Postpartum depression (PPD) is a serious condition that affects approximately 10 to 20 percent of new parents globally, manifesting through a range of debilitating symptoms such as significant mood swings, withdrawal from loved ones, and challenges in bonding with their newborn. Understanding the triggers and neurobiology of PPD is crucial, as these insights can lead to early intervention and better postpartum mental health outcomes. Recent studies have begun to highlight the connection between progesterone levels and the likelihood of developing PPD, paving the way for innovative treatments like zuranolone. This synthetic drug functions similarly to naturally occurring hormones that enhance GABA receptor activity, potentially offering rapid relief from PPD symptoms. By demystifying the neurobiology of PPD, researchers are drawing closer to developing targeted therapies that could transform the experiences of many new parents affected by this condition.
Often referred to as maternal depression, postpartum mood disorders encapsulate a range of emotional challenges faced by individuals after childbirth. These conditions, while commonly recognized under the umbrella of postpartum depression (PPD), include not only the hallmark symptoms but also variations that may impact a parent’s ability to connect with their baby and maintain mental well-being. Recent research delving into hormonal shifts and neurotransmitter imbalances highlights the complexities of postpartum mental health. With alternative treatments emerging, understanding the full spectrum of postpartum depression can foster more effective strategies for support and intervention. By addressing these issues early, we can aim to significantly improve the lives of new parents and their families.
Understanding Postpartum Depression (PPD) Symptoms
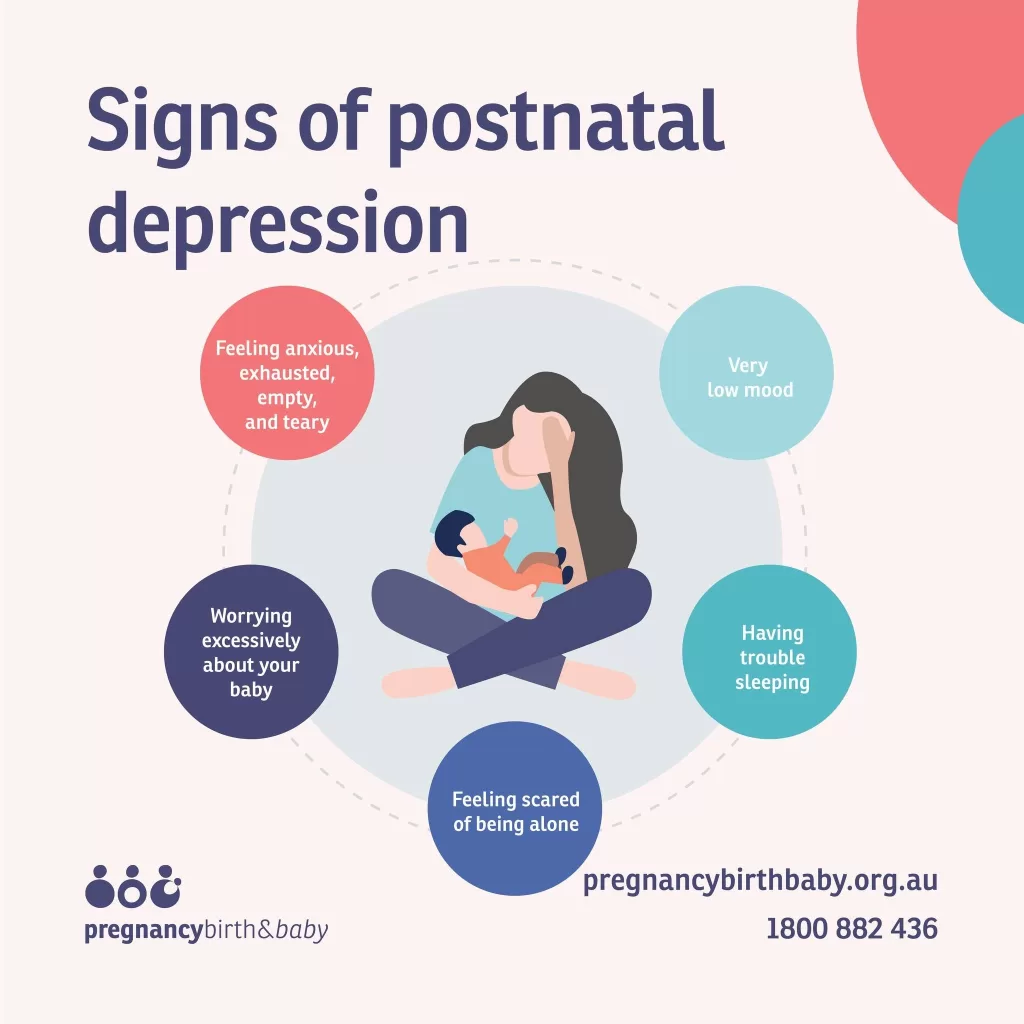
Postpartum depression (PPD) is a significant mental health condition affecting a large number of parents following childbirth. The typical symptoms include severe mood swings, feelings of irritability, overwhelming sadness, and detachment from family and friends. Those suffering from PPD may also experience difficulty in forming a bond with their newborn, which can strain the parent-child relationship. Understanding these symptoms is crucial, as early recognition can lead to timely support and treatment.
Many individuals experiencing PPD display symptoms that differ from traditional major depression, making it essential for clinicians to be aware of the unique features of postpartum mental health. Some patients might report their symptoms as feelings of hopelessness or anxiety, which can easily be misattributed to typical stressors associated with new parenthood. By educating caregivers and families about the varied symptoms of PPD, we can help in identifying affected individuals and guiding them to seek appropriate help.
The Role of Progesterone Levels in PPD
Research has revealed a critical connection between progesterone levels during pregnancy and the onset of postpartum depression. During the third trimester, progesterone undergoes unique metabolic changes in women who later develop PPD. This male hormone, while vital for pregnancy, can have varying effects on mood and neurochemistry, particularly in relation to neurotransmitters like GABA. Higher levels of unprocessed progesterone may disrupt the balance of neurosteroids, negatively impacting GABA’s calming effects and leading to heightened anxiety or depressive symptoms post childbirth.
The interesting intrigue surrounding progesterone metabolism not only sheds light on PPD but also offers a potential biomarker for predicting its onset. With findings indicating that mothers with higher progesterone levels might be more susceptible to developing PPD, there is hope that medical professionals could potentially predict and preemptively treat those at risk, enhancing postpartum mental health outcomes.
Zuranolone Treatment: A New Hope for PPD
One of the most promising developments in treating postpartum depression is the approval of zuranolone, a synthetic derivative of allopregnanolone. This medication addresses the neurobiological aspects of PPD by enhancing GABA functioning in the brain, which can lead to rapid relief from symptoms. Unlike traditional SSRIs that may take weeks to show effectiveness, zuranolone can provide relief within just two weeks, which is critical for new parents who are in dire need of immediate support.
While zuranolone presents a significant advancement in postpartum depression treatment, it is essential to consider safety and practicality. As new parents often struggle with severe fatigue and drowsiness as a side effect of the medication, the presence of additional childcare support is vital during the treatment period. This calls for a multidimensional approach to postpartum care that includes not only medication but also emotional and practical assistance for new parents.
Neurobiology of Postpartum Depression
Understanding the neurobiology of postpartum depression requires detailed insight into how hormonal changes impact brain function and emotional well-being. Unlike major depression, which has traditionally been linked to serotonin and dopamine imbalances, recent studies focus on the role of neurosteroids and their interaction with neurotransmitters after childbirth. These insights open new avenues for research and could lead to more targeted therapeutic approaches, helping to shift the treatment landscape for PPD.
The exploration of neurobiological pathways associated with PPD also emphasizes the need for more nuanced treatment strategies tailored specifically to postpartum individuals. As research continues to elucidate these connections, healthcare providers are better equipped to address the unique psychological challenges posed by hormone fluctuations, potentially minimizing the stigma associated with mental health issues in new parents.
Identifying Predictors of PPD: The Importance of Blood Tests
Identifying predictors of postpartum depression is a critical aspect of improving maternal mental health care. Current research focuses on the potential for blood tests that can accurately predict an individual’s likelihood of developing PPD based on hormone levels, particularly progesterone metabolites. Such tools could significantly enhance early detection and intervention, which are essential in mitigating the long-term effects of untreated PPD on both mothers and infants.
If implemented in prenatal care routines, a predictive blood test could revolutionize how we approach postpartum mental health. It would empower healthcare providers to devise preemptive treatment plans that could be enacted right after childbirth, potentially preventing PPD before it starts. This proactive method underscores the importance of ongoing research and collaboration among medical professionals to establish effective screening and intervention strategies.
The Alarming Statistics of PPD in the U.S.
Despite being a common condition, postpartum depression remains one of the most underdiagnosed mental health disorders in the United States. With statistics indicating that only about 3% of individuals with PPD receive a diagnosis, treatment, and subsequent remission, there is an urgent need for improved access to mental health resources for new parents. The disparity between prevalence and diagnosis suggests a systemic issue in recognizing and addressing the mental health challenges faced during the postpartum period.
Additionally, the alarming fact that maternal suicide accounts for approximately 20% of postpartum deaths highlights the severity of untreated PPD. These statistics not only stress the necessity for better screening practices but also illuminate a broader public health concern regarding maternal wellbeing. Promoting awareness and education around PPD is essential to destigmatizing mental health issues associated with new parenthood, ultimately saving lives and supporting healthier family dynamics.
Long-Term Consequences of Untreated PPD
Untreated postpartum depression can have profound long-term consequences, affecting not only the individual but also their relationships and the emotional development of their children. Research has shown that when mothers experience PPD without adequate treatment, it can hinder their ability to bond with their children, leading to potential developmental implications for the child. The cyclical nature of depression can create challenges in parenting style, which may carry forward into the child’s behavior and emotional health.
Moreover, the effects of untreated PPD extend beyond familial relationships, influencing community and societal dynamics. Mothers facing chronic mental health challenges are less likely to engage socially, which can lead to feelings of isolation. Addressing PPD effectively is crucial—not just for individual recovery but for fostering supportive family units that contribute positively to society. Comprehensive treatment and support can break this cycle, leading to healthier outcomes for future generations.
The Need for Comprehensive Support Systems for New Parents
The importance of establishing comprehensive support systems for new parents cannot be overstated. These systems should encompass mental health resources, educational support, and practical assistance to help alleviate the pressures of new parenthood. Clinics and hospitals can play a vital role by integrating mental health screenings during prenatal and postnatal check-ups, ensuring that new parents have access to the care they need from early on.
Additionally, fostering community support networks can provide crucial emotional and logistic support. Engaging family members, friends, and community resources can promote an environment in which new parents feel validated and supported in their experiences. As societal attitudes continue to shift toward recognizing the importance of mental health, creating robust support networks will not only aid in the prevention of postpartum depression but will enhance the overall postpartum experience.
The Stigma Surrounding Postpartum Mental Health
The stigma surrounding postpartum mental health issues like postpartum depression remains a significant barrier to seeking help. Many new parents feel shame or embarrassment about struggling with their mental health after childbirth, often believing they should have the ability to manage their emotions or situations effectively. This stigma can prevent individuals from sharing their experiences or reaching out for help, resulting in prolonged suffering and avoidable distress.
To combat this stigma, public awareness campaigns and education are essential. By normalizing conversations around postpartum mental health, society can create a supportive environment where new parents feel comfortable discussing their challenges. A cultural shift toward acceptance can assist in destigmatizing PPD, encouraging more individuals to seek assistance and access the appropriate resources that can lead to recovery and improved mental well-being.
Frequently Asked Questions
What are common PPD symptoms that new parents should watch for?
Postpartum depression (PPD) symptoms can manifest as severe mood swings, withdrawal from loved ones, feelings of sadness or hopelessness, and difficulties in bonding with the baby. It’s essential for new parents to be aware of these signs to seek timely help.
How do progesterone levels affect postpartum mental health?
Progesterone levels play a significant role in postpartum mental health. Recent studies suggest that differences in the metabolism of progesterone during pregnancy can influence GABA levels in the brain, which may contribute to the onset of postpartum depression (PPD). Understanding these hormonal changes can help in predicting and managing PPD.
What is zuranolone treatment, and how is it related to PPD?
Zuranolone is a recently approved treatment for postpartum depression (PPD) that acts similarly to allopregnanolone, a metabolite of progesterone. It enhances GABA functioning in the brain, providing relief from PPD symptoms typically within two weeks, a contrast to traditional antidepressants that may take longer to take effect.
Can understanding the neurobiology of PPD help in prevention?
Yes, understanding the neurobiology of postpartum depression (PPD) is crucial for prevention. Research into how progesterone metabolites influence neurotransmitter balance can lead to better predictive tools for PPD, allowing for earlier intervention and treatment.
What challenges do new parents face when treated for PPD?
New parents undergoing treatment for postpartum depression (PPD), particularly with medications like zuranolone, may face challenges such as side effects like drowsiness and fatigue. This can be particularly difficult without childcare support, as they need assistance to care for their baby’s needs during treatment.
Why is PPD often underdiagnosed, and how can blood tests help?
Postpartum depression (PPD) is frequently underdiagnosed due to a lack of awareness and screening practices. Blood tests to identify hormonal imbalances linked to PPD may enable early detection and prompt treatment, significantly improving outcomes for new parents.
What is the link between postpartum depression and suicide risk?
Postpartum depression (PPD) increases the risk of suicidal thoughts and behaviors, contributing to maternal mortality rates. Recognizing and treating PPD effectively is essential as suicide accounts for about 20 percent of postpartum deaths in the U.S.
Are there significant differences between postpartum depression and major depression?
Yes, postpartum depression (PPD) is distinct from major depression in its causes and neurobiological mechanisms. While major depression is often linked to imbalances in neurotransmitters like serotonin and dopamine, PPD is more closely associated with the metabolic processing of progesterone and its effects on GABA.
| Key Points |
|---|
| Postpartum depression (PPD) affects 10-20% of new parents worldwide, leading to severe effects including mood swings and difficulties in bonding with the baby. |
| Risk factors for PPD include prior major depression, but many affected individuals have no previous symptoms. |
| Research indicates potential biomarkers in the metabolism of progesterone that may predict PPD. |
| A blood test could predict PPD risk, allowing for preventive treatment immediately after childbirth. |
| The FDA-approved treatment zuranolone shows potential to reduce PPD symptoms quickly, unlike traditional antidepressants. |
| Undiagnosed PPD can lead to severe consequences, including maternal mortality. |
| There is increasing understanding of the neurobiology of PPD, indicating distinct causes compared to major depression. |
Summary
Postpartum depression (PPD) is a critical mental health issue that affects a significant percentage of new parents each year. With current research revealing biomarkers that may predict the risk of PPD and innovative treatments like zuranolone showing promise, there is hope for early intervention and improved care for those at risk. As awareness grows, it is essential to provide support and treatment for postpartum depression to prevent its severe consequences.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.