Processed meat colorectal cancer is a growing health concern, particularly as increasing evidence links dietary choices to disease risk. These meats, which are often preserved through methods like curing and smoking, have been classified as carcinogenic by global health authorities, marking them as significant contributors to colorectal cancer risk factors. With the rise in colorectal cancer diagnoses among younger adults, understanding the health impact of processed meat becomes even more crucial. Implementing a cancer prevention diet that minimizes the intake of processed and red meats can play a vital role in reducing this risk. As individuals seek to navigate their dietary habits amidst the confusion surrounding carcinogenic foods, it is essential to be informed about the implications of consuming processed meats and make mindful choices to protect long-term health.
The risk of developing colorectal cancer has increasingly been associated with the consumption of meat that has undergone various preservation techniques, often referred to as deli or cured meats. Known as harmful dietary components, these processed varieties may contribute significantly to the overall incidence of this type of cancer, particularly in populations with higher meat consumption. In light of recent research, it is clear that a proactive approach to dietary habits can help mitigate cancer risk. Emphasizing the avoidance of both processed and red meat is crucial in the conversation about health and nutrition, as they both stand out amongst recognized cancer risk factors. Engaging in discussions about safe eating practices can guide individuals towards healthier, cancer-preventive diets.
The Link Between Processed Meat and Colorectal Cancer
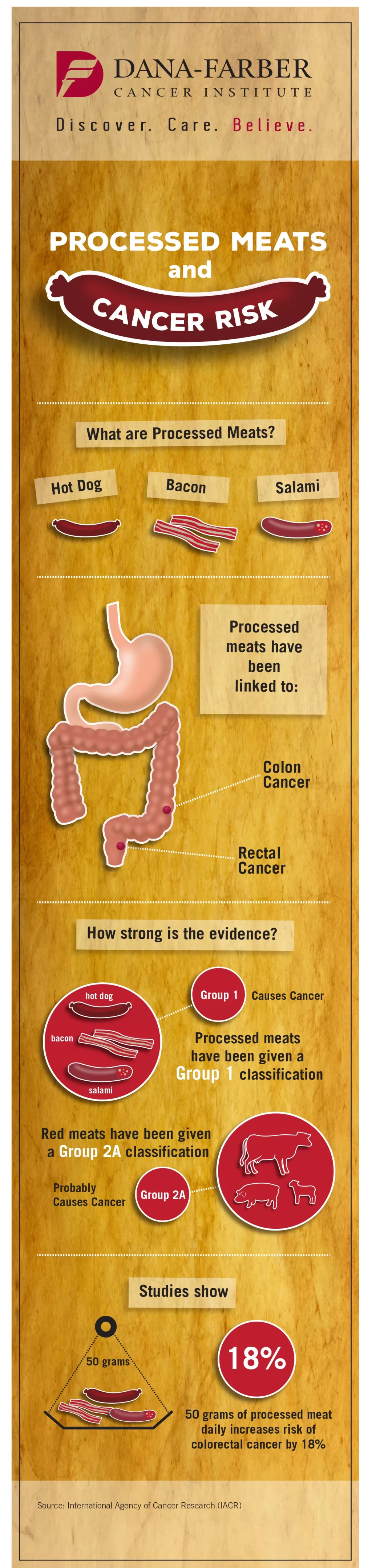
Processed meat has been consistently correlated with an increased risk of colorectal cancer (CRC), as highlighted by numerous studies over the years. The classification of processed meats as carcinogenic to humans by the International Agency for Research on Cancer (IARC) stems from extensive data that demonstrates this link. Dietary habits contribute significantly to CRC risk, and while many factors are involved, processed meat stands out as particularly impactful. Epidemiological studies reveal that individuals with high consumption of processed meats face greater odds of developing CRC, emphasizing the necessity for public awareness regarding this dietary risk.
Within the framework of cancer prevention diets, the reduction of processed meats, particularly those rich in nitrates and nitrites, is vital. These compounds not only enhance flavors but also contribute to the formation of harmful chemicals during digestion. The detrimental effects of such carcinogenic foods illuminate the significance of informed nutritional choices. Health organizations advocate for stringent limits on the intake of processed meats, recommending minimal consumption, if any, to mitigate the risk of CRC and promote overall health.
Understanding Risk Factors for Colorectal Cancer
Various colorectal cancer risk factors have emerged from research, with processed meat being a focal point of ongoing studies. Traditional known risk factors like age, obesity, and family history intersect with dietary influences, creating a complex landscape in predicting CRC likelihood. In recent analyses, dietary shifts towards higher processed meat intake, even amongst younger demographics, have brought heightened awareness to how modern eating patterns might influence cancer rates. It is crucial to recognize that risk is cumulative; thus, dietary choices, particularly those involving processed and red meats, play a prominent role in CRC susceptibility.
Additionally, the elevated cancer risk associated with red meat consumption is a continuing subject of scrutiny. While red meat is labeled as ‘probably carcinogenic,’ the evidence against processed meat is markedly more conclusive. The transition from a traditional diet rich in fiber and lower in processed foods to one dominated by processed options is essential in understanding the rising rates of CRC, particularly in younger populations. Engaging in dietary changes that focus on whole foods, fruits, vegetables, and lean proteins can help lower colorectal cancer risk and promote better health outcomes.
The Role of Lifestyle in Colorectal Cancer Prevention
Adopting a cancer prevention diet involves more than merely reducing processed meat consumption; it encompasses a comprehensive lifestyle approach. Regular physical activity, maintaining a healthy body weight, and limiting alcohol are essential components that complement dietary modifications. Scientific studies indicate that lifestyle factors synergistically interact, compounding the risks associated with unhealthy eating habits. Awareness of how these risk factors intertwine can empower individuals to make informed choices, ultimately aiding in colorectal cancer prevention.
Furthermore, public health initiatives play a significant role in raising awareness about lifestyle-related risk factors for colorectal cancer. By promoting evidence-based dietary guidelines and encouraging individuals to incorporate more plant-based foods into their meals, we can significantly mitigate risks associated with processed meats. Educational campaigns that offer practical strategies for healthier eating can foster a culture of proactive health management, leading not only to reduced CRC incidence but improved overall wellbeing.
Carcinogenic Compounds Found in Processed Meats
The health impact of processed meat consumption is largely attributed to various carcinogenic compounds formed during processing and cooking. Compounds such as nitrates and nitrites, found in many processed meats, are known to convert into nitrosamines, potent carcinogens linked to CRC. Furthermore, cooking methods that include grilling or frying create harmful heterocyclic amines and polycyclic aromatic hydrocarbons, which also contribute to the disease process. Understanding these carcinogenic foods is vital for making informed dietary choices.
In the fight against colorectal cancer, it is crucial to educate the public on the specific compounds associated with processed meats and their mechanisms of action. For instance, heme iron, prevalent in red and processed meat, has been implicated in promoting inflammation and enhancing the formation of cancer-causing agents in the gut. Awareness of these carcinogenic elements can aid in shifting dietary habits away from processed meats, reducing the overall cancer burden in society.
Red Meat and Its Correlation with Cancer Risk
While processed meats have been classified as more hazardous, the consumption of red meat itself also poses a significant cancer risk. Studies indicate that individuals who consume large quantities of red meat are more likely to experience adverse health outcomes, including colorectal cancer. This association requires careful consideration, particularly in dietary guidelines promoting red meat moderation as part of a balanced diet. The challenge lies in understanding the exact mechanisms of how red meat contributes to cancer risk, including the potential role of heme iron and other compounds occurring during deep cooking.
Public dietary guidelines recommend limiting red meat intake while promoting an increase in plant-based foods to mitigate cancer risk. By embracing a diet lower in processed meats and red meat, individuals can potentially lower their risk of CRC. Initiatives that focus on these dietary adjustments not only contribute to cancer prevention but also improve overall health metrics, reinforcing the notion that diet plays an integral role in cancer risk management.
Global Trends in Meat Consumption and Colorectal Cancer Rates
As global consumption trends shift towards increased intake of processed and red meats, correlations with rising colorectal cancer rates have been documented. The significant rise in dietary meat intake over the last few decades, particularly in developed countries, raises alarm over the future landscape of CRC prevalence. Reports indicate that regions with traditionally lower meat consumption now face increasing rates of CRC as lifestyles adapt to include more processed options, underscoring the urgent need for dietary education and advocacy.
Understanding this link emphasizes the need for preventive measures aimed at reducing overall meat consumption. Strategies promoting the benefits of a plant-rich diet over a meat-dominant diet can help counteract the rising statistics of colorectal cancer cases globally. Implementing public health campaigns targeting meat consumption reduction can align dietary habits with recommended public health guidelines, ultimately aiming to lower the burden of CRC.
Genetic Factors in Colorectal Cancer Risk
Recent studies have hinted at genetic predispositions that may interact with dietary habits, particularly regarding processed meat consumption. For individuals with specific genetic markers, the risk of developing colorectal cancer may be significantly amplified with increased processed meat intake. Ongoing research aims to identify these genetic factors, allowing for more personalized dietary recommendations and interventions to minimize CRC risk in vulnerable populations.
The integration of genomic research into colorectal cancer prevention strategies is pivotal for developing tailored approaches. Understanding how genetic backgrounds influence individual responses to diets high in processed meats could lead to innovative preventive measures and targeted recommendations. This knowledge highlights the multifactorial nature of colorectal cancer, reinforcing the need to consider both genetic and lifestyle factors in developing effective prevention guidelines.
Nutritional Interventions for Colorectal Cancer Survivors
For individuals diagnosed with colorectal cancer, understanding the role of diet in influencing survival outcomes remains an essential yet understudied aspect of cancer care. Dietary patterns established post-diagnosis can have profound implications on recovery and long-term health, necessitating a focus on nutritional interventions that support survivorship. While guidelines currently emphasize cancer prevention through dietary modifications, there is growing recognition of the need for research that specifically addresses dietary strategies during and after cancer treatment.
Incorporating evidence-based nutritional guidance for CRC survivors can enhance quality of life and potentially impact survival rates positively. Collaboration between oncology professionals and nutritionists is vital in developing targeted dietary plans that address nutrient needs while minimizing processed meats and other carcinogenic foods. This holistic approach can foster a more comprehensive cancer care strategy, bridging the gap between prevention, treatment, and survivorship.
Empowering Patients Through Dietary Education
To empower patients in their health journeys, effective dietary education and counseling are crucial components of cancer prevention and care. Patients benefit from understanding the risks associated with processed meat and the importance of a balanced diet rich in fruits, vegetables, and whole grains. Regular discussions between healthcare providers and patients about nutrition can motivate individuals to make meaningful changes to their eating habits, ultimately leading to improved health outcomes.
The impact of physician recommendations on patient behavior is significant, and ongoing dialogues surrounding dietary choices can serve as a strong catalyst for change. By providing clear, actionable advice on limiting processed meat and focusing on healthier alternatives, healthcare providers can play a pivotal role in reducing colorectal cancer risks. Creating a supportive environment for patients to explore dietary modifications enables them to take charge of their health and prevention strategies.
Frequently Asked Questions
What is the link between processed meat and colorectal cancer risk factors?
Research indicates that processed meat significantly increases colorectal cancer (CRC) risk. The International Agency for Research on Cancer has classified processed meats as carcinogenic to humans, with strong evidence linking their consumption to heightened CRC rates.
How does processed meat affect colorectal cancer health impact?
Processed meat health impact is substantial, with studies showing that higher consumption correlates with increased colorectal cancer risk. Compounds formed during the processing, such as nitrates and heterocyclic amines, contribute to the carcinogenic nature of these foods.
What dietary changes can help in cancer prevention regarding processed meat?
To prevent colorectal cancer, dietary changes should include reducing processed meat intake significantly, as recommended by the World Cancer Research Fund, which advises consuming very little to no processed meat while focusing on whole foods.
Are there specific carcinogenic foods linked to colorectal cancer?
Yes, certain carcinogenic foods linked to colorectal cancer include processed meats like bacon, sausages, and hot dogs, which contain harmful additives such as nitrates that can increase cancer risk.
What role does red meat play in relation to cancer risk?
Red meat is classified as probably carcinogenic, meaning it may contribute to increased colorectal cancer risk, especially when consumed in conjunction with processed meats, which present a higher risk due to their chemical composition.
How can individuals reduce their colorectal cancer risk factors?
Individuals can reduce colorectal cancer risk factors by adopting a cancer prevention diet that limits processed and red meats, increases fiber-rich foods, maintains a healthy weight, and engages in regular physical activity.
Why is processed meat considered a risk factor for early-onset colorectal cancer?
Processed meat is increasingly recognized as a risk factor for early-onset colorectal cancer, particularly due to dietary shifts and the higher prevalence of processed meat consumption among younger populations.
What actions should healthcare providers take regarding processed meat and colorectal cancer awareness?
Healthcare providers should prioritize counseling patients about the risks associated with processed meat and encourage dietary modifications to mitigate colorectal cancer risk, supporting overall cancer prevention.
| Key Point | Details |
|---|---|
| Colorectal Cancer (CRC) Rising Rates | The incidence of CRC is increasing among younger adults, highlighting the need for education on risk factors. |
| Processed Meat and CRC Link | Processed meat is classified as carcinogenic to humans, associated with higher CRC risk compared to red meat. |
| Carcinogenic Compounds in Processed Meat | Key compounds include heterocyclic amines, nitrates/nitrites, polycyclic aromatic hydrocarbons, and heme iron. |
| Risk Mitigation Strategies | Reducing processed meat intake and understanding genetic risk factors can aid in CRC prevention. |
| Lifestyle and Dietary Changes | Adopting dietary guidelines can lead to a significant reduction in CRC risk. |
Summary
Processed meat colorectal cancer is a critical health issue, as the consumption of processed meats has been strongly linked to an increased risk of colorectal cancer (CRC). Numerous studies have indicated that dietary changes, specifically reducing processed meat intake, can significantly mitigate this risk. With rising CRC rates, especially among younger populations, awareness and education on the dangers of processed meat consumption are vital in implementing effective preventive measures against this preventable disease.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.