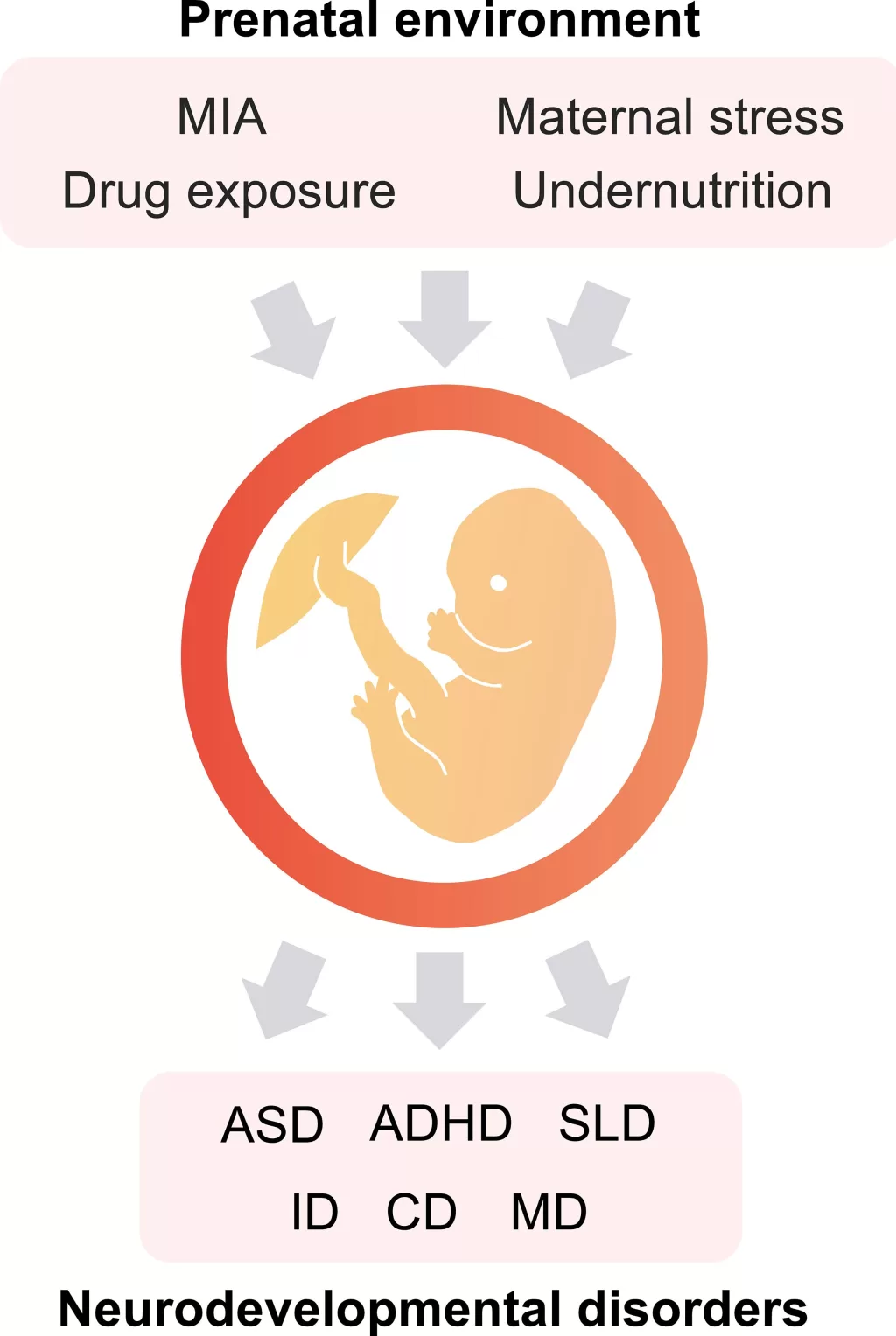
Pregnancy diabetes, specifically gestational diabetes, has emerged as a significant concern due to its potential link to neurodevelopmental disorders such as autism and ADHD. Recent research indicates that women who experience diabetes during pregnancy face an elevated risk, with their children showing a 28% increased likelihood of developing neurodevelopmental disorders compared to those born to mothers without such conditions. This complex interplay between maternal health and child development reveals critical insights into how gestational diabetes can influence neurodevelopmental outcomes. Furthermore, studies demonstrate that children of mothers diagnosed with gestational or pre-gestational diabetes exhibit heightened risks for specific disorders, including a 25% increase in autism and a 30% increase in ADHD. As healthcare professionals emphasize the importance of blood sugar monitoring during pregnancy, understanding these relationships can help mitigate potential impacts on future generations.
The implications of high blood sugar levels during pregnancy extend beyond the immediate health of the expecting mother, influencing the long-term neurological health of the child. Termed maternal diabetes or gestational glucose intolerance, these conditions have been linked to an increased prevalence of neurodiverse traits in offspring, notably increasing the risk of conditions like autism spectrum disorder and attention deficit hyperactivity disorder. Studies have shown that the effects of diabetes during the perinatal period may result in neurodevelopmental challenges that affect children well into their formative years. Such associations highlight the critical intersection between maternal metabolic health and the neurological development of children, underscoring the necessity of thorough screening and intervention strategies. By adopting proactive measures during pregnancy, healthcare providers can play a pivotal role in enhancing the overall health trajectory for both mothers and their children.
Understanding the Link Between Pregnancy Diabetes and Neurodevelopmental Disorders
Recent studies have shed light on the troubling correlation between diabetes during pregnancy and various neurodevelopmental disorders in children. Women with gestational diabetes or pre-gestational diabetes have been shown to have an increased risk of giving birth to children with conditions such as autism and ADHD. This critical finding underscores the importance of meticulous blood sugar management throughout pregnancy. By closely monitoring and maintaining optimal glucose levels, healthcare providers can mitigate potential risks that may adversely affect the child’s neurodevelopmental outcomes.
According to a comprehensive review involving over 56 million pregnancies, mothers diagnosed with diabetes during their gestational period saw a staggering 28% increase in the risk of having offspring with neurodevelopmental issues. Specifically, autism rates were linked to a 25% increase, ADHD a 30% increase, and intellectual disabilities a 32% increase. These statistics emphasize the need for awareness and proactive interventions among expectant mothers, particularly those with pre-existing conditions, as their children may face additional challenges due to neurodevelopmental disorders.
The Importance of Blood Sugar Management During Pregnancy
Effective management of blood sugar levels is paramount for pregnant women, especially those at risk of developing gestational diabetes. Elevated glucose levels can disrupt fetal development, impacting not only physical health but also neurodevelopmental aspects. Health professionals recommend regular screenings and lifestyle modifications to lower the risk of diabetes during pregnancy. Implementing dietary changes, increased physical activity, and frequent monitoring can help maintain stable blood sugar levels, which in turn supports healthier pregnancy outcomes.
Moreover, as emphasized by expert consultations, rigorous screening for diabetes can identify at-risk mothers early in their pregnancy journey. This identification allows for timely intervention strategies that could prevent complications. Research findings highlight that the effects of maternal diabetes extend beyond the immediate perinatal period, affecting the child’s cognitive and emotional development throughout their life. Maintaining vigilant blood sugar control is not just about preventing complications; it plays a crucial role in safeguarding the lifelong health of both mother and child.
Elevated Risks of Autism and ADHD Linked to Maternal Diabetes
The association between maternal diabetes and the heightened risks of autism and ADHD in children has gained considerable attention in recent academic discourse. Specific studies have shown that children born to mothers with gestational diabetes display significant susceptibility to neurodevelopmental challenges. The increased likelihood of autism diagnosis in these children showcases how metabolic conditions during pregnancy might influence brain development, making early detection and management of maternal diabetes critical for optimizing child health.
Furthermore, ADHD emergence has also been notably attributed to diabetes during pregnancy. A well-documented increase in ADHD diagnoses among children of diabetic mothers raises vital questions about the environmental and biological impacts of maternal health on child neurodevelopment. Understanding these links can help parents, healthcare providers, and policymakers focus on preventative measures, ensuring that maternal glucose levels are properly controlled and reducing risks associated with neurodevelopmental disorders.
Exploring Neurodiversity and Its Connection to Pregnancy Complications
Neurodiversity, encompassing conditions such as autism and ADHD, is a crucial concept in understanding how varied brain functions arise from different developmental environments. Maternal health, including conditions like diabetes during pregnancy, plays a pivotal role in shaping these neurodiverse outcomes. By recognizing that neurological differences are a natural variation, society can adopt a more inclusive perspective that respects these differences while also addressing the risks associated with pregnancy complications.
Encouragingly, greater awareness and understanding of neurodiversity can aid in the formulation of support systems that benefit children diagnosed with conditions like autism and ADHD. Practical measures can include resource allocation for tailored education methods and community support to accommodate neurological differences. This not only enhances quality of life for affected individuals but also promotes a societal culture that values inclusivity, stemming from informed maternal health practices.
Gestational Diabetes: Prevention Strategies and Implications
Preventing gestational diabetes requires a multifaceted approach that includes lifestyle alterations, nutritional education, and regular prenatal care. Women can significantly lower their risks by adopting a balanced diet rich in whole grains, fruits, and vegetables while minimizing processed sugars and high-calorie foods. Physical activity during pregnancy, as advised by healthcare providers, not only helps maintain a healthy weight but also improves insulin sensitivity, further reducing the risk of gestational diabetes.
Additionally, education about the symptoms and risks of gestational diabetes is crucial for early diagnosis and management. This education should extend to women with a family history of diabetes or those belonging to high-risk demographic groups. Healthcare providers play a crucial role in delivering this information and encouraging regular screenings, paving the way for healthier pregnancies and better neurodevelopmental outcomes for children.
Insights from MRI Studies on Maternal Diabetes Effects
Emerging research utilizing MRI imaging techniques has provided significant insights into how maternal diabetes affects brain structure and function in offspring. These studies reveal that children exposed to maternal diabetes in utero may develop structural changes in key brain regions, such as the hypothalamus. This area of the brain is crucial for various bodily functions, including hunger regulation and stress responses, which are intricately linked to mental health.
The findings underscore the necessity for continued research and understanding of how environmental factors during pregnancy can shape neurodevelopmental outcomes. With early identification of risks associated with maternal diabetes, healthcare professionals can implement preventative strategies that seek to minimize the likelihood of neurodevelopmental disorders, guiding us toward better health for future generations.
Recognizing the Risk Factors for Gestational Diabetes
Understanding the risk factors associated with gestational diabetes is vital for expecting mothers and healthcare providers alike. Factors such as obesity, advanced maternal age, and being part of certain ethnic groups, including South Asian and African Caribbean backgrounds, significantly increase a woman’s likelihood of developing this pregnancy complication. Recognizing these risks empowers healthcare systems to focus their screening efforts and educational resources on the populations that need them most.
Moreover, awareness of these risk factors enables women to make informed lifestyle choices before and during their pregnancy. Implementing healthier diets, increasing physical activity, and maintaining a healthy weight can greatly diminish the risk of gestational diabetes. As public health initiatives continue to target gestational diabetes, the emphasis on personalized risk assessments and preventative strategies will play a pivotal role in ensuring safer pregnancies.
The Role of Family Support in Managing Maternal Health
Family support is an integral factor in managing maternal health, particularly for women at risk of diabetes during pregnancy. Encouragement from partners and family members can motivate expectant mothers to adhere to prescribed diets and exercise regimens, fostering a healthier lifestyle. A supportive environment promoting wellness not only improves the mother’s health but also lays a foundation for the child’s well-being, reducing risks for neurodevelopmental disorders like autism and ADHD.
Furthermore, family members can participate in healthcare decisions and provide emotional support, making the pregnancy journey more manageable. When families are educated about gestational diabetes, they become valuable allies in the prevention and management of this condition, creating a holistic approach to maternal and child health that benefits the entire family unit.
Community Health Initiatives Addressing Gestational Diabetes
Community health initiatives aimed at addressing gestational diabetes are increasingly vital in promoting awareness and empowering expecting mothers. Programs that offer free screenings, nutritional education workshops, and fitness classes can significantly lower the incidence of diabetes during pregnancy. Such initiatives, supported by local health departments, target at-risk populations, raising awareness about risk factors and prevention strategies.
Moreover, these community efforts often include collaborations with healthcare providers who can offer specialized counsel on managing blood sugar levels throughout pregnancy. By fostering a network of support that encompasses healthcare, social resources, and educational opportunities, these initiatives hold the potential to improve maternal health outcomes and reduce the risk of neurodevelopmental disorders in children.
Frequently Asked Questions
How does gestational diabetes affect neurodevelopmental outcomes in children?
Gestational diabetes, a condition that develops during pregnancy, has been linked to an increased risk of neurodevelopmental disorders in children. Studies suggest that children born to mothers with gestational diabetes face a 28% higher risk of neurodevelopmental disorders compared to those without. Specific conditions, such as autism and ADHD, show a 25% and 30% increased risk, respectively.
What is the connection between diabetes during pregnancy and autism?
Research has established a connection between diabetes during pregnancy and autism. Mothers who experience diabetes, whether gestational or pre-gestational, have children at a 25% increased risk of being diagnosed with autism. This highlights the importance of monitoring blood sugar levels throughout pregnancy.
Can ADHD be linked to maternal diabetes during pregnancy?
Yes, ADHD has been linked to maternal diabetes during pregnancy. Children of mothers who had diabetes while pregnant have a 30% increased risk of developing ADHD. This underscores the significance of proper diabetes management during pregnancy for the child’s neurodevelopmental health.
What role does diligent monitoring of blood sugar play in preventing neurodevelopmental disorders?
Diligent monitoring of blood sugar levels during pregnancy is crucial for preventing neurodevelopmental disorders. Fluctuations in blood sugar can impact fetal development, leading to conditions like autism and ADHD. Consistent monitoring helps manage diabetes effectively and reduces risks for the child.
Are the neurodevelopmental risks greater for mothers with pre-gestational diabetes compared to gestational diabetes?
Yes, studies indicate that the risks for neurodevelopmental disorders are greater for children of mothers with pre-gestational diabetes compared to those who develop gestational diabetes during pregnancy. Pre-gestational diabetes is associated with higher risks of autism, ADHD, and intellectual disabilities.
What preventive measures can reduce the impact of gestational diabetes on neurodevelopmental outcomes?
Preventive measures include early screening and diagnosis of gestational diabetes, maintaining a healthy diet, regular exercise, and monitoring blood sugar levels. These actions can significantly reduce the risk of adverse neurodevelopmental outcomes, such as autism and ADHD, in offspring.
What is the significance of the recent study on diabetes during pregnancy and neurodevelopmental disorders?
The recent study, which reviewed over 202 studies with over 56 million pregnancies, underscores the critical link between diabetes during pregnancy and neurodevelopmental outcomes. It emphasizes that mothers with diabetes are at a heightened risk of having children with disorders like autism and ADHD, highlighting the need for targeted interventions.
How does maternal diabetes impact fetal brain development?
Maternal diabetes can lead to structural and functional changes in the developing brain of the fetus, particularly in areas like the hypothalamus. This brain region is important for both mental and physical health, potentially influencing lifetime risk of neurodevelopmental disorders.
What are the long-term implications of pregnancy diabetes on children’s health?
Children born to mothers with pregnancy diabetes may face long-term health implications, including an increased risk of neurodevelopmental disorders like autism and ADHD. Ensuring proper diabetes management during pregnancy is essential to minimize these risks and promote better overall health for the child.
What are the implications of the study on public health and diabetes screening during pregnancy?
The findings from the study indicate that public health efforts should prioritize diabetes screening and prevention strategies during pregnancy to protect maternal and child health. Increased awareness and proactive management of diabetes can significantly reduce the risk of neurodevelopmental disorders in children.
| Key Points | Details |
|---|---|
| Risk of Neurodevelopmental Disorders | Pregnancy diabetes is linked to a 28% increased risk of any neurodevelopmental disorder in children. |
| Specific Disorders | Increased risks include 25% for autism, 30% for ADHD, and 32% for intellectual disability. |
| Pre-pregnancy vs. Gestational Diabetes | Women with pre-gestational diabetes face greater risks compared to those with gestational diabetes. |
| Research Scope | The study reviewed 202 studies with over 56 million pregnancies. |
| Expert Opinions | Experts emphasize the importance of monitoring diabetes during pregnancy for maternal and fetal health. |
| Gestational Diabetes Statistics | Affects 1 in 20 pregnancies in the UK according to Diabetes UK. |
| Risk Factors for Gestational Diabetes | Higher risk associated with factors like being overweight, previous pregnancies with large babies, and certain ethnic backgrounds. |
| Implications for Baby’s Health | Potential complications include delivery problems, jaundice, and premature birth. |
Summary
Pregnancy diabetes and neurodevelopmental disorders are critically interconnected, as recent studies indicate that this pregnancy complication significantly increases the risk of neurodevelopmental disorders such as autism and ADHD in children. The findings reveal a pressing need for careful monitoring of blood sugar levels during pregnancy to mitigate these risks. It’s crucial for expecting mothers to be aware of the potential impacts on their child’s development and to engage with healthcare providers to manage their diabetes effectively. By prioritizing diabetes monitoring and intervention, we can work towards ensuring better health outcomes for both mothers and their children.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.