In the latest US flu activity update from the Centers for Disease Control and Prevention (CDC), influenza levels are notably low, continuing a trend of decline across the nation. Outpatient visits for influenza-like illness (ILI) have decreased from 2.1% to 1.9%, indicating a significant drop in flu-related health concerns. Hospitalizations also dropped, with the number of hospital patients down to 2,008, reaffirming the overall decrease in flu impact. Moreover, the test positivity rate for flu has fallen to 2.9%, providing a glimmer of hope as seasonal flu activity remains minimal. However, the report highlights a concerning statistic: the CDC confirmed one new H1N1 pediatric death this past January, bringing the total of such tragic losses during the 2024-25 season to 227, the highest since the 2009-10 outbreak, signaling the ongoing need for vigilance against influenza and its variants.
Currently, the state of influenza transmission across the United States shows promising signs of decline, as reflected in the fresh data from the CDC’s FluView report. The decrease in outpatient visitation rates for respiratory illnesses suggests a notable reduction in flu prevalence, with hospital admissions also experiencing a downward trend. Additionally, statistics reveal that the test positivity rate for flu has tapered, aligning closely with COVID-19 positivity rates, indicating a balanced landscape of respiratory illnesses. Despite this encouraging situation, there remains an urgent need to stay informed about pediatric fatalities linked to H1N1, which have reached the highest numbers since recent years. This comprehensive overview reflects the broader spectrum of public health concerns, including RSV activity and COVID-19 levels, emphasizing the interconnectedness of these respiratory viruses.
Current US Flu Activity Update
According to the latest FluView update from the Centers for Disease Control and Prevention (CDC), US flu activity is currently low and steadily declining. The percentage of outpatient visits for influenza-like illness (ILI) has dropped to 1.9% from 2.1% the previous week, signaling a continued reduction in flu’s impact on public health. Furthermore, the number of patients hospitalized with flu has also decreased significantly, falling from 2,336 to 2,008. This steady decline in flu activity is promising, especially as health officials monitor the overall respiratory illness landscape.
As part of the CDC’s report, it’s important to recognize that no states are currently reporting moderate to high ILI activity levels. The test positivity rate for influenza stands at 2.9%, showing a decrease from 3.6% the week prior. These statistics indicate that while influenza remains a concern, the severity of illness and hospitalizations is trending downward. With only one new flu-related pediatric death reported this season, totaling 227, the numbers reflect a significant improvement that warrants ongoing observation as we progress through the flu season.
Influenza Statistics and Pediatric Impact
The CDC’s influenza statistics reveal that the flu season has been unusual, with pediatric cases drawing particular attention. Notably, the number of pediatric deaths attributed to flu strains has reached 227 this season, marking the highest number of pediatric fatalities since the 2009-10 flu season when there were 288 deaths. This alarming statistic emphasizes the importance of widespread flu vaccinations and public awareness campaigns focusing on protective measures for children who are particularly vulnerable to severe flu outcomes.
The increase in H1N1-related pediatric deaths this season serves as a critical reminder of the persistent risks posed by influenza. The CDC’s continued surveillance of influenza statistics is vital for informing healthcare providers and the public about the seriousness of the situation, especially among children. Ongoing education about flu vaccinations and understanding the flu’s symptoms can help reduce further incidences and safeguard the health of children across the United States.
Furthermore, as the flu statistics evolve, it becomes essential to compare them with other respiratory illnesses to gain a clearer picture of public health. The CDC’s updates indicate that although COVID-19 levels have remained low, continuous tracking of respiratory syncytial virus (RSV) positivity rates alongside flu will provide more comprehensive insights into the health challenges faced during the cold months.
COVID-19 and Respiratory Illness Surveillance
As revealed in the CDC data updates, COVID-19 levels in the US continue to remain low, with stable mortality rates. Last week, the overall deaths caused by COVID-19 stayed at 0.6%, which is notably lower than the flu’s death percentage of 0.2%. Wastewater detections from various regions indicate a low presence of the virus, although areas like Louisiana are experiencing higher concentrations. This trend underpins the need for sustained surveillance of COVID-19, especially as comparisons are drawn with influenza and RSV.
The inclusion of respiratory illnesses such as RSV in the CDC reports is pivotal. National test positivity rates for COVID-19 (2.9%) are parallel to those for flu (2.9%), while RSV is notably lower at 0.9%. This parallelism reflects how the public health response needs to be comprehensive, addressing all respiratory illnesses as we navigate these challenging seasons. By understanding these patterns, healthcare systems can better allocate resources to manage outbreaks effectively.
RSV Positivity Rate Impact on Public Health
Respiratory Syncytial Virus (RSV) continues to be an important concern within the triad of respiratory illnesses examined by the CDC. Current RSV positivity rates are reported at 0.9%, demonstrating a relatively low but significant prevalence. Compared to both flu and COVID-19, RSV’s lower positivity rate may suggest some regions are experiencing a respite from this particular virus. However, as past seasons have shown, RSV can impact young children and the elderly severely, particularly in terms of hospitalization and healthcare burdens.
Addressing RSV actively is essential, especially during flu season when multiple illnesses collide. Public health agencies must encourage awareness of RSV symptoms and preventive measures, especially among child care providers and parents. The synergy between flu, COVID-19, and RSV data underscores the necessity for integrated approaches to respiratory illness management—encouraging vaccinations, promoting hygiene practices, and maintaining attention to community health outcomes across all age groups.
Vaccination Importance for Flu and RSV
As flu activity and RSV percentages fluctuate, the significance of vaccination becomes increasingly clear. The CDC emphasizes the need for annual flu vaccinations, not only to protect individuals but also to shield the most vulnerable populations, such as infants and older adults, from serious complications. Vaccination against flu and RSV can significantly cut down infection rates and prevent hospital visits, ultimately reducing the burden on healthcare systems during peak seasons.
Moreover, educating the public about vaccination benefits can lead to higher uptake rates. For the 2024-25 season, parents must be informed about the risks of pediatric deaths associated with flu and the role of vaccines in alleviating these risks. As we approach winter months, a combined effort to promote flu and RSV vaccines can help diminish the spread of both viruses, thereby enhancing community health security.
Flu Prevention Tips for Families
With flu activity currently on the decline, families can still implement preventative measures to stay healthy. Basic public health practices such as frequent handwashing, using hand sanitizers, and encouraging a flu vaccination for everyone in the household can greatly reduce the chances of flu transmission. Furthermore, families should discuss flu-related symptoms and recognize when to seek medical help, particularly concerning young children who may be at greater risk.
Additionally, creating a health-conscious home environment can go a long way. Ensuring proper ventilation, maintaining a balanced diet rich in vitamins and nutrients, and promoting regular sleep habits can bolster the immune system. By fostering health awareness and engaging in preventive behaviors, families can significantly mitigate their risk of flu and other respiratory illnesses this season.
Understanding Flu Season Dynamics
The dynamics of flu season can fluctuate greatly, influenced by various factors such as public health efforts, community behaviors, and viral mutations. The CDC’s real-time updates provide crucial insights that help healthcare professionals and the public understand when flu activity peaks and when to anticipate lower rates. This real-time data is essential for timely vaccination campaigns and public awareness initiatives aimed at reducing illness spread.
It’s also essential for local health departments to use these insights to prepare community resources, including clinics for vaccinations and testing centers for respiratory illnesses. Understanding flu season dynamics allows for optimized responses, helping mitigate impacts on healthcare systems while providing accurate information to the public for proactive health measures.
The Role of Public Health Messaging
Public health messaging plays a critical role in managing flu levels and educating the population on preventive measures. Clear and consistent communication from the CDC about flu activity, pediatric deaths, and vaccination information can empower individuals to make informed decisions regarding their health. Engaging educational campaigns can help dispel misinformation and promote understanding of the risks associated with both the flu and COVID-19.
Moreover, collaboration among community stakeholders, such as schools, healthcare providers, and local businesses, can amplify public health messages. Inspired by the challenges faced during the ongoing respiratory illness seasons, unified messaging can tremendously increase community awareness, encouraging collective action to combat flu and other viruses. Working together within communities can forge a path towards improved health outcomes and resilience against seasonal diseases.
Future Projections for Flu Activity
Looking ahead, the projections for flu activity will be shaped by current trends and pivotal public health strategies. The CDC will continue to monitor and assess the effectiveness of vaccines in relation to circulating strains of the virus. Future activity projections will depend on various factors, including vaccination coverage rates, public compliance with health guidelines, and the potential emergence of new variants.
Moreover, health systems are expected to remain vigilant to respond effectively to any spikes in flu activity, particularly as the cold months can usher in a co-circulation of multiple respiratory pathogens. This readiness can be paramount as healthcare infrastructure must remain equipped to handle peak demands, ensuring comprehensive care for all patients experiencing respiratory symptoms.
Frequently Asked Questions
What is the latest CDC flu report on US flu activity?
According to the latest CDC flu report, US flu activity is currently low and continuing to decline. The percentage of outpatient visits for influenza-like illness (ILI) decreased from 2.1% to 1.9%, and hospitalizations have also dropped significantly.
What are the current influenza statistics for pediatric deaths in the US?
The current influenza statistics indicate that there have been 227 pediatric deaths this season, the highest number since 2009-10. The latest victim was attributed to the H1N1 strain, highlighting the serious impacts of flu in children.
How does the US flu activity update relate to COVID-19 levels?
The US flu activity update reveals that while flu cases remain low, COVID-19 levels are also stable. Last week, COVID-19 hospitalizations and overall deaths were low, with only 0.6% of deaths attributed to COVID compared to 0.2% for flu.
What is the RSV positivity rate in the context of US flu activity?
In the context of US flu activity, the RSV positivity rate remains low at about 0.9%. This is in line with the CDC’s assessment that flu and COVID-19 test positivity rates are similar, both at approximately 2.9%.
Has the CDC reported any changes in flu-related hospitalizations?
Yes, the CDC has reported a decrease in flu-related hospitalizations, from 2,336 to 2,008 over the past week, indicating a continued downward trend in US flu activity.
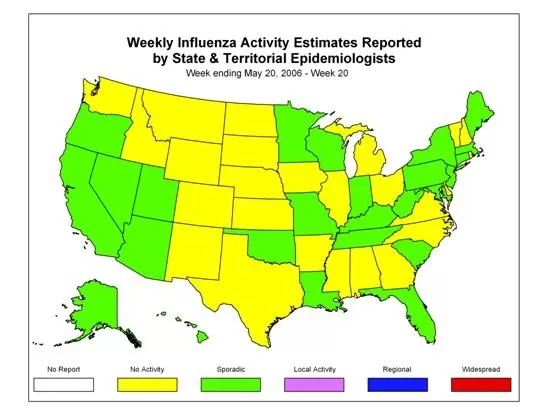
Are there any states reporting high influenza-like illness (ILI) activity?
No states are currently reporting moderate, high, or very high influenza-like illness (ILI) activity, as per the latest CDC update on US flu activity.
What should we know about the relationship between flu and COVID-19 levels?
The relationship between flu and COVID-19 levels shows that both remain low in the US, with similar test positivity rates of 2.9% each. The CDC highlights this in their updates on US flu activity and COVID-19 levels.
What is the significance of the latest flu activity update from the CDC?
The significance of the latest flu activity update from the CDC is that it reflects a reduction in both flu cases and hospitalizations, along with a concerning rise in pediatric deaths due to flu, particularly from the H1N1 strain.
| Key Point | Details |
|---|---|
| Flu Activity | US flu activity is low and continues to decline. |
| Outpatient Visits | Percentage decreased from 2.1% to 1.9%. |
| Hospitalizations | Hospitalizations decreased from 2,336 to 2,008. |
| ILI Activity | No states reported moderate or high ILI activity. |
| Test Positivity Rate | Decreased to 2.9% from 3.6%. |
| Pediatric Deaths | 1 new flu-related pediatric death confirmed, total of 227 for the season, highest since 2009-10. |
| COVID-19 Status | COVID-19 levels remain low; wastewater detections also low except for Louisiana. |
| Overall Death Rates | Deaths from COVID at 0.6% versus 0.2% for flu. |
| Test Positivity Rates for Respiratory Illnesses | Flu (2.9%), COVID (2.9%), RSV (0.9%). |
Summary
The US flu activity update indicates that flu cases are low and continue to decline, as per the latest report from the CDC. Key metrics, such as outpatient visits, hospitalizations, and flu test positivity rates, have all seen a decrease. Furthermore, fatalities related to flu remain concerning, particularly among children, highlighting the necessity for ongoing vigilance. Meanwhile, COVID-19 levels are stable, suggesting a dual focus needed on both flu and respiratory illnesses as we progress through the season.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.