Tularemia epidemiology is crucial for understanding the spread and impact of this zoonotic disease caused by *Francisella tularensis*, which significantly affects both human and animal populations. In recent years, particularly during 2021, Germany reported a notable increase in tularemia cases, highlighting its persistence in regions like Baden-Wuerttemberg. This area has become a focal point for studying tularemia transmission routes, as various studies have documented the pathogen’s genetic diversity. As arthropod bites constitute a primary route of infection for humans, examining these transmission dynamics is essential for public health surveillance. Overall, insights into tularemia epidemiology not only inform local health strategies but also raise awareness about zoonotic diseases Germany faces.
The study of tularemia, a disease linked to the bacterium *Francisella tularensis*, reveals significant epidemiological patterns that affect wildlife and human health alike, particularly in specific regions like Baden-Wuerttemberg. Understanding the transmission pathways of this zoonotic infection, alongside analyzing the genetic variation of the pathogen, provides pivotal insights into its behavior and spread. Recent statistics underscore alarming increases in tularemia cases, especially noted in 2021, which necessitates immediate attention from public health authorities. Surveillance in both animal populations and human cases is critical to accurately mapping the risk factors associated with this disease. Thus, a comprehensive examination of tularemia epidemiology is not only relevant for immediate public health responses but also for advancing research into the complexities of zoonotic diseases.
Understanding Tularemia Epidemiology in Baden-Wuerttemberg
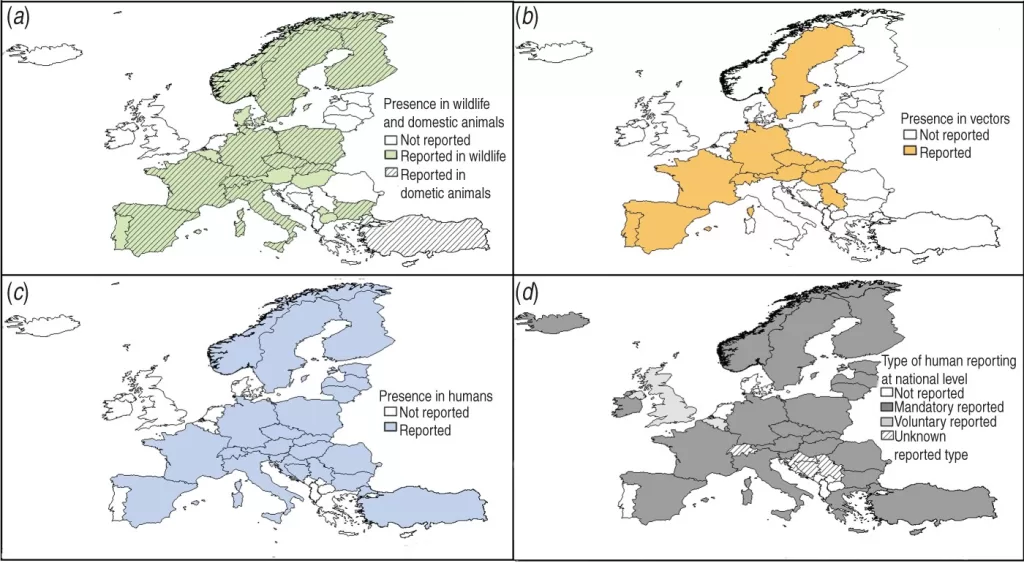
Tularemia, driven by the bacterium *Francisella tularensis*, has garnered attention across Europe due to its significant impact on both animal and human health. In the specific case of Baden-Wuerttemberg, the epidemiology of tularemia reveals crucial insights into how this zoonotic disease propagates in the region. An analysis conducted over the decade from 2012 to 2022 indicates that the disease is primarily transmitted to humans through direct exposure to infected animals, particularly brown hares, which serve as a major reservoir. The findings from our genomic studies show that human and animal strains often exhibit a remarkable genetic correlation, suggesting shared transmission routes and complicating efforts to delineate precise vectors of infection.
The overall increase in reported tularemia cases, notably peaking in 2021, highlights a growing concern among public health officials. Surveillance data indicates that human cases predominantly arise from environmental interactions, including bites from infected arthropods, which were reported in a significant 45% of the analyzed cases. Moreover, fluctuations in animal positivity rates, particularly among hares, underscore the need for ongoing monitoring as ecological conditions may continue to influence the dynamics of tularemia transmission.
Further understanding tularemia epidemiology requires a concerted effort in both veterinary and human health sectors. Collaborative research initiatives that leverage whole-genome sequencing of *Francisella tularensis* strains collected from diverse sources—including wildlife, agricultural settings, and human cases—can provide an integrated perspective to combat this zoonotic threat. Additionally, expanding public health awareness campaigns about tularemia transmission routes can empower communities to engage in preventive measures, especially in rural areas where human and wildlife interactions are more pronounced.
Transmission Routes of Tularemia: Key Insights
The transmission routes of tularemia are multifaceted, highlighting the complexities associated with controlling this infectious disease. Humans can contract tularemia through various means, including direct contact with infected animals, inhalation of aerosolized bacteria, and bites from infected arthropods, such as ticks and fleas. The predominance of arthropod-mediated transmission, particularly noted in the case studies from Baden-Wuerttemberg, reinforces the importance of understanding ecological dynamics that facilitate these interactions. As climate conditions become more favorable for these vectors, the risk of rapidly escalating tularemia cases rises, necessitating increased vigilance from public health authorities.
Recent data suggests a significant uptick in tularemia cases directly linked to increased environmental exposure during warmer months, when engagement with wildlife is at its peak. Notably, individuals involved in outdoor activities such as hunting, hiking, and farming are at a heightened risk. This fact underscores the necessity of informing the public about preventive strategies, including protective clothing and prompt reporting of animal deaths or unusual symptoms among wildlife, to intercept the potential spread of *Francisella tularensis*.
Mitigating the transmission of tularemia also requires examining the interplay between wildlife populations and their habitats. The persistent rise in positivity rates among animal populations, particularly brown hares, serves as an alarming indicator of changing ecological conditions potentially fueled by urban expansion and habitat modification. As wildlife habitats are altered, the interaction between humans and infected animals can lead to increased spillover events. Surveillance efforts should, therefore, not only focus on human cases but also include comprehensive monitoring of animal populations, enhancing our understanding of the ecological underpinnings of tularemia transmission.
The Clinical Manifestations of Tularemia: What to Watch For
Clinical manifestations of tularemia can vary widely among affected individuals, making it a challenging disease for early diagnosis. Common symptoms often include fever, lymphadenopathy, and ulcers that develop at the site of infection, particularly in glandular and ulceroglandular forms. The variability in presentation, combined with the relatively low incidence of tularemia, frequently leads to misdiagnosis or underreporting of the disease. During peak years of transmission in Baden-Wuerttemberg, particularly 2021, healthcare providers noted a marked increase in these presentations, indicating a pressing need for heightened awareness within clinical settings.
Moreover, the symptomatology associated with tularemia can reflect the transmission route, with pulmonary manifestations arising in cases of inhalation exposure. This underscores the importance of understanding the different clinical forms of the disease, helping healthcare professionals differentiate tularemia from other zoonotic diseases in Germany and ensuring timely and appropriate treatment. Early identification and treatment with antibiotics, such as streptomycin and gentamicin, significantly improve patient outcomes and reduce complications.
Recognizing tularemia symptoms is essential for controlling outbreaks and providing effective patient care. Given the legal requirements for reporting infectious diseases in Germany, awareness can enhance public health responses to emerging cases. The role of educational initiatives cannot be understated; as healthcare providers become more familiar with potential signs of tularemia, they can promote better community interactions with wildlife and encourage safer outdoor practices. This proactive approach to disease management can significantly impact the trajectory of tularemia cases and provide insights into broader zoonotic disease trends affecting regional health.
The Role of Surveillance in Tularemia Management
Surveillance plays a critical role in managing tularemia and other zoonotic diseases, providing essential data to public health authorities. In Baden-Wuerttemberg, enhanced surveillance strategies have been employed to track the incidence and spread of tularemia among both humans and animal populations. By integrating human health data with veterinary monitoring systems, public health officials can identify trends and potential outbreaks more effectively. This also allows for a better understanding of the epidemiology of *Francisella tularensis* and its transmission dynamics in various environmental contexts.
The analysis of data from 2012 to 2022 illustrates significant variations in human tularemia cases, notably a peak in 2021. Surveillance systems that utilize technologies such as whole-genome sequencing provide in-depth insights into the genetic diversity of the pathogen, facilitating targeted interventions and public health responses. By employing a multidisciplinary approach that includes veterinary expertise, environmental monitoring, and genomic research, the challenges posed by tularemia can be systematically addressed.
Strengthening surveillance systems, however, comes with challenges, such as underreporting due to low awareness and testing limitations among healthcare providers. Fostering collaboration between public health entities and local communities is vital in addressing these barriers and ensuring comprehensive data collection. Enhancing case detection methods and fostering educational outreach about tularemia can lead to better reporting practices, ultimately stabilizing and reducing tularemia cases in Baden-Wuerttemberg. As surveillance continues to evolve, it will play a decisive role in not only managing tularemia but also informing broader strategies for controlling other emerging zoonotic diseases.
Environmental Factors Influencing Tularemia Transmission
Environmental factors significantly influence the transmission dynamics of tularemia, particularly in regions like Baden-Wuerttemberg, where interactions between wildlife, vector populations, and human health are closely interconnected. Changes in land use, climate variability, and ecological disturbances can alter habitat suitability for both *Francisella tularensis* carriers and their vectors, such as ticks and fleas. For instance, as urban development encroaches into natural habitats, wildlife populations may increasingly come into contact with humans, escalating the risk of disease spillover. This ecological interplay highlights the necessity for integrated environmental monitoring as part of tularemia management strategies.
Furthermore, seasonal factors contribute heavily to tularemia transmission patterns. In Baden-Wuerttemberg, human cases tend to rise during warmer months when outdoor activities peak, coinciding with increased arthropod activity. Identifying such patterns enables public health officials to formulate timely interventions and raise awareness of preventive measures during high-risk periods. Environmental conditions thereby serve as both catalysts for disease emergence and critical determinants of community health outcomes.
Climate change further accentuates the need to understand environmental factors concerning tularemia transmission. As temperatures rise and precipitation patterns shift, the habitats of carriers and vectors change, ultimately influencing their populations and interactions with humans. Surveillance programs that incorporate environmental data can provide valuable insight into how these factors may correlate with rising tularemia cases. This knowledge is crucial for adapting public health responses and formulating proactive strategies to mitigate risks associated with climate-induced changes in disease dynamics.
Genetic Insights into *Francisella tularensis* Epidemiology
Whole-genome sequencing of *Francisella tularensis* is redefining our understanding of tularemia epidemiology in Baden-Wuerttemberg. This advanced genetic analysis provides a comprehensive perspective on the diversity and pathogenicity of various strains, allowing researchers to pinpoint genetic variations that may predispose certain isolates to more virulent or transmissible forms. By mapping the genetic relationships between human and animal strains of *F. tularensis*, insights into transmission routes can be bolstered, paving the way for more targeted public health interventions.
In the context of this research, genetic clustering observed among human isolates mirroring those derived from hare populations suggests a direct link, underscoring the role of wildlife in tularemia transmission. Understanding these genetic dynamics is crucial for informing surveillance protocols, providing a detailed framework for tracking disease outbreaks as they occur. Enhanced genomic resources also allow for a more nuanced approach to managing tularemia cases based on the specific dynamics observed in local populations.
Additionally, genomic insights inform stakeholders about potential reservoirs and environmental pressures that might shape the epidemiology of tularemia. As surveillance and sequencing technologies improve, the ability to detect shifts in strain prevalence in tandem with changing environmental conditions can lead to early warning systems for public health officials. Such proactive measures enhance community resilience against tularemia and other zoonotic diseases, illustrating the value of integrating genetics into overall epidemiological frameworks for disease management.
Community Engagement in Tularemia Prevention
Community engagement is pivotal in the prevention of tularemia, especially in areas where human-animal interactions are frequent. In Baden-Wuerttemberg, fostering community awareness about the risks associated with tularemia transmission can significantly reduce incidence rates. Educational campaigns focusing on protective measures during outdoor activities, such as wearing appropriate clothing and managing wildlife encounters, help empower citizens to protect themselves against zoonotic diseases effectively. Furthermore, community-driven surveillance efforts, where local populations volunteer for reporting and monitoring wildlife health, can bolster the data available for public health officials, creating a comprehensive picture of tularemia dynamics in real-time.
Moreover, schools can play a critical role in disseminating information regarding tularemia and its prevention. Curriculum enhancements that include zoonotic diseases and public health education can prepare future generations to engage responsibly with their environments and wildlife. By embedding knowledge at the community level, health authorities can foster a culture of prevention, enhancing the community’s response to potential tularemia outbreaks.
Engaging public health stakeholders in open dialogues with community representatives can further refine prevention strategies tailored to specific local contexts. Stakeholders can gather feedback on the effectiveness of current public health messages and work collaboratively to identify gaps in knowledge or resources. This cooperation fosters trust between health authorities and community members, facilitating proactive measures that may deter infection among high-risk groups. By promoting a shared responsibility for tularemia prevention and surveillance, communities in Baden-Wuerttemberg can enhance their resilience against this re-emerging zoonotic threat.
Future Directions in Tularemia Research and Surveillance
The future of tularemia research and surveillance in Baden-Wuerttemberg promises exciting advancements as new methodologies and technologies are integrated into public health frameworks. The application of genomic epidemiology, coupled with spatial analysis, can enhance our understanding of the burgeoning dynamics of tularemia transmission within communities. Ongoing research initiatives aim to further elucidate the ecological factors underlying the transmission of *Francisella tularensis*, enabling a more effective response to the re-emerging threats posed by this zoonotic disease.
Additionally, further studies are necessary to explore the environmental factors contributing to the increased positivity rates in animal populations and their implications for human health. As the relationship between climate change and disease emergence becomes more pronounced, researchers must investigate how alterations in ecosystems affect the prevalence of tularemia in wildlife, which can ultimately inform veterinary and public health strategies.
Investing in advanced training and resources for healthcare practitioners on zoonotic diseases and tularemia, in particular, will be crucial in sustaining momentum-for discovery and intervention. Tailoring research agendas to include interdisciplinary partnerships involving ecologists, veterinarians, and public health professionals can foster holistic approaches to managing zoonotic threats like tularemia. By enhancing collaborative efforts, we can expect to see improved surveillance systems, leading to a better understanding of *Francisella tularensis* epidemiology and its implications for both human and animal health.
Frequently Asked Questions
What is the epidemiology of Tularemia caused by Francisella tularensis in Baden-Wuerttemberg, Germany?
The epidemiology of Tularemia in Baden-Wuerttemberg, Germany, highlights a significant prevalence of the disease caused by *Francisella tularensis*. Between 2012 and 2022, there were 152 reported human cases, with the highest incidence occurring in 2021, which saw 34 cases. The infection is particularly linked to brown hares, serving as a primary transmission source for humans.
What were the main transmission routes of Tularemia in the reported cases for 2021?
In 2021, the primary transmission routes of Tularemia included arthropod bites, which accounted for 45% of cases with documented animal exposure. Additional transmission routes remain unclear, highlighting the need for further epidemiological investigation into how *Francisella tularensis* spreads between humans and animals.
How did Tularemia cases trend in Baden-Wuerttemberg from 2012 to 2022?
From 2012 to 2022, Tularemia cases in Baden-Wuerttemberg exhibited a significant increasing trend, particularly notable in 2021. Poisson regression analysis indicated a statistically significant rise in human cases (p<0.001), although no seasonal pattern was identified, with the lowest cases recorded during winter.
What role do brown hares play in the epidemiology of Tularemia in Germany?
Brown hares are critical in the epidemiology of Tularemia in Germany, especially in Baden-Wuerttemberg, where they are the predominant reservoirs for *Francisella tularensis*. The genetic analysis of human isolates often shows clustering with hare-derived strains, supporting the hypothesis of their role in disease transmission to humans.
What are the symptoms commonly observed in human cases of Tularemia in Baden-Wuerttemberg?
Common symptoms in human cases of Tularemia reported in Baden-Wuerttemberg include fever and lymph node swelling. Patients typically present with glandular and ulceroglandular forms of the disease, reflecting its various clinical manifestations.
Are there differences in Tularemia prevalence among animal populations in Baden-Wuerttemberg?
Yes, there are notable differences in Tularemia prevalence among animal populations in Baden-Wuerttemberg. The positivity rates in animal testing fluctuated between 5% and 34% from 2012 to 2022, with an increasing trend noted since 2017, particularly among brown hare populations.
What methods are used to track the epidemiology of Tularemia in Baden-Wuerttemberg?
The epidemiology of Tularemia in Baden-Wuerttemberg is tracked using a combination of human and veterinary surveillance data, alongside whole-genome sequencing. These methods help characterize the genetic diversity of *Francisella tularensis* and assess correlations between human and animal cases.
How can genomic analysis improve the understanding of Tularemia epidemiology?
Genomic analysis enhances the understanding of Tularemia epidemiology by identifying the genetic variations of *Francisella tularensis* strains found in humans and animals. This information is crucial for understanding evolutionary relationships, transmission dynamics, and informing public health interventions.
| Aspect | Findings |
|---|---|
| Distribution | Tularemia is endemic in Baden-Wuerttemberg, Germany. |
| Human Cases | 152 reported cases from 2012 to 2022, with a spike in 2021 (n = 34). |
| Transmission Sources | Human cases often linked to arthropod bites and hare exposure (45% with animal exposure details). |
| Trends | Significant increase in cases (p<0.001) over time; no seasonal pattern, lowest in winter. |
| Animal Positivity Rates | Fluctuating rates between 5%-34%, increasing since 2017, particularly in brown hares. |
| Genetic Analysis | Human isolates clustering with hare-derived strains; genomic analysis shows phylogenetic similarities. |
| Public Health Recommendations | Improved coordination between public health and veterinary services; enhanced surveillance needed. |
Summary
Tularemia epidemiology in Baden-Wuerttemberg highlights a complex interaction between wildlife, environmental factors, and human health. Insights from the study indicate a concerning rise in human cases primarily linked to animal exposure and environmental conditions, particularly affecting brown hares as a key transmission vector. Furthermore, the study underscores the potential of genomic tools to enhance disease tracking, aiding public health initiatives to better mitigate this re-emerging zoonotic threat.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.