US flu indicators have shown a notable decline for six consecutive weeks, as reported by the Centers for Disease Control and Prevention (CDC) in their latest flu activity update. Despite the drop, flu levels remain elevated across the nation, indicating that the virus’s impact is still being felt. Current data reveals that 3.3% of outpatient visits are attributed to flu-like illnesses, remaining above the national baseline, which has now persisted for 17 weeks. Although hospitalization rates and pediatric flu deaths are trending downward, the CDC confirmed eight new pediatric flu deaths, raising the total for the season to 159. As concerns about flu persist, juxtaposed against decreasing COVID-19 wastewater levels, monitoring these US flu indicators becomes essential for public health responses.
The latest updates on flu metrics in the United States illustrate a complex interplay between seasonal illness and ongoing public health challenges. Reports from health authorities indicate a sustained presence of influenza throughout the country, with significant attention on rising outpatient visits due to flu symptoms. Although hospitalization rates suggest a downward trend, the impact on vulnerable populations, particularly children, remains a critical concern, highlighted by recent fatalities. As we also observe the fluctuations in COVID-related wastewater levels, it’s crucial to continue monitoring both flu activity and respiratory virus trends to inform health directives and community awareness.
Current US Flu Indicators and Activity Trends
Recent data from the CDC indicates that while US flu indicators have shown a steady decrease for six consecutive weeks, flu activity remains elevated across the nation. The percentage of outpatient visits for flu-like illness is still reported at 3.3%, surpassing the baseline for the seventeenth week in a row. This sustained level of flu activity highlights ongoing concerns, even as certain regions report falling below their respective baselines, specifically five regions demonstrating lower flu-like visits.
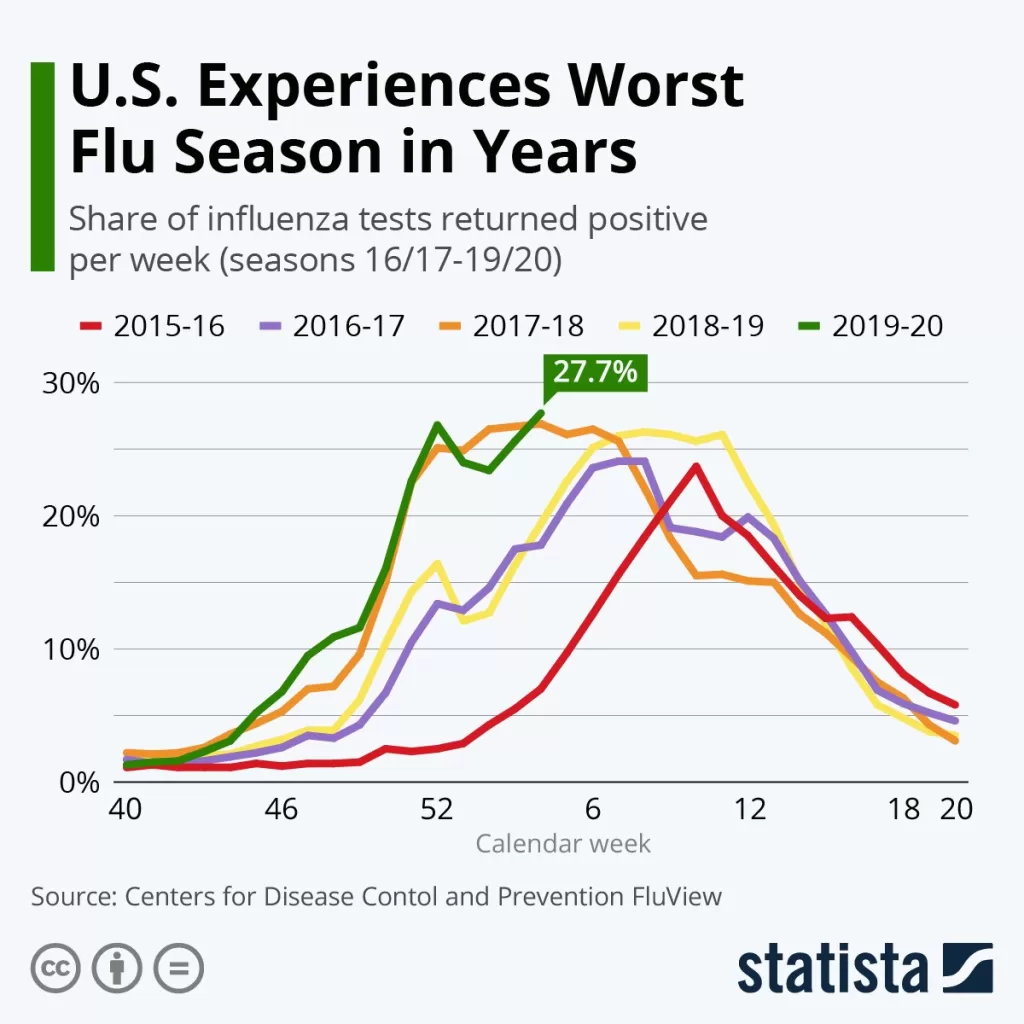
Moreover, it is notable that from the previous week, there has been a marked decline in jurisdictions reporting high or very high flu activity, dropping from twenty to just seven. Despite the positive trend, the overall test positivity rate for influenza is at 10.7%, down from 13.3%. The CDC has emphasized that this flu season has classified as high severity, with alarming statistics suggesting at least 44 million infections, which reinforces the importance of ongoing surveillance and public health measures.
Impact of Hospitalizations and Pediatric Flu Deaths
The impact of the flu season has been significant, particularly regarding hospitalization rates and pediatric flu deaths. The CDC’s latest report reflects a downward trend in hospitalizations and related deaths, a beacon of hope amid the high severity classification of this flu season. However, the report also confirmed eight additional pediatric flu deaths last week, bringing the total to 159 fatalities. This alarming statistic underscores the vulnerability of children to severe influenza infections and the necessity for targeted vaccination efforts and public awareness.
Families and healthcare providers alike must continue to stay informed about flu activity to better protect at-risk populations. With estimates of 580,000 hospitalizations attributed to influenza thus far, healthcare systems are still under significant strain. This situation highlights the need for proactive measures such as vaccination campaigns and public health advisories to mitigate further risks of severe illness associated with the flu, especially among children.
COVID Wastewater Levels and Their Implications
In a parallel development, the CDC has reported a decrease in COVID-19 levels, particularly evident in wastewater surveillance. This week, wastewater detections have reduced from a medium level to low, signaling a potential shift in the trajectory of COVID infections. The impact of these lower levels is crucial not only for public health officials but also for healthcare providers managing flu cases during this time. An effective surveillance system can aid in understanding the interplay between flu and COVID-19 outbreaks.
Notably, the proportion of overall deaths attributed to COVID last week stood at 0.9%, in contrast to the 1.5% related to influenza. This data suggests that while COVID-19 remains a significant concern, the flu’s impact on health outcomes is still paramount, particularly for vulnerable populations. As new variants, such as LP.8.1, continue to circulate, ongoing monitoring of wastewater and other indicators like hospitalization rates and flu activity updates will be essential for informing public health responses.
Pediatric Flu Deaths: A Growing Concern
The recent rise in pediatric flu deaths has raised alarms among health officials and parents alike. Totaling 159 for the season, these fatalities highlight the necessity of vigilance and immediate action, particularly as the flu’s impact on younger populations has proven severe. The CDC emphasizes that children under five are at greater risk, often requiring medical attention even for simple flu symptoms.
This situation calls for implementing preventive measures such as widespread vaccination among children and public education campaigns regarding flu symptoms and when to seek medical care. Healthcare providers play a critical role in early diagnosis and treatment, potentially reducing the risk of complications associated with influenza in pediatric patients.
Long-term Effects of Current Flu Season on Public Health
The ongoing flu season is likely to have long-term implications for public health strategies across the United States. With a reported 44 million infected individuals, the repercussions are not only immediate but also set the stage for future flu seasons. The severity of this year’s strain may influence vaccine development and public health policies aimed at preventing similar outcomes in subsequent years.
Additionally, the experience gained from this flu season could enhance preparedness for flu and influenza-like illnesses, particularly in the face of co-circulating viruses like COVID-19. Educational programs, increased vaccination awareness, and robust health surveillance systems will be essential as we navigate the complexities of public health challenges that span beyond individual seasons.
Understanding the Flu: CDC Reports and Updates
The CDC plays a pivotal role in monitoring flu activity across the United States, delivering regular reports and updates that inform public health policies and community health decisions. The most recent CDC flu report outlined the current landscape of flu activity, including hospitalization rates and pediatric deaths. Staying updated with these reports is important for healthcare providers, policymakers, and the general public to understand the seriousness of the situation.
By disseminating data on flu activity and its impact on various demographics, the CDC ensures timely responses can be coordinated, particularly in areas experiencing high transmission rates. Understanding these reports also aids in effectively communicating risks and safety measures to communities, potentially improving vaccination rates and flu prevention strategies.
Public Health Strategies in Response to Increased Flu Activity
In light of sustained high levels of flu activity, public health officials are urged to implement comprehensive strategies aimed at controlling the spread of influenza. Effective measures may include rolling out targeted vaccination campaigns, particularly in schools and daycare centers where pediatric flu deaths have been notably high. Engaging community health leaders in these campaigns can foster trust and encourage participation.
Moreover, public health messaging must be clear and persistent. Empowering individuals with knowledge about flu symptoms, the importance of vaccination, and when to seek medical advice is crucial. By maintaining open lines of communication and providing up-to-date information regarding flu activity updates, communities can be better prepared and more resilient in the face of seasonal influenza.
Importance of Vaccination During High Flu Seasons
Vaccination remains the most effective defense against influenza, especially during seasons characterized by high levels of flu activity. The CDC highlights that getting vaccinated not only protects individuals but also aids in community immunity, reducing transmission rates. With the current flu season being classified as high severity, prioritizing vaccination can mitigate the risks posed by the virus.
Additionally, healthcare providers should stress the importance of vaccinations for vulnerable populations, particularly children and the elderly who are at increased risk of severe flu complications. Public health initiatives focused on dispelling myths and emphasizing benefits can empower more people to take proactive steps in safeguarding their health.
Future Predictions for Flu Activity and Trends
As we analyze current flu indicators, it is essential to look towards future predictions regarding flu activity in the coming weeks. The CDC has indicated that flu activity is expected to persist, reinforcing the need for continued vigilance and preparedness among healthcare facilities. Understanding trends in seasonal flu can inform hospitals and clinics about expected patient loads and necessary resource allocation.
Moreover, as we observe the flu’s cyclical nature combined with the ramifications of the COVID-19 pandemic, public health experts will need to adapt their strategies continually. Future predictions will rely heavily on monitoring emerging flu strains, vaccination efficacy, and real-time data to tailor responses effectively, paving the way for a more prepared public health landscape.
Frequently Asked Questions
What are the key US flu indicators according to the latest CDC flu report?
The latest CDC flu report indicates that flu indicators show a declining trend for the sixth consecutive week, with outpatient visits for flu-like illness at 3.3%, remaining above the national baseline for 17 weeks. Hospitalizations and pediatric flu deaths also reflect a high severity flu season, with the total deaths reaching 159 this season.
How does the CDC flu report categorize current flu activity across the US?
According to the CDC’s flu activity update, while national flu indicators indicate a decrease, levels remain elevated. Only seven jurisdictions are reporting high or very high flu activity, a significant decline from 20 earlier. Regions with flu activity below their specific baselines have also increased.
What is the current state of pediatric flu deaths in the US according to the CDC?
The CDC reports an additional eight pediatric flu deaths this season, bringing the total to 159. This figure underscores the severity of the flu season, as indicated by the CDC’s classification of high severity for this flu season.
What trends are observed in hospitalizations and flu rates this season?
Recent CDC updates show that hospitalizations and flu rates are trending downward, even though the overall severity of the flu season remains high. The current test positivity rate for flu is 10.7%, down from last week’s 13.3%.
How do flu indicators compare to COVID wastewater levels according to the CDC?
The CDC has reported that COVID wastewater levels have dropped to low levels, contrasting with the ongoing situation with flu indicators. Last week, COVID-related deaths accounted for 0.9%, whereas flu deaths were at 1.5%, indicating that while both respiratory illnesses remain concerning, flu activity has had a greater death rate recently.
What is the projected impact of the current flu season based on CDC flu indicators?
The CDC estimates that the current flu season has resulted in at least 44 million infections and 580,000 hospitalizations, along with 25,000 deaths. These projections are based on ongoing surveillance and the data from US flu indicators.
| Indicator | Current Status | Notes |
|---|---|---|
| Flu-like Illness Outpatient Visits | 3.3% | Above national baseline for 17 weeks. |
| Regions Below Baseline | 5 | Significant drop in high activity regions. |
| High/Very High Flu Activity Jurisdictions | 7 | Down from 20 jurisdictions last week. |
| Test Positivity Rate | 10.7% | Decreased from 13.3% last week. |
| Pediatric Flu Deaths | 159 | 8 new deaths reported this week. |
| Total Estimated Infections | 44 Million | High severity classification by CDC. |
| Total Estimated Hospitalizations | 580,000 | Significant healthcare implications. |
| Total Estimated Deaths | 25,000 | Ongoing monitoring needed. |
Summary
US flu indicators have shown a decrease for the sixth consecutive week, yet they remain elevated on a national scale. Despite a downward trend in several metrics including hospitalization and death rates, some jurisdictions continue to experience high flu activity. This persistence highlights the need for continued public health vigilance and vaccination efforts to combat the ongoing flu season.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.