SARS-CoV-2 encephalopathy has emerged as a frightening complication among pediatric patients, showcasing severe neurological symptoms linked to COVID-19. Reports highlight a tragic case series involving 25 children from various Asian and Oceanian countries, grappling with life-threatening encephalopathy as a result of this viral infection. These children experienced alarming conditions characterized by rapid brain edema, ultimately leading to multiorgan failure in a significant number of cases. The association between SARS-CoV-2 and neurological crises in children not only raises concerns about immediate health impacts but also stresses the importance of monitoring long-term neurological outcomes. As healthcare providers increasingly encounter these cases, understanding the nuances of symptoms like brain edema in children is crucial for timely interventions.
The condition known as SARS-CoV-2 encephalopathy reflects a critical manifestation of COVID-19, particularly in younger patients facing severe neurological challenges. Often seen in conjunction with acute multiorgan failure, this neurological crisis raises urgent public health questions as it can lead to life-threatening situations. The ongoing analysis of pediatric patients who develop profound brain swelling and other related symptoms emphasizes the need for heightened awareness in treating affected children. With cases rising in regions across Asia and Oceania, the urgent need to identify and manage neurological symptoms associated with SARS-CoV-2 cannot be overstated. Understanding the full spectrum of this condition is vital to improving outcomes and addressing the complexities surrounding pediatric COVID-19 infections.
Understanding SARS-CoV-2 Encephalopathy in Pediatric Patients
SARS-CoV-2 encephalopathy has emerged as a significant concern in the realm of pediatric health, particularly during the COVID-19 pandemic. This life-threatening neurological condition appears to manifest in children following SARS-CoV-2 infections, leading to severe outcomes, including multiorgan failure. In recent reports from Asia and Oceania, medical professionals have detailed alarming cases where young patients developed acute encephalopathy characterized by rapid brain edema. This underscores the need for heightened awareness and monitoring of neurological symptoms in children suspected of COVID-19 infections.
The neurological symptoms associated with SARS-CoV-2 encephalopathy can be particularly severe, ranging from confusion and altered consciousness to respiratory distress and shock. In fact, many children presented with shock and multiorgan failure shortly after the onset of their neurological symptoms, raising concerns about the immediate and long-term effects of this condition. With 88% of reported cases resulting in death, it’s clear that SARS-CoV-2 encephalopathy represents a formidable challenge for clinicians and families alike.
The Impact of COVID-19 on Children’s Neurological Health
As the COVID-19 pandemic continues to evolve, children’s health has been impacted in numerous ways, with neurological complications being among the most concerning. Reports of children experiencing life-threatening neurological symptoms, such as encephalopathy and brain edema, have become increasingly common. These complications may stem from the body’s hyperinflammatory response—a phenomenon sometimes referred to as a COVID-19 neurological crisis, where excessive cytokine release leads to significant brain injury and multiorgan failure.
The observation of elevated levels of cytokines and chemokines, like interleukin 6 and tumor necrosis factor-α, has been crucial in understanding the pathophysiology of these neurological manifestations. Understanding the intricate relationship between viral infection and neurological symptoms, alongside comprehensive management strategies, is paramount. It’s essential for healthcare providers to remain vigilant for signs of neurological distress in pediatric patients with COVID-19, facilitating earlier interventions that may mitigate severe outcomes.
Recognizing Early Signs of Neurological Crisis in Children
Timely recognition of neurological symptoms in children with COVID-19 is critical in preventing the progression to severe conditions, such as SARS-CoV-2 encephalopathy and associated multiorgan failure. Symptoms like sudden confusion, seizures, or significant changes in behavior should alert healthcare providers to the potential for neurological involvement. Studies indicate that nearly half of children with SARS-CoV-2 encephalopathy can experience life-threatening decompensation within just a few hours, emphasizing the importance of rapid assessment and intervention.
Healthcare systems must implement screening protocols for neurological symptoms in pediatric COVID-19 patients, particularly given the rapid onset of complications such as brain edema. Health professionals should be trained to recognize these early warning signs, as they can significantly influence the prognosis and mortality risk. Additionally, raising awareness among parents and caregivers about potential neurological symptoms is vital, as it could lead to quicker medical attention and potentially save lives.
The Role of Multiorgan Failure in SARS-CoV-2 Encephalopathy
Multiorgan failure is often seen in conjunction with SARS-CoV-2 encephalopathy, complicating the clinical presentation and management of affected pediatrics. This failure arises when the body’s organs begin to shut down due to the extreme inflammatory response elicited by SARS-CoV-2. For pediatric patients, the combination of brain edema and multiorgan dysfunction can lead to rapid clinical deterioration, often seen during critical illnesses linked to COVID-19.
The mechanism behind this interplay is thought to involve direct viral effects on organ systems, as well as indirect consequences of systemic inflammation. Evidence suggests that over 70% of children with neurological symptoms may experience multiorgan failure within hours of onset, indicating a need for integrated treatment approaches addressing both neurological care and support for failing organ systems. Collaborative efforts among neurologists, intensivists, and infectious disease specialists are essential to improving outcomes for these vulnerable patients.
Long-Term Consequences of SARS-CoV-2 on Children’s Neurology
The long-term neurological consequences of SARS-CoV-2 infections in children remain an area of ongoing research. While immediate complications such as encephalopathy and brain edema are well-documented, the potential for lasting effects, such as cognitive impairment or increased susceptibility to neurological disorders, raises significant concerns among health professionals and families alike. The extent of these repercussions can involve chronic fatigue, mood disorders, and learning difficulties, which may emerge even after the acute phase of illness.
As we strive to understand the full impact of SARS-CoV-2 on pediatric neurological health, it becomes crucial to establish clear follow-up protocols for children who have experienced severe COVID-19 symptoms. Regular neurological assessments and mental health screenings should be integrated into routine healthcare for these patients, to ensure early identification and management of any emerging issues. A proactive approach may ultimately improve the quality of life for children recovering from COVID-19 and lessen the burden of potential long-term neurological effects.
Cytokine Storm and its Role in Neurological Damage
The phenomenon known as the ‘cytokine storm’ plays a pivotal role in the pathogenesis of SARS-CoV-2 encephalopathy, especially in pediatric patients. This hyper-inflammatory response leads to an overwhelming release of pro-inflammatory cytokines that can damage brain tissue and disrupt normal neural functions. Elevated levels of cytokines, including interleukin 6 and TNF-α, have been associated with more severe cases of encephalopathy and can significantly contribute to conditions such as brain edema and multiorgan failure.
Understanding the mechanism by which cytokines contribute to neurological damage could help inform treatment strategies aimed at mitigating these effects. Interventions targeting inflammatory pathways may offer promising avenues for reducing the severity of encephalopathy and associated symptoms in children affected by COVID-19. Ongoing research will be critical in elucidating how best to manage the delicate balance between fighting viral infection and preventing the devastating consequences of excessive inflammation.
Clinical Management Strategies for SARS-CoV-2 Encephalopathy
Managing SARS-CoV-2 encephalopathy in children necessitates a multidisciplinary approach that focuses on immediate stabilization and supportive care. Healthcare providers must be equipped to assess and monitor neurological status promptly, ensuring that any signs of deterioration are addressed without delay. Therapeutic interventions may include the use of anti-inflammatory medications, intravenous fluids, and, in certain severe cases, mechanical ventilation to support compromised functions.
In addition to clinical management, a robust framework for longitudinal care is essential to address the needs of children recovering from SARS-CoV-2 encephalopathy. Rehabilitation services, including speech, occupational, and physical therapy, can play a significant role in helping these children regain their cognitive and motor skills. Community support systems should also be implemented to provide families with resources, encompassing both physical health and mental health support, to navigate the challenges posed by these severe cases.
Implications for Future Research on Pediatric COVID-19 Outcomes
The emergence of severe neurological complications in children due to SARS-CoV-2 necessitates a focused research agenda to better understand and mitigate these effects. Insights gained from recent cases of SARS-CoV-2 encephalopathy could inform public health strategies, vaccination campaigns, and clinical guidelines tailored to protect pediatric populations. Collaborative studies focusing on immune responses, neurobiological factors, and long-term outcomes will be pivotal in shaping future approaches to managing COVID-19 in young patients.
Moreover, understanding the variations in outcomes among different geographical regions, as illustrated by reports from Asia and Oceania, can highlight critical factors influencing severe disease in children. Future investigations should also prioritize the establishment of robust datasets that track neurological symptoms and their impacts over time, thereby contributing to a comprehensive view of COVID-19 in pediatric populations and helping to guide effective interventions.
Frequently Asked Questions
What is SARS-CoV-2 encephalopathy in children?
SARS-CoV-2 encephalopathy is a severe neurological condition occurring in children infected with the SARS-CoV-2 virus. It manifests as life-threatening encephalopathy marked by rapidly progressive cerebral edema and is often linked to multiorgan failure.
What neurological symptoms are associated with SARS-CoV-2 encephalopathy in children?
Children with SARS-CoV-2 encephalopathy can present with neurological symptoms such as confusion, seizures, reduced consciousness, and signs of increased intracranial pressure due to brain edema.
How does COVID-19 cause multiorgan failure associated with encephalopathy in children?
COVID-19 can lead to multiorgan failure in children due to severe inflammatory responses triggered by SARS-CoV-2, often resulting in encephalopathy and subsequent organ dysfunction due to hypoperfusion and edema.
What are the signs of brain edema in children with SARS-CoV-2 encephalopathy?
Signs of brain edema in children with SARS-CoV-2 encephalopathy may include sudden onset of severe headache, vomiting, altered mental status, and neurological deficits due to increased intracranial pressure.
Why is SARS-CoV-2 encephalopathy considered a neurological crisis?
SARS-CoV-2 encephalopathy is considered a neurological crisis due to its rapid progression and high mortality rate, with affected children frequently developing acute shock and multiorgan failure shortly after the onset of neurological symptoms.
What is the mortality rate for children with SARS-CoV-2 associated encephalopathy?
The mortality rate for children affected by SARS-CoV-2 associated encephalopathy is alarmingly high, with studies showing that up to 88% of affected children may die, often within 24 hours of hospitalization.
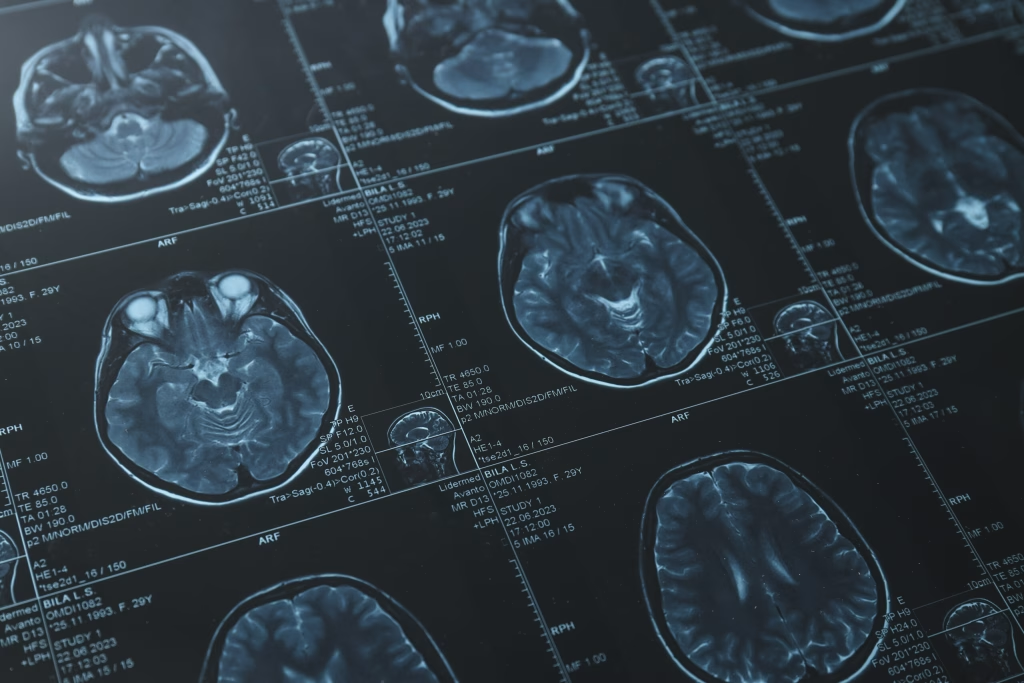
How is SARS-CoV-2 encephalopathy diagnosed in children?
Diagnosis of SARS-CoV-2 encephalopathy in children relies on clinical evaluation of neurological symptoms, imaging studies to assess brain edema, and laboratory tests to identify viral infection and inflammatory markers.
What treatment options are available for children with SARS-CoV-2 encephalopathy?
Treatment for children with SARS-CoV-2 encephalopathy focuses on supportive care, managing increased intracranial pressure, and addressing any associated multiorgan failure, as there is currently no specific antiviral treatment for this condition.
How prevalent is SARS-CoV-2 encephalopathy in Asia and Oceania from 2022 to 2024?
Reports from Asia and Oceania indicate that SARS-CoV-2 encephalopathy is an emerging public health issue, with numerous cases identified among children during the 2022 to 2024 period, notably characterized by severe outcomes and multiorgan involvement.
What cytokines are elevated in cases of SARS-CoV-2 encephalopathy?
In cases of SARS-CoV-2 encephalopathy, cytokines such as interleukin-6 and tumor necrosis factor-alpha are significantly elevated, indicating a hyper-inflammatory response associated with the progression of neurological symptoms.
| Key Point | Details |
|---|---|
| Overview | The study documents severe cases of SARS-CoV-2–associated encephalopathy in children across Asia and Oceania during 2022–2024. |
| Patient Demographics | A total of 25 children from Australia, Japan, Singapore, and Taiwan were involved in the case series. |
| Mortality Rate | 88% of the children died, with 44% dying within the first 24 hours of hospitalization. |
| Symptoms | The children presented with rapidly progressive cerebral edema, shock, and multiorgan failure within hours of symptoms onset. |
| Inflammatory Markers | Elevated serum concentrations of interleukin 6 and tumor necrosis factor-α were observed within 24 hours of onset compared to controls. |
| Critical Insights | The data underscores SARS-CoV-2 encephalopathy as a major neurological crisis in children with high morbidity and mortality rates. |
Summary
SARS-CoV-2 encephalopathy has emerged as a life-threatening condition affecting children in Asia and Oceania. This neurological crisis is characterized by severe symptoms including rapidly progressive cerebral edema and multiorgan failure, leading to a staggering mortality rate. As evidenced by the case series from 2022 to 2024, the ability to identify and manage the associated inflammation promptly is crucial for improving outcomes in affected children.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.