US flu activity remains a significant public health concern as we move further into the flu season of 2025. Despite a decline in cases, the Centers for Disease Control and Prevention (CDC) reports that the severity of this season demands continued vigilance, particularly with 17 more pediatric flu deaths recorded recently. Influenza A has dominated the recent testing, making up a staggering 93.7% of the samples analyzed, further highlighting the 2009 H1N1 strain’s prevalence among cases. As the percentage of outpatient visits for flu-like illness hovers around the alarming 3.9% mark, it is crucial to stay informed through the latest CDC flu report. With expectations for ongoing flu activity in the coming weeks, understanding this season’s trends, including the impact on young patients, is vital for public awareness and safety.
As we analyze the current landscape of influenza in the United States, it is clear that flu outbreaks are shaping up to be a major topic of discussion this year. The recent trends in flu cases, particularly those caused by various strains of the influenza virus such as H1N1 and influenza B, warrant close attention. With pediatric flu deaths on the rise, the conversation around the health impacts of influenza in children becomes increasingly urgent. The continuing surveillance and findings from entities like the CDC will help in assessing the overall severity of the ongoing flu season. Monitoring these developments not only enhances our understanding of respiratory viruses but also aids in preparing for future outbreaks.
Understanding US Flu Activity Trends
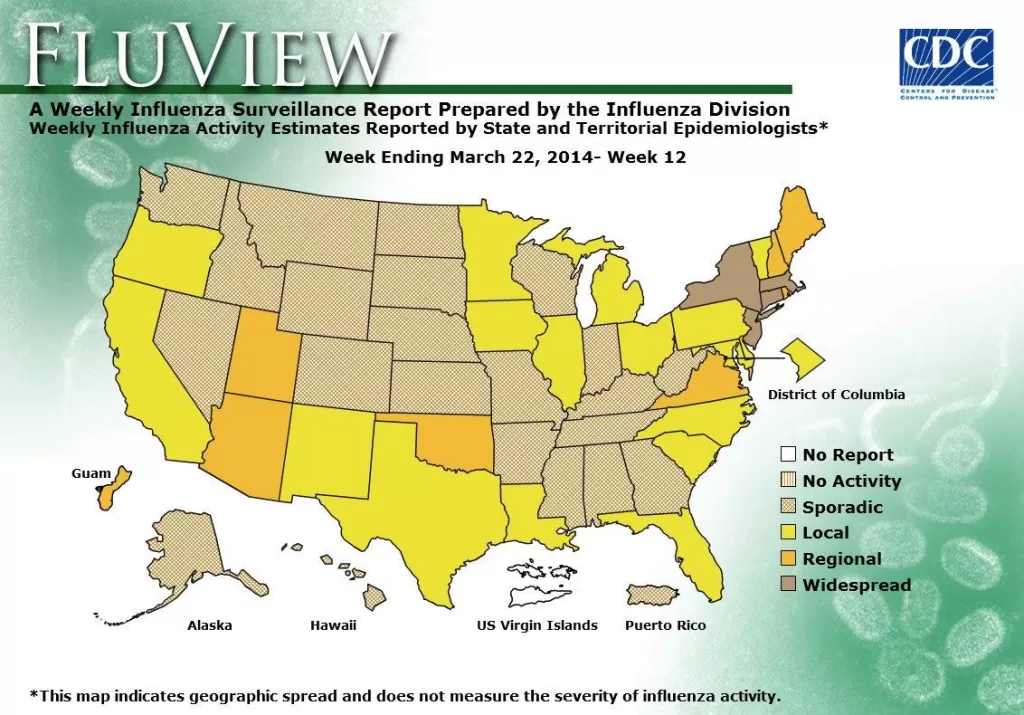
The recent data indicates a notable decline in US flu activity, which fell for the fifth consecutive week, a welcome trend for public health officials. As reported by the CDC, flu activity during flu season 2025 peaked earlier in the year, but the current levels suggest a gradual return to baseline, although the prevalence of flu-like illnesses remains above the normal threshold. This highlights the robust nature of influenza A, which makes up the majority of cases this season, particularly the H1N1 strain that has been prominently circulating.
Analyzing the overall impact of influenza on health systems, the decline in flu activity is encouraging; however, it does not signify the end of the flu season. The continued presence of flu-related hospitalizations and pediatric flu deaths underlines the need for vigilance. Public health messaging must focus on flu prevention strategies, especially in high-activity states, to reduce the risk of further complications as we approach the seasonal transitions.
Pediatric Flu Deaths: A Growing Concern
The rise in pediatric flu deaths has raised alarms among healthcare professionals, with 17 additional fatalities recorded in just one week. With a cumulative total of 151 pediatric deaths attributed primarily to influenza A, it is crucial for parents and caretakers to be aware of the symptoms associated with this viral infection. The CDC’s report emphasizes that children with underlying health conditions are particularly at risk, indicating that preventive measures, including vaccinations and timely medical interventions, are vital in safeguarding the health of vulnerable populations.
In previous flu seasons, pediatric deaths have been significantly higher, echoing concerns about the ongoing severity of this season’s flu activity. Given that the majority of recent fatalities resulted from the H1N1 strain, it is important to ensure that healthcare providers remain alert to the manifestations of both influenza A and B. Additionally, community outreach and education will play a critical role in addressing the factors contributing to pediatric flu hospitalizations and deaths, empowering parents with knowledge to seek necessary medical help.
The Role of Influenza A in the Current Season
Influenza A continues to dominate the current flu season in the US, accounting for over 93% of the confirmed cases as identified through public health lab testing. The prevalent subtypes, specifically the 2009 H1N1 strain, are under scrutiny as they contribute heavily to the ongoing hospitalizations and severe cases reported across different regions of the country. Despite a decline in overall flu activity, the virulence of influenza A highlights the need for ongoing surveillance and research into effective vaccination strategies.
As health professionals analyze the trends of influenza A infections, it becomes evident that people should remain cautious. The CDC’s continual observations of high positivity rates, especially around the northeastern states, signal that even as cases decline, the potential for outbreaks remains. Mitigating the spread of influenza A will require public compliance with health recommendations, timely vaccinations, and an understanding of the dynamics at play in flu transmission.
CDC Insights on Flu Season 2025
The CDC’s ongoing surveillance reports provide crucial insights into the dynamics of flu season 2025. Their latest findings highlight a marked reduction in outpatient visits for flu-like illnesses, confirming a downward trend in US flu activity. However, the data also underscores that while the flu season appears to be waning, it remains significant. Officials stress that influenza-related illnesses can still have serious implications, particularly as the public transitions from winter to spring.
In addition to chronicling the severity of influenza A and its subtypes, the CDC’s flu report informs preventive measures for the population. Their expectations for continued flu activity push for an increase in awareness regarding the importance of vaccination, especially for those at risk of severe illness. As testimonies from health professionals reflect the changing landscape of influenza dynamics, the CDC aims to provide the public with effective strategies to navigate the remaining weeks of flu season.
Emerging Challenges in Flu Response
As the US flu season progresses, there are emerging challenges that public health officials must address. The complexity of managing the dual threats of influenza and COVID-19 has put additional strain on healthcare resources, necessitating coordinated response strategies. The overlapping nature of these respiratory viruses requires continuous adaptation of public health messaging and resource allocation to safeguard the health of communities.
Given the substantial impact of influenza A, especially the H1N1 strain, in regions experiencing high hospitalization rates, it is essential for healthcare systems to implement adaptive responses. This may include evaluating vaccine distribution effectiveness and ensuring sufficient antiviral medications are available for high-risk populations. Understanding the interplay between different respiratory viruses can enhance outbreak preparedness and reduce the morbidity associated with flu seasons.
Health Recommendations During Flu Season
Public health authorities, including the CDC, provide vital health recommendations to navigate flu season safely. These emphasize the importance of getting vaccinated annually to reduce the risk of infection from influenza A and other strains. During flu season 2025, maintaining good hygiene practices such as thorough handwashing, using sanitizers, and avoiding close contact with infected individuals are all strategies encouraged to minimize flu transmission.
Moreover, health officials recommend that individuals exhibiting flu-like symptoms should seek medical attention promptly, especially if they are part of vulnerable demographics, such as young children or those with pre-existing health conditions. Adopting these recommendations can significantly improve outcomes and reduce pediatric flu deaths while also lessening the burden on healthcare systems still recovering from the challenges posed by the COVID-19 pandemic.
The Impact of Seasonal Transitions on Flu Spread
As the seasons change and we shift from winter to spring, the dynamics of flu spread often shift as well. Variations in temperature and humidity can influence virus survival and transmission rates, impacting public health outcomes. Understanding these seasonal trends is critical for health officials and communities to prepare for the potential resurgence of influenza A in areas previously experiencing declines in flu activity.
It’s important for stakeholders to remain proactive during transitional seasons. Public education campaigns can promote awareness concerning the importance of continued flu vaccinations and adherence to health recommendations even as the weather warms. Such proactive strategies can significantly mitigate the consequences of flu season and help in maintaining community health.
Vaccination Strategies to Combat Flu
With influenza A remaining a top contender in the flu season 2025, the emphasis on vaccination strategies becomes more pronounced. The CDC advocates for widespread vaccination as a primary defense against severe flu outcomes—especially given the high incidence of the H1N1 strain this season. Health providers are encouraged to promote flu vaccinations through community programs, with special attention to at-risk populations such as children and those with comorbidities.
In addition, enhancing public access to vaccines, along with ongoing educational efforts to dispel myths surrounding flu shots, can foster higher vaccination uptake. As studies demonstrate the effectiveness of vaccines in reducing hospitalizations and outbreaks, public health initiatives must ensure that every eligible individual is informed about the protective benefits and encouraged to get vaccinated before the season’s peak activity.
Analyzing Flu Hospitalizations Across the US
As reported in the latest CDC data, flu hospitalizations have reached alarming levels this season, reminiscent of figures not seen since the 2010-11 flu season. This surge is mainly attributed to the predominance of influenza A, with the H1N1 strain being the most frequently reported subtype responsible for severe cases. The pivotal information across various regions indicates that healthcare institutions must gear up for potential surges, particularly in areas still experiencing high flu activity.
Monitoring hospitalization trends allows public health authorities to adjust resources and enhance preparedness strategies accordingly. Establishing efficient communication channels between hospitals and local health departments can help streamline patient care and management during escalating flu activity. By sharing information on hospitalization rates and flu strain variations, healthcare providers can deliver targeted care for affected patients more effectively.
Public Awareness and Education on Flu Risks
Enhancing public awareness on the risks associated with influenza is critical during flu season 2025. Given the serious consequences of infections such as pediatric flu deaths, community outreach programs can serve an essential role in educating the public. By utilizing various platforms to disseminate risk information, health authorities can reach a broader audience, encourage vaccinations, and outline actionable steps to reduce flu transmission.
Furthermore, schools and workplaces can collaborate with health departments to facilitate educational initiatives that inform individuals about flu symptoms, prevention techniques, and when to seek medical help. Increased awareness not only bolsters individual health choices but also helps foster community resilience against flu outbreaks, ultimately contributing to lower rates of hospitalization and flu-related complications.
Frequently Asked Questions
What is the current status of US flu activity for the flu season 2025?
As of March 21, 2025, US flu activity has shown a decline for five consecutive weeks, although the Centers for Disease Control and Prevention (CDC) reports that it remains substantial. During this season, positivity rates for flu tests peaked at 31.6% but are currently at 13.3%.
How many pediatric flu deaths have been reported in the US during the current flu season?
In the current flu season, there have been 151 reported pediatric flu deaths in the US. Last week alone, the CDC reported 17 additional pediatric deaths, with the majority attributed to influenza A.
What strains of influenza are prevalent in the US flu activity this season?
This flu season, influenza A predominates, accounting for 93.7% of tested viruses. Among subtyped influenza A viruses, 57% are the H1N1 strain and 43% are H3N2, indicating a significant presence of various strains during the 2025 flu season.
How does the CDC monitor US flu activity during the flu season?
The CDC monitors US flu activity through weekly reports that include test positivity rates, hospitalizations, and mortality data. Their respiratory virus snapshot indicates expectations for ongoing flu activity for several more weeks even as hospitalization rates decline.
What are the implications of influenza A and B on pediatric flu deaths this season?
This season, the data show that 15 of the recent pediatric flu deaths were due to influenza A and 2 to influenza B. The prevalence of influenza A, particularly the H1N1 strain, has been a significant concern in relation to pediatric health during the flu season 2025.
Is the flu season 2025 more severe compared to past seasons in the US?
Yes, the flu season 2025 has been noted for its high severity, with hospitalization rates reaching the highest level since the 2010-11 flu season. While flu activity has started to decline, it has remained above average for several weeks.
Are flu-related hospitalizations in the US still a concern during the current flu season?
Yes, flu-related hospitalizations remain a concern during the current flu season. Although there has been a decline since mid-February, the rates are still high compared to previous years, emphasizing the ongoing impact of flu activity in the US.
| Key Point | Details |
|---|---|
| Flu Activity Decline | US flu activity has decreased for five consecutive weeks. |
| Recent Pediatric Deaths | 17 additional pediatric flu deaths reported, totaling 151 this season. |
| Test Positivity Rate | Peaked at 31.6% in early months, now at 13.3%. |
| Outpatient Visits for Flu-like Illness | Dropped to 3.9% but has been above the baseline for 16 weeks. |
| Flu Virus Distribution | 93.7% were influenza A viruses, with 57% being H1N1 strain. |
| Hospitalization Rate | Flu hospitalizations are the highest since the 2010-11 season. |
| Flu Activity Trends | CDC expects flu activity to persist for several more weeks. |
Summary
US flu activity has shown a continued decline over the past five weeks, yet it remains significant, particularly with recent pediatric flu deaths adding to concerns. Although the infection rates are decreasing, health authorities indicate that flu activity is likely to persist for some time. With continued monitoring and public health efforts, it is crucial to remain vigilant as we navigate the tail end of this flu season.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.