Rotavirus vaccine effectiveness is a critical area of study, particularly highlighted by a recent CDC report stating that the vaccine is 78% effective in preventing serious illness among preschoolers. The findings underscore the importance of this vaccination in reducing pediatric hospitalization rates associated with gastrointestinal infections. With a substantial impact on childhood gastroenteritis prevention, the vaccination has led to a significant decline in severe rotavirus diseases since its introduction. Notably, the study also emphasizes the vital role of ongoing monitoring to ensure the continued confidence in rotavirus vaccination benefits. As parents and caregivers become informed about the importance of this vaccine, they can better protect their children against gastroenteritis and its complications.
The effectiveness of the rotavirus immunization is essential in combating severe diarrheal diseases in infants and young children. This vaccine has revolutionized the approach to managing gastrointestinal illnesses, helping to drastically lower hospital admissions related to pediatric gastroenteritis. By examining the efficacy of rotavirus vaccinations, we gain insights into preventing acute inflammation of the gastrointestinal tract, which is a leading cause of hospitalization in the pediatric population. These findings highlight the significance of vaccination in reducing the burden of severe gastrointestinal infections, ultimately enhancing child health outcomes. As research continues to unfold, the ongoing benefits of rotavirus vaccination will be crucial in safeguarding children from preventable illnesses.
Understanding Rotavirus Vaccine Effectiveness
The effectiveness of the rotavirus vaccine, pivotal in protecting children from severe gastroenteritis, has shown promising results, particularly in preschool-aged children. According to the findings from the CDC’s study, a single dose of the vaccine is 78% effective in preventing emergency department visits and hospitalizations related to rotavirus in children under five. The implications of this finding underscore the critical role the vaccine plays in childhood health, significantly reducing the incidence of severe gastrointestinal illnesses that can lead to dehydration and serious complications.
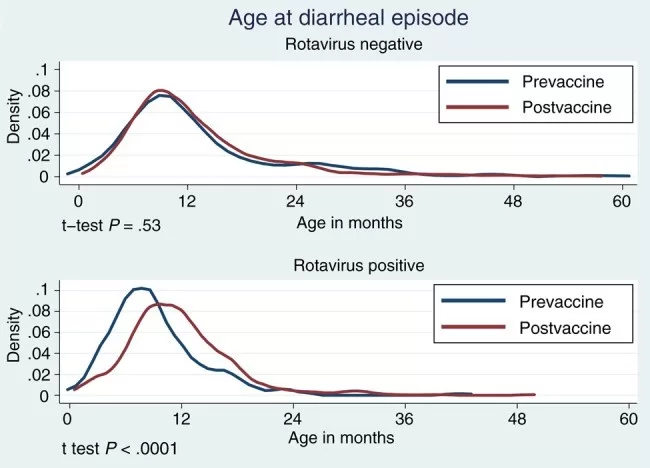
In contrast, the vaccine’s effectiveness diminishes as children age, registering at only 53% effectiveness for those older than five years. This trend highlights the necessity for continuous monitoring and evaluation of vaccine efficacy across different age groups. With rotavirus once being the leading cause of acute gastroenteritis in the United States, the decline in hospitalization rates since the vaccine’s introduction in 2006 is a testament to the vaccine’s success and its importance in pediatric healthcare.
The Impact of Rotavirus on Childhood Gastroenteritis
Rotavirus remains a significant contributor to gastroenteritis in children, leading to approximately 200,000 hospitalizations annually in the United States. Gastroenteritis, characterized by diarrheal episodes and vomiting, can be particularly severe in younger children, making effective prevention essential. The CDC’s study sheds light on the prevalence of rotavirus and the associated pediatric hospitalization rates, reflecting a clear need for vaccination as a primary strategy for reducing morbidity associated with this viral infection.
Ensuring children receive the rotavirus vaccine on schedule is critical for preventing outbreaks of gastroenteritis. Vaccination campaigns targeting parents and caregivers can further enhance awareness regarding the importance of rotavirus immunization. The benefits of rotavirus vaccination extend beyond individual protection; they also contribute to community health by decreasing overall disease transmission, enabling children to remain healthier and reducing the strain on healthcare resources.
Long-term Benefits of Rotavirus Vaccination
The long-term benefits of the rotavirus vaccination program are evident as researchers continue to observe significant declines in severe rotavirus disease. With the CDC’s research highlighting a 78% effectiveness rate against severe illness among children under five, it is clear that the vaccine plays a crucial role in maintaining child health and preventing gastrointestinal hospitalizations. Furthermore, continuous vaccination and monitoring strategies are essential to ensure that these gains are upheld over time.
In addition to minimizing the immediate risks of serious illness, rotavirus vaccination yields broader health benefits, including reduced healthcare costs and improved quality of life for children and families. By preventing serious gastroenteritis cases, the rotavirus vaccine helps families avoid the emotional and financial burdens associated with hospital emergencies and treatments. This holistic approach to child wellness underscores the importance of maintaining high vaccination coverage to continue reaping the benefits of rotavirus immunization.
CDC’s Findings on Pediatric Hospitalizations
The data utilized in the CDC study stems from an extensive evaluation of pediatric hospitalizations, specifically focusing on children presenting with symptoms of gastroenteritis. By involving eight pediatric hospitals, the research captures a comprehensive picture of rotavirus impacts on emergency health services. With findings indicating that vaccinated children are significantly less likely to be admitted for rotavirus-related illnesses, these results reinforce the importance of proactive vaccination initiatives in reducing pediatric hospitalization rates.
Moreover, the study highlights the importance of public health strategies in addressing gastroenteritis in children. The vaccination not only decreases the direct health burdens but also mitigates the strain on healthcare systems during peak rotavirus seasons. By translating vaccine effectiveness data into actionable public health policies, communities can better protect their younger populations from gastroenteritis-related health issues, ensuring fewer children experience preventable hospital visits.
Rotavirus Vaccination and Emergency Department Visits
The CDC’s analysis also emphasizes the reduction of emergency department visits among vaccinated children, with rotavirus vaccination demonstrating a protective effect against gastroenteritis symptoms severe enough to require hospital treatment. This aspect is particularly relevant for parents concerned about the frequent hospital visits that can be disruptive and arduous. Seeing that vaccinated children are likely to have fewer emergency room visits, offers reassurance and motivation for families to adhere to pediatric vaccination schedules.
Incorporating education about the rotavirus vaccine into routine pediatric care can further enhance its uptake. Healthcare providers can play a pivotal role by discussing the symptoms of rotavirus and emphasizing the preventative nature of the vaccine against these symptoms. This proactive approach is necessary for minimizing emergency visits related to gastroenteritis, ensuring that children can navigate their developmental stages without the interruptions that frequent illnesses can cause.
The Role of CDC in Monitoring Vaccine Effectiveness
The CDC’s role in tracking rotavirus vaccine effectiveness is paramount in informing public health policies and adjusting vaccination strategies as needed. By analyzing data over several years, the CDC has been able to detect trends in rotavirus incidence and vaccine responsiveness. This ongoing surveillance ensures that any decline in vaccine effectiveness is quickly addressed, maintaining public confidence in vaccination programs.
Moreover, the CDC’s emphasis on collaborative approaches in its studies serves as a model for future research initiatives. Continued support and investment in vaccine studies, such as the one involving the New Vaccine Surveillance Network, are essential for ensuring that the benefits of immunization against rotavirus are sustained and optimized. As the landscape of pediatric health evolves, the CDC’s vigilance will be vital in safeguarding children’s health outcomes and minimizing the incidence of gastroenteritis.
Public Confidence in Rotavirus Vaccination Programs
Maintaining public confidence in rotavirus vaccination programs is crucial, especially as parents weigh the benefits and risks associated with childhood vaccines. Trust in health authorities, like the CDC, can significantly influence parents’ decisions to vaccinate their children. The findings from the recent study provide scientific credibility to the effectiveness of the rotavirus vaccine, reinforcing that it substantially reduces serous illnesses among children.
Efforts to engage with the community, disbursing clear and accurate information about vaccine effectiveness and safety can help sustain public trust. Educational initiatives, community forums, and partnerships with healthcare professionals can effectively communicate the importance of vaccination in preventing severe gastroenteritis, thereby encouraging higher vaccination rates and contributing to herd immunity.
Future Trends in Rotavirus Vaccination
As research into rotavirus continues, future trends in vaccination may include improving vaccine formulations and addressing changing epidemiological patterns. The CDC’s findings indicate a need for ongoing surveillance to prepare for shifts in rotavirus strains and their corresponding vaccine effectiveness. Health systems must remain agile and responsive, analyzing data to ensure that immunization strategies adapt over time to protect children effectively.
Additionally, advancing public health messaging on the importance of timely vaccinations can help increase overall participation rates in vaccination programs. Parents’ awareness of the necessity for rotavirus vaccination as a preventive measure against severe gastroenteritis will be pivotal to maintaining the observed downward trends in hospitalizations and related health complications.
Encouraging Rotavirus Vaccination in Communities
Grassroots efforts to promote the rotavirus vaccine at the community level can significantly contribute to overall public health. Local health departments and pediatricians can collaborate to organize informational sessions that guide parents through the benefits of the rotavirus vaccination. By leveraging community trust, these initiatives may effectively combat hesitancy and enhance awareness surrounding childhood gastroenteritis prevention.
Moreover, addressing misconceptions about vaccine side effects and efficacy through transparent and health literacy-focused communication can further boost vaccination rates. Strategies that engage families directly, such as mobile vaccination clinics and community vaccination drives, will play an important role in promoting rotavirus vaccination as an essential component of a child’s health and wellness.
Frequently Asked Questions
What is the effectiveness of the rotavirus vaccine as reported by the CDC?
The CDC reported that the rotavirus vaccine is 78% effective in preventing serious illness from rotavirus in children under 5 years old and 53% effective in older children. This study highlights the vaccine’s role in reducing pediatric hospitalization rates due to rotavirus-related gastroenteritis.
How does the rotavirus vaccine aid in childhood gastroenteritis prevention?
The rotavirus vaccine significantly aids in childhood gastroenteritis prevention by reducing the incidence of severe rotavirus infections, which previously led to high hospitalization rates among children. With effective rotavirus vaccination, families can experience lowered risks of gastroenteritis in children.
What are the benefits of rotavirus vaccination in preventing gastroenteritis in children?
The benefits of rotavirus vaccination include a substantial reduction in emergency department visits and hospitalizations due to severe gastrointestinal diseases such as rotavirus. Studies show that vaccinated children have lower rates of rotavirus-related gastroenteritis, improving overall child health outcomes.
How does the effectiveness of the rotavirus vaccine change with age?
The effectiveness of the rotavirus vaccine tends to be highest in children under 3 years old, where it is reported to be between 73% and 88%. Effectiveness declines with age, particularly beyond 3 years, emphasizing the importance of early vaccination to prevent severe gastroenteritis.
What does the CDC study say about the long-term effectiveness of the rotavirus vaccine?
The CDC study emphasizes the importance of monitoring the long-term effectiveness of rotavirus vaccines, especially against severe illness. The findings indicate that rotavirus vaccines continue to be effective over time, significantly reducing hospitalizations linked to gastroenteritis in children.
What were the main findings regarding rotavirus vaccination benefits in the recent CDC study?
The recent CDC study found that the rotavirus vaccine offers significant protection against severe gastroenteritis, achieving a 78% effectiveness rate against emergency visits and hospitalizations in children under 5 years. This underscores the critical role the vaccine plays in pediatric healthcare.
| Key Points |
|---|
| Study by CDC from 2009 to 2022 showing effectiveness of the rotavirus vaccine |
| Vaccine is 78% effective in preventing serious illness in children under 5 years |
| Vaccine is 53% effective in preventing serious illness in older children (5-17 years) |
| Participants included 1,720 children under 5 and 14,468 controls |
| VE declines after 3 years and is highest in children under 3 years (73%-88%) |
| Monitoring long-term effectiveness is crucial for public confidence in the vaccination program |
Summary
The effectiveness of the rotavirus vaccine, as reported by the CDC, is an impressive 78% against serious illnesses in preschoolers and 53% in older children. This highlights the vaccine’s vital role in preventing rotavirus-related hospitalizations and emergency department visits. With the data spanning a significant period from 2009 to 2022, we see clear indications of the vaccine’s impact, particularly in younger children. Ongoing assessment of its effectiveness is essential to maintain public trust and to continue combating rotavirus, which has significantly declined since the vaccination program’s inception.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.