RSV prevention interventions are crucial in safeguarding newborns from respiratory syncytial virus (RSV) infections, especially during the peak virus season. Recent studies highlight the cost-effectiveness of these interventions, namely maternal vaccination and the administration of nirsevimab, a long-acting monoclonal antibody. Research from the University of Utah suggests that the timing of these preventive measures can significantly influence their efficacy and overall cost-effectiveness. With RSV vaccination recommendations emphasizing the importance of administering the maternal vaccine at specific gestational ages, the potential impact on reducing hospitalizations and outpatient visits is remarkable. By optimizing these strategies, we can not only enhance nirsevimab efficacy but also contribute to better health outcomes for vulnerable infants.
As the fight against respiratory syncytial virus (RSV) intensifies, innovative strategies for newborn RSV prevention have emerged, focusing on interventions that protect our youngest and most susceptible populations. The evaluation of cost-effective measures, including maternal immunization and the use of nirsevimab, shows promising results in safeguarding health during peak RSV seasons. These interventions provide critical protection against severe illness, reducing the burden on healthcare systems. By understanding the nuances of each preventive method, healthcare professionals can make informed RSV vaccination recommendations tailored to the needs of mothers and their infants. Continued research is essential to refine these methods and ensure optimal outcomes in RSV prevention.
Understanding RSV Prevention Interventions
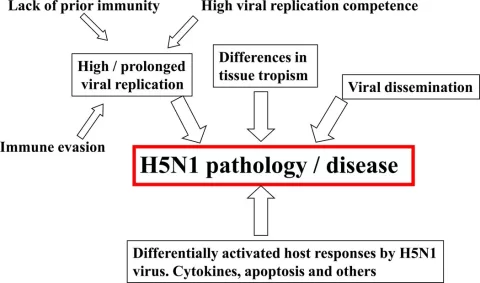
Respiratory syncytial virus (RSV) is a significant cause of hospitalization among infants, making the need for prevention interventions critical. Current strategies include maternal vaccination and the administration of nirsevimab, a long-acting monoclonal antibody. Both interventions aim to provide early protection to newborns against RSV, ensuring that these vulnerable populations have a lower risk of severe infections. The timing of these interventions heavily influences their effectiveness and cost-effectiveness, which is essential for healthcare policies.
Recent studies underscore that administering the maternal vaccine between the gestational ages of 32 and 36 weeks optimizes the immune response for newborns. This window is crucial because it aligns with the RSV season, thereby enhancing the likelihood of generating adequate maternal antibodies that can protect infants after birth. In comparison, nirsevimab offers immediate passive immunity to infants at risk of RSV, creating a dual strategy in combating this virus, depending on the specific circumstances surrounding each birth.
Examining Cost-Effectiveness of RSV Prevention Strategies
Cost-effectiveness analyses of RSV prevention interventions indicate significant differences in their economic impacts and health outcomes. For instance, while maternal vaccination demonstrated a cost-effectiveness of $19,562 per quality-adjusted life-year (QALY), nirsevimab was variably effective based on the month administered, costing $67,178/QALY in October and rising to $88,531/QALY in November. Such information not only guides healthcare professionals in making informed decisions about RSV prevention but also aids policymakers in allocating resources efficiently.
Furthermore, the analysis from the University of Utah highlights the efficacy and cost-effectiveness of each intervention in the context of real-life hospitalizations and outpatient visits. Maternal vaccination was projected to avert a substantial number of outpatient visits and hospital admissions compared to nirsevimab. This underscores the importance of considering both the economic and health-related outcomes when evaluating RSV prevention strategies, ultimately aiming for the most beneficial intervention within set budget constraints.
Impact of Maternal Vaccination for RSV
Maternal vaccination is emerging as a pivotal intervention in the fight against RSV, particularly through its ability to generate passive immunity for infants. The Advisory Committee on Immunization Practices recommends the seasonal administration of the maternal vaccine to enhance the protective antibody response during critical months of RSV transmission. Given that RSV poses a significant risk to infants in their first year of life, timely vaccination during pregnancy can drastically reduce their likelihood of severe disease.
The study findings further suggest that when maternal vaccination is administered correctly, it can lead to impressive outcome statistics, including the prevention of thousands of outpatient visits and hospitalizations. Considering the projected outcomes, maternal vaccination not only acts to protect individual infants but also contributes to the overall public health strategy aimed at reducing the burden of RSV on healthcare systems. As understanding of maternal vaccination expands, it may become increasingly integrated into standard prenatal care routines.
Evaluating Nirsevimab Efficacy and Timing
Nirsevimab has shown significant promise in providing immediate, passive immunity to infants against RSV. Its high efficacy rates—recorded at 76.8% for preventing RSV hospitalization and 78.0% for outpatient infections—position it as a critical tool for clinical practice, especially for infants deemed at high risk of severe RSV. However, the effectiveness of nirsevimab is notably influenced by the timing of administration, highlighting the need for clear guidelines regarding its use.
Researchers have identified that nirsevimab is particularly cost-effective when administered in October, just prior to the peak RSV season, thereby emphasizing the importance of timing. The delineation of optimal months for nirsevimab administration is essential to maximize resource allocation and health outcomes. With ongoing studies exploring RSV transmission dynamics, future recommendations may evolve to further refine and enhance the cost-effectiveness and clinical impact of nirsevimab.
RSV Vaccination Recommendations and Guidelines
Vaccination recommendations for RSV are crucial to ensuring the health of infants during their vulnerable first year of life. The Centers for Disease Control and Prevention (CDC) emphasizes that both maternal vaccination and nirsevimab should be considered to provide the best protection against RSV infections. These guidelines inform healthcare providers about the most effective strategies to mitigate RSV risks, promoting proactive rather than reactive healthcare practices.
The recommendations provided by health authorities help streamline the decision-making process for parents and healthcare providers alike. By complying with vaccination protocols, newborns can achieve a level of immunity that significantly lowers their risk of severe respiratory illnesses associated with RSV. As new data emerges and strategies evolve, staying updated with the latest guidelines is essential for maximizing the effectiveness of RSV prevention efforts.
Newborn RSV Prevention Strategies
Preventing RSV in newborns involves a multifaceted approach, combining maternal vaccination and the administration of monoclonal antibodies like nirsevimab. These strategies are designed to create immunity both before and after birth, protecting infants during the critical months following delivery. Health professionals recommend that expectant mothers get vaccinated during their later trimesters, coinciding with RSV transmission peaks.
Healthcare systems focused on newborn RSV prevention can significantly reduce the incidence of severe cases and hospitalizations. Ensuring that parents are educated about these prevention strategies and the critical timeframes for administration can lead to better health outcomes for infants. Implementing these interventions effectively requires collaboration between maternal healthcare providers and pediatricians.
Future Directions in RSV Prevention Research
As RSV prevention strategies evolve, ongoing research will be critical in optimizing interventions. Currently, data on maternal vaccination and nirsevimab efficacy are guiding best practices, but understanding the dynamics of RSV transmission within various populations will be essential for further refinement. Future studies are expected to focus on better identifying cost-effective timing for both maternal vaccination and individualized administration of nirsevimab.
Additionally, the implications of these interventions on healthcare resources and public health outcomes warrant continuous exploration. As more is learned about the long-term effectiveness and economic viability of RSV prevention strategies, health experts can develop enhanced recommendations to minimize the viral burden on society.
The Role of Public Health in RSV Prevention
Public health plays an instrumental role in the promotion and implementation of RSV prevention strategies. Strong messaging around the importance of maternal vaccination during pregnancy and timely administration of monoclonal antibodies can significantly influence community uptake. Public health campaigns aimed at educating expectant mothers about the risks of RSV can foster a proactive approach to preventing respiratory infections in newborns.
Moreover, health policymakers must prioritize funding for these interventions to ensure accessibility for all populations. By integrating RSV prevention into broader public health initiatives, communities can better prepare to combat seasonal outbreaks, reduce healthcare costs, and ultimately protect the most vulnerable members of society—our newborns.
Assessing the Long-term Impact of RSV Interventions
The long-term impact of interventions like maternal vaccination and nirsevimab on the landscape of RSV infections is still being studied. Observations from ongoing research will be vital in determining whether these prevention strategies decrease the incidence of RSV in the population over time. As healthcare providers implement these recommendations, continued surveillance of infection rates and health outcomes will inform future adjustments to these strategies.
Furthermore, by analyzing data accumulated from the implementation of these interventions, healthcare experts can assess whether the investment in RSV prevention translates into a measurable decrease in hospitalizations and healthcare costs associated with RSV. The longitudinal data will be critical in advocating for sustained support of these life-saving interventions across healthcare systems.
Frequently Asked Questions
What are the cost-effectiveness factors of RSV prevention interventions for newborns?
The cost-effectiveness of RSV prevention interventions, such as maternal vaccination and nirsevimab administration, can significantly depend on the timing of administration. For instance, maternal vaccination was found to be highly cost-effective at $19,562 per quality-adjusted life-year (QALY) in certain months, while nirsevimab was only cost-effective during October at $67,178/QALY and November at $88,531/QALY. This timing is crucial to optimize resource use and achieve better health outcomes.
How does maternal vaccination impact RSV prevention in infants?
Maternal vaccination plays a vital role in RSV prevention for infants by providing passive immunity during critical first months of life. The vaccine can be administered between 32-36 weeks of gestation, and research indicates it has an initial effectiveness of 67.9% for preventing RSV hospitalization and 48.2% for outpatient infections. This intervention not only reduces the risk of severe RSV outcomes but is also cost-effective, potentially averting thousands of hospitalizations during the RSV season.
What is nirsevimab and how effective is it for RSV prevention in infants?
Nirsevimab is a long-acting monoclonal antibody designed for RSV prevention in infants. It has shown an impressive initial effectiveness rate of 76.8% for RSV hospitalization and 78.0% for outpatient infections. Given its efficacy, nirsevimab is a valuable option for infants, especially if maternal vaccination is not administered during pregnancy.
What are the current RSV vaccination recommendations for pregnant women?
The Advisory Committee on Immunization Practices and the Centers for Disease Control and Prevention strongly recommends that pregnant women receive the seasonal maternal vaccination between 32 to 36 weeks of gestation during the RSV season, typically from September to January. This recommendation is aimed at minimizing risks to newborns from severe RSV infections.
How does the timing of RSV prevention interventions affect their cost-effectiveness?
Timing is a critical factor affecting the cost-effectiveness of RSV prevention interventions. For example, maternal vaccination is most cost-effective when administered in specific months, while nirsevimab demonstrates varying cost-effectiveness depending on the month of administration. By optimizing the timing of these interventions, the healthcare system can achieve better health outcomes and manage costs more effectively.
What is the projected impact of maternal vaccination and nirsevimab on RSV-related hospitalizations?
Projected data indicate that maternal vaccination could avert approximately 45,558 outpatient visits and 7,154 hospital admissions during the RSV season. In contrast, nirsevimab could prevent around 92,265 outpatient visits and 11,893 hospitalizations. These interventions drastically reduce the burden of RSV on infants and the healthcare system.
What are the differences in efficacy between maternal vaccination and nirsevimab for RSV prevention?
Maternal vaccination and nirsevimab differ in terms of their efficacy rates for preventing RSV. Maternal vaccination has an effectiveness of 67.9% for hospitalization and 48.2% for outpatient infections, while nirsevimab significantly outperforms with 76.8% and 78.0% effectiveness, respectively. This makes nirsevimab a strong option, especially when maternal vaccination is not utilized.
Are there any specific months recommended for administering RSV prevention interventions?
Yes, it is recommended that maternal vaccination be administered between 32 to 36 weeks of gestation during the RSV season, ideally from September to January. For nirsevimab, research indicates that its cost-effectiveness is optimal when given in October and November, indicating the importance of targeting vaccination timing to enhance RSV prevention outcomes.
| Intervention Type | Initial Effectiveness | Cost-Effectiveness (QALY) | Outcomes Averted | Optimal Timing |
|---|---|---|---|---|
| Maternal Vaccination | 67.9% (RSV hospitalization), 48.2% (outpatient infection) | $19,562 | 45,558 outpatient visits, 7,154 hospitalizations, 12 deaths | Administered at 32-36 weeks gestation (Sept-Jan) |
| Nirsevimab (Beyfortus) | 76.8% (RSV hospitalization), 78.0% (outpatient infection) | $67,178 (October), $88,531 (November) | 92,265 outpatient visits, 11,893 hospitalizations, 19 deaths | Administered if maternal vaccination not given |
| No Intervention | N/A | 19.8% odds | N/A | N/A |
Summary
RSV prevention interventions are crucial for protecting infants from severe RSV infections, particularly during their critical first year of life. Maternal vaccination shows a high cost-effectiveness, especially when administered during specific gestational weeks. Nirsevimab, while initially more effective in outpatient settings, requires careful timing to be cost-effective. A strategic approach to the administration timing of these interventions can significantly optimize health outcomes for newborns in the face of RSV, as indicated by the research findings.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.