmitted malaria, the first since 2003, underlining the importance of vigilance due to increased travel and potential local transmission risks.
What caused the recent malaria outbreaks in the US?
The recent malaria outbreaks in the US were attributed to a combination of factors including increased imported malaria cases and high temperatures in 2023. These conditions may have facilitated local transmission, particularly involving *Anopheles* mosquitoes in states like Florida and Texas.
How are disease vectors such as Anopheles mosquitoes connected to US malaria cases?
Anopheles mosquitoes are the primary vectors for malaria transmission in the US. Recent locally transmitted cases were linked to this mosquito species, confirming the ongoing risk even with a history of malaria elimination in the country. Studies show these mosquitoes can carry *Plasmodium* parasites, leading to localized outbreaks.
What malaria prevention strategies are recommended following the recent outbreaks in the US?
In response to recent malaria outbreaks, public health officials recommend several malaria prevention strategies. Travelers should consider malaria chemoprophylaxis, and communities should engage in outdoor insecticide spraying, distribute bed nets, and use mosquito repellent to minimize exposure during peak *Anopheles* mosquito activity.
How does climate affect malaria transmission risks in the US?
Climate, particularly increased temperatures and rainfall, affects malaria transmission risks in the US by enhancing the breeding conditions for *Anopheles* mosquitoes. The hot summer of 2023 coincided with a spike in malaria cases, suggesting that warmer climates may lead to higher risks of locally transmitted malaria.
What steps can healthcare providers take regarding malaria cases reported in the US?
Healthcare providers can improve malaria management by ensuring timely diagnosis and treatment of suspected cases, reporting these incidents promptly to public health authorities, and providing patients with information related to malaria prevention strategies, especially for those who travel to endemic regions.
| Key Points | Details |
|---|---|
| Recent Locally Transmitted Cases | The first cases of mosquito-transmitted malaria in the US in 20 years have been reported, with 10 cases occurring in Florida, Arkansas, Texas, and Maryland. |
| Significance of Cases | Malaria was eliminated in the US in 1951, with the last local cases occurring in 2003. The recent increase raises concerns about re-establishment of malaria due to various factors. |
| Epidemiology of the Cases | Seven out of ten patients were from a 4-mile radius in Sarasota, FL, with *Plasmodium vivax* and *P. falciparum* identified in cases. |
| Public Health Response | Efforts included insecticide spraying, community outreach, and training for healthcare providers to manage and prevent further outbreaks. |
| Factors Contributing to Outbreak | Increased travel from malaria-endemic areas, a record of imported malaria cases, and rising temperatures have heightened the risk of local transmission. |
Summary
US malaria cases have seen an unexpected rise with the first documented local transmission in two decades, highlighting new public health challenges. Despite successful malaria elimination in 1951, the recent report from the CDC emphasizes the importance of vigilance against imported and locally acquired cases, particularly with increasing travel and vector populations. To prevent future outbreaks, strategies such as proper traveler precautions and enhanced monitoring of mosquito populations are essential.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.