Understanding antibiotics is essential in today’s medical landscape, where the battle against antibiotic resistance poses significant challenges for healthcare systems worldwide. With the increasing prevalence of antibiotic misuse and its consequences, patients and providers must prioritize antibiotic safety and efficacy. This knowledge is vital not just for treating common conditions like urinary tract infections (UTIs), but also for preserving the gut microbiome’s health. As research evolves, the implications of antibiotic treatments continue to unfold, making it crucial for everyone to stay informed. This article will explore the latest developments, trends, and findings surrounding antibiotics to enhance our understanding and application of these powerful medications.
Exploring the realm of antimicrobial therapies sheds light on the pressing need for responsible antibiotic usage amidst growing concerns over drug resistance. The importance of comprehending these medications extends beyond mere treatment; it encompasses safeguarding our health and the integrity of our internal ecosystems. Understanding the nuances of antibiotic application is critical in managing infections effectively while minimizing adverse effects on the gut microbiome. As we delve into this topic, we will uncover alternative strategies and innovations in antibiotic treatment, particularly in the context of common ailments such as UTIs. By embracing this knowledge, we can better navigate the complexities of modern medicine and enhance our health outcomes.
Understanding Antibiotics and Their Importance
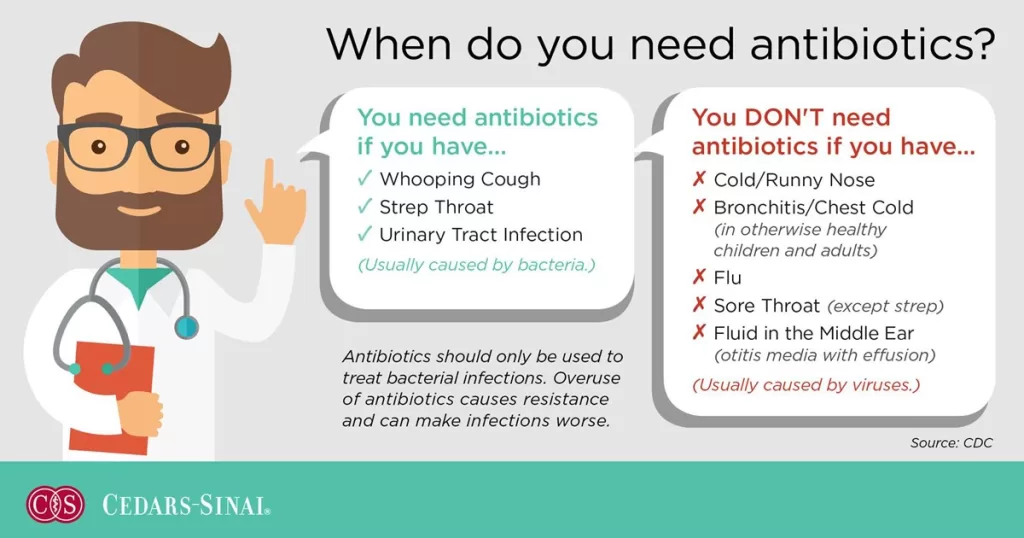
Antibiotics are powerful medications used to fight bacterial infections, but understanding their role in healthcare is essential for effective treatment. They work by either killing bacteria or inhibiting their growth, which helps the body to recover from infections. However, the misuse of antibiotics can lead to significant health issues, including antibiotic resistance, where bacteria evolve to survive despite the presence of these drugs. This phenomenon poses a considerable threat to global health, making it imperative for both patients and healthcare providers to be educated about the proper use of antibiotics.
Additionally, antibiotics can have unintended side effects, particularly on the gut microbiome, which is crucial for digestion and immune function. Disruption of the gut microbiome can lead to further health complications, including gastrointestinal distress and increased susceptibility to other infections. Therefore, understanding antibiotics not only encompasses their benefits in treating infections but also highlights the importance of using them judiciously to maintain overall health.
The Rise of Antibiotic Resistance
Antibiotic resistance is an alarming trend that has gained attention worldwide. As bacteria adapt to survive antibiotic treatment, the effectiveness of these crucial medications diminishes, leading to harder-to-treat infections. Statistics show that antibiotic resistance results in increased healthcare costs, prolonged hospital stays, and a higher mortality rate. Factors contributing to this phenomenon include over-prescription of antibiotics for conditions that may not require them, such as viral infections, and the improper use of antibiotics in both human and veterinary medicine.
Countries like India have reported a surge in drug-resistant infections, raising concerns among public health officials. This situation underscores the critical need for strict regulations regarding antibiotic prescriptions and the development of new treatment alternatives. Public awareness campaigns aimed at educating both healthcare professionals and patients about the risks associated with antibiotic misuse are essential in combating this rising threat.
Antibiotics and the Gut Microbiome
The gut microbiome plays a vital role in our overall health, influencing everything from digestion to immune response. Recent studies have shown that antibiotics, while effective against harmful bacteria, can also disrupt this delicate balance by killing beneficial bacteria. This disruption can result in a range of issues, including digestive problems and diminished immunity, making patients more vulnerable to infections. Researchers are now exploring ways to protect the gut microbiome during antibiotic treatment, which could improve patient outcomes and reduce the risk of complications.
Innovative therapies aimed at preserving gut health while administering antibiotics include the use of probiotics and prebiotics. These substances can help restore the balance of beneficial bacteria in the gut, potentially mitigating some of the negative effects associated with antibiotic use. As our understanding of the gut microbiome continues to evolve, it is becoming increasingly clear that maintaining its health is crucial for maximizing the benefits of antibiotic treatments.
Safe Antibiotic Practices
To ensure the safe use of antibiotics, it is vital for both patients and healthcare providers to adhere to best practices. This includes only using antibiotics when necessary, completing the full course of treatment as prescribed, and avoiding self-medication. By doing so, patients can help prevent the development of antibiotic resistance and safeguard their own health. Healthcare providers play a crucial role in this process by making informed decisions about prescribing antibiotics, taking into account individual patient needs and the specific nature of the infection.
Furthermore, continuous education on the potential side effects of antibiotics, including their impact on the gut microbiome and overall health, is essential. Patients should be encouraged to discuss any concerns with their healthcare providers, ensuring they have the information needed to make informed decisions about their treatment. By promoting safe antibiotic practices, we can collectively work towards minimizing the risks associated with antibiotic misuse and resistance.
Innovations in UTI Treatment
Urinary tract infections (UTIs) are one of the most common bacterial infections treated with antibiotics. Recent advancements in rapid testing technologies are promising improvements in the management of UTIs. For example, a new 15-minute testing system is being developed to quickly determine the appropriate antibiotic for treatment. This innovation aims to reduce the prevalence of antibiotic misuse by ensuring that patients receive the most effective medication based on their specific infection.
Moreover, understanding the natural course of UTIs has led to a more cautious approach in prescribing antibiotics. Research indicates that many UTIs can resolve on their own with proper hydration and care. This knowledge encourages healthcare providers to consider alternative treatment options before resorting to antibiotics, helping to preserve their effectiveness for future use and combat the growing issue of antibiotic resistance.
Frequently Asked Questions
What is antibiotic resistance and why is it a concern in understanding antibiotics?
Antibiotic resistance occurs when bacteria evolve to resist the effects of medications designed to kill them. This is a growing concern in understanding antibiotics as it complicates the treatment of infections, leading to longer hospital stays, higher medical costs, and increased mortality. Awareness of antibiotic resistance helps promote the responsible use of these medications.
How can antibiotic misuse affect my health and the gut microbiome?
Antibiotic misuse can disrupt the natural balance of bacteria in the gut microbiome, leading to adverse health effects such as diarrhea, yeast infections, and increased susceptibility to future infections. Understanding antibiotics includes recognizing the importance of using them only when necessary to preserve gut health and prevent resistance.
What are the safety precautions to take when using antibiotics?
When using antibiotics, it’s important to follow your healthcare provider’s instructions, complete the full course of treatment, and avoid combining them with alcohol unless advised. Understanding antibiotics also involves being aware of potential side effects and the risks of antibiotic resistance, ensuring safer use.
How are urinary tract infections (UTIs) treated with antibiotics, and what innovations are being made?
UTIs are commonly treated with antibiotics like nitrofurantoin, but recent innovations include rapid testing systems that ensure proper antibiotic prescriptions. Understanding antibiotics in the context of UTI treatment emphasizes the importance of accurate diagnosis to reduce misuse and improve outcomes.
What recent developments have been made in antibiotic research related to safety and efficacy?
Recent developments in antibiotic research focus on improving safety and efficacy, including recalls of certain antibiotics due to safety concerns and studies on protecting the gut microbiome from the negative effects of antibiotics. Understanding antibiotics means staying informed about these developments to ensure effective and safe treatment.
| Key Points | Details |
|---|---|
| Introduction | Understanding antibiotics is crucial due to antimicrobial resistance and evolving treatment options. |
| Recent Trends and Findings | 1. Some antibiotics negatively affect gut, brain, and skin health. 2. Rising drug-resistant infections reported in India. 3. FDA recalls antibiotics for pneumonia and bronchitis due to safety concerns. 4. New therapies are being researched to protect gut microbiomes during antibiotic use. 5. Rapid testing for UTIs to ensure proper antibiotic prescriptions is being developed. |
| Common Antibiotics for Conditions | 1. UTIs: Nitrofurantoin; some resolve without antibiotics. 2. Sinus Infections: Amoxicillin; avoid unnecessary prescriptions. 3. Pneumonia: Critical treatment with appropriate antibiotics. 4. Strep Throat: Treated with Penicillin or Amoxicillin. |
| Alcohol and Antibiotics | Alcohol can reduce antibiotic efficacy and increase side effects; patients advised to abstain. |
| Veterinary Concerns | Increased market for veterinary antibiotics due to pet ownership; proper prescribing is essential. |
Summary
Understanding antibiotics is vital for patients and healthcare providers alike, especially in light of the increasing threats posed by antimicrobial resistance. This topic encompasses the latest trends in antibiotic research, the implications of antibiotic use, and the importance of proper prescriptions. It is essential to stay informed about how antibiotics can affect health, the potential risks associated with their use, and the innovative strategies being developed to enhance treatment efficacy while minimizing harm. As we continue to navigate the complexities of antibiotic management, ongoing education and awareness will play a critical role in ensuring safe and effective healthcare practices.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.