In recent weeks, a surge of concern has arisen regarding sexually transmitted fungal infections, particularly as New York reports four confirmed cases linked to the increasingly recognized pathogen Trichophyton mentagrophytes. This sexually transmitted organism is responsible for conditions such as genital tinea—often categorized within the broader scope of fungal infection symptoms. Men aged 30 to 39 were primarily affected, illuminating the need for heightened STI awareness among sexually active individuals. Not only does this case highlight the potential for fungal infections to transmit through sexual contact, but it also underscores the significance of prompt genital tinea treatment. As our understanding of ringworm in men evolves, the medical community is urged to remain vigilant in recognizing and addressing these infections to prevent further spread.
The recent identification of a novel type of fungal infection, particularly those related to sexual activities, emphasizes the importance of awareness surrounding dermatophyte transmission. Often misunderstood, these infections, commonly linked to genital tinea and its symptoms, can significantly impact men’s health, especially in urban settings. Awareness campaigns targeting vulnerable populations, including men who have sex with men, are essential for prevention and prompt treatment. Understanding the implications of conditions such as ringworm, typically regarded as benign, when contracted during sexual intercourse is crucial for both public health officials and community members alike. The emergence of Trichophyton mentagrophytes as a sexually transmitted fungus serves as a timely reminder to prioritize education and early intervention in combating fungal infections.
Understanding Sexually Transmitted Fungal Infections
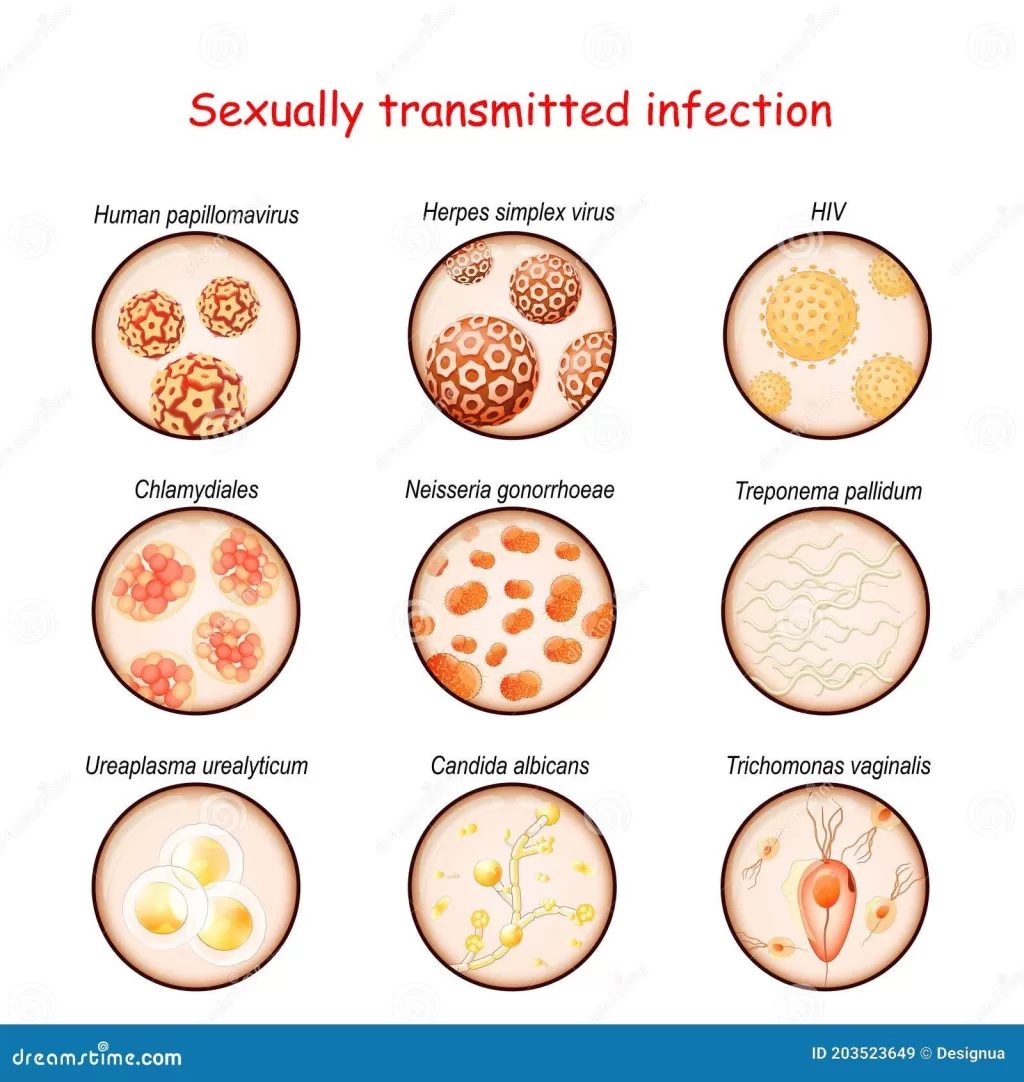
Sexually transmitted fungal infections, although less frequently discussed than bacterial or viral STIs, are becoming a greater concern in public health. One such infection is caused by Trichophyton mentagrophytes type VII (TMVII), which can lead to genital tinea, more commonly known as ringworm. The recent identification of TMVII infections among men who have sex with men (MSM) and those with multiple sexual partners highlights the need for increased awareness and education on this topic.
Fungal infections can often present symptoms that may be mistaken for other conditions. For instance, individuals infected with TMVII might exhibit rashes on the face, buttocks, or genitals, which can lead to misdiagnosis if healthcare providers are not well-informed about this specific pathogen. Therefore, it is essential that both healthcare providers and patients recognize the signs and symptoms associated with sexually transmitted fungal infections to facilitate prompt diagnosis and treatment.
Symptoms of Fungal Infections: Recognizing the Signs
With sexually transmitted fungal infections, the symptoms can vary based on the area of the body affected. In many cases, the presence of rashes or lesions will be the first indicative sign, particularly in the genital area, buttocks, or trunk. In the cases reported in New York City, all affected individuals presented with such rashes, which necessitated further evaluation to determine the underlying cause.
Other symptoms accompanying fungal infections might also include itching, redness, or discomfort in the affected areas. Effective recognition of these symptoms is crucial, not just for initial treatment but also to prevent the further spread through intimate contact. Increased public awareness around these symptoms can significantly contribute to better STI awareness and encourage individuals to seek medical help without stigma.
Drugs and Treatments: Genital Tinea Management
The treatment of genital tinea, particularly when caused by Trichophyton mentagrophytes, typically involves antifungal medications, which have proven effective in eradicating the infection. The four men treated in New York City were successfully managed with the right antifungal therapy, which highlights the importance of prompt and appropriate medical intervention following diagnosis.
It is crucial for healthcare providers to not only prescribe antifungal medication but also to educate patients about proper hygiene and preventive measures. This education can help reduce the risk of reinfection and transmission. For instance, avoiding direct skin-to-skin contact with affected areas and adhering to treatment regimens are vital components in the effective management of genital tinea and related fungal infections.
The Role of Public Health in Managing STIs
Public health initiatives play an essential role in the management of sexually transmitted infections, including emerging fungal infections like TMVII. Surveillance, education, and awareness campaigns can significantly enhance early detection and treatment, thus preventing further spread. Increasing healthcare provider knowledge through continuous medical education can ensure that these infections are diagnosed and treated appropriately.
Moreover, public health strategies must focus on providing accessible and informative resources for at-risk populations. Barriers preventing individuals from discussing their sexual health openly or seeking care must be addressed to ensure that everyone has the tools they need to protect themselves and their partners.
Trichophyton mentagrophytes: An Emerging Threat
The emergence of Trichophyton mentagrophytes type VII as an infectious agent poses a new threat in terms of sexually transmitted infections. Previously more common in specific geographic areas, it is now making its way into urban centers like New York, where sexual activities may facilitate its spread. This change necessitates new approaches in STI awareness, focusing on not only traditional bacterial and viral pathogens but also on fungal pathogens that may have similar transmission routes.
As TMVII infections are primarily reported among men who have sex with men and individuals with multiple sexual partners, targeted education and preventive measures are vital. Understanding the infection’s transmission pathways will enable public health officials to construct effective interventions aimed at high-risk groups, ultimately curbing its spread and impact.
Importance of STI Awareness and Education
Raising awareness about sexually transmitted fungal infections is crucial for public health. Many individuals remain unaware that such infections exist and can be transmitted through sexual contact. Education regarding the signs and symptoms of conditions like genital tinea can empower individuals to seek timely medical treatment, potentially reducing the number of cases reported.
Increased awareness campaigns can also highlight the importance of safe sexual practices, such as using protection and avoiding skin contact with infected areas. These strategies are essential components of a broader public health approach aimed at minimizing the prevalence of STIs, including fungal infections, thereby safeguarding the overall health of communities.
Identifying Fungal Infections: Diagnostic Techniques
Accurate diagnosis of sexually transmitted fungal infections like those caused by Trichophyton mentagrophytes requires specific diagnostic techniques. Clinicians rely on a combination of clinical evaluations, laboratory cultures, and DNA sequencing to confirm the presence of the fungus and ensure appropriate treatment. Improved diagnostic tools and rapid testing can significantly enhance the ability to identify infections early.
Furthermore, increasing access to dermatophyte identification and antifungal susceptibility testing is essential in clinical settings. These advancements can lead to better patient outcomes and reduce the public health burden associated with untreated fungal infections. It is vital for healthcare systems to integrate advanced diagnostics into routine STI screenings to facilitate faster and more accurate responses.
Preventing the Spread of Fungal Infections
Preventing the spread of sexually transmitted fungal infections requires a multifaceted approach, emphasizing hygiene practices and safe sexual behaviors. Avoiding skin-to-skin contact with infected areas and maintaining cleanliness are fundamental steps individuals can incorporate into their daily routines to reduce transmission risk.
Additionally, regular screening and open communication about sexual health among partners can help in identifying infections early. Providing education focused on STI prevention, including sexually transmitted fungal infections, will equip individuals with the knowledge they need to safeguard their health and that of their partners.
The Impact of Travel on Fungal Transmission
Traveling to different regions can expose individuals to various pathogens, including sexually transmitted fungal infections. The cases reported in New York highlighted a common link among some patients who had traveled to Europe or engaged in sexual activities with partners whose sexual health backgrounds were unknown. This emphasizes the need for awareness among travelers regarding potential health risks.
Travelers should be educated about the importance of safe practices in sexual health, especially in areas where sexually transmitted infections are more prevalent. Providing resources and guidelines specifically catered to travelers can help minimize the risk of contracting and transmitting infections like TMVII during trips.
Frequently Asked Questions
What are the symptoms of sexually transmitted fungal infections caused by Trichophyton mentagrophytes?
Symptoms of sexually transmitted fungal infections, particularly those caused by Trichophyton mentagrophytes, include rashes on the face, buttocks, or genitals. Patients may experience itching, redness, and discomfort in the affected areas, which are indicative of genital tinea or ringworm.
How is genital tinea treated when caused by sexually transmitted fungal infections?
Genital tinea, particularly when linked to sexually transmitted fungal infections like those from Trichophyton mentagrophytes, is typically treated with antifungal medications. These treatments effectively target the fungal infection and can help alleviate symptoms such as rashes and itching.
How does STI awareness relate to sexually transmitted fungal infections?
STI awareness is crucial for understanding and preventing sexually transmitted fungal infections. The emergence of infections like those caused by Trichophyton mentagrophytes highlights the need for education on safe sex practices and recognizing symptoms of genital tinea.
Can sexually transmitted fungal infections like ringworm occur in men?
Yes, sexually transmitted fungal infections, including ringworm caused by Trichophyton mentagrophytes, can occur in men. Recent cases in New York have primarily affected men who reported sexual contact with other men, emphasizing the importance of awareness and preventive measures.
What measures can healthcare providers take to recognize sexually transmitted fungal infections?
Healthcare providers should be educated on the symptoms of sexually transmitted fungal infections, particularly those caused by Trichophyton mentagrophytes. Enhanced public health surveillance, along with improved access to dermatophyte identification and antifungal susceptibility testing, can aid in early detection and prevention.
Is Trichophyton mentagrophytes common in sexually active individuals?
While Trichophyton mentagrophytes is traditionally associated with dermatophyte infections, the emergence of sexually transmitted cases has raised attention. Awareness of its transmission through sexual contact is essential, particularly among sexually active individuals and at-risk groups.
What steps can be taken to prevent the spread of sexually transmitted fungal infections?
Preventing the spread of sexually transmitted fungal infections such as genital tinea involves practicing safe sex, avoiding contact with infected areas, and seeking medical advice if symptoms arise. Public health initiatives and education are also key to raising awareness about these infections.
| Key Point | Details |
|---|---|
| Emerging Fungal Infection | Recent cases of Trichophyton mentagrophytes type VII (TMVII) reported in New York. |
| Source | Morbidity and Mortality Weekly Report. |
| Patient Demographics | Four men aged 30 to 39 from New York City. |
| Symptoms | Rashes on face, buttocks, or genitals. |
| Transmission | Can be transmitted through sexual contact. |
| Treatment | Successfully treated with antifungal medications. |
| Public Health Recommendations | Awareness and education for healthcare providers and patients. |
Summary
Sexually transmitted fungal infection, particularly those caused by Trichophyton mentagrophytes type VII (TMVII), is emerging as a significant health concern in the U.S., especially indicated by recent reports of cases in New York City. The identification of these infections highlights the need for increased awareness among healthcare providers regarding transmission routes and symptoms. Enhanced public health surveillance, alongside educational initiatives, is crucial to prevent the potential spread of TMVII and ensure prompt treatment for affected individuals.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.