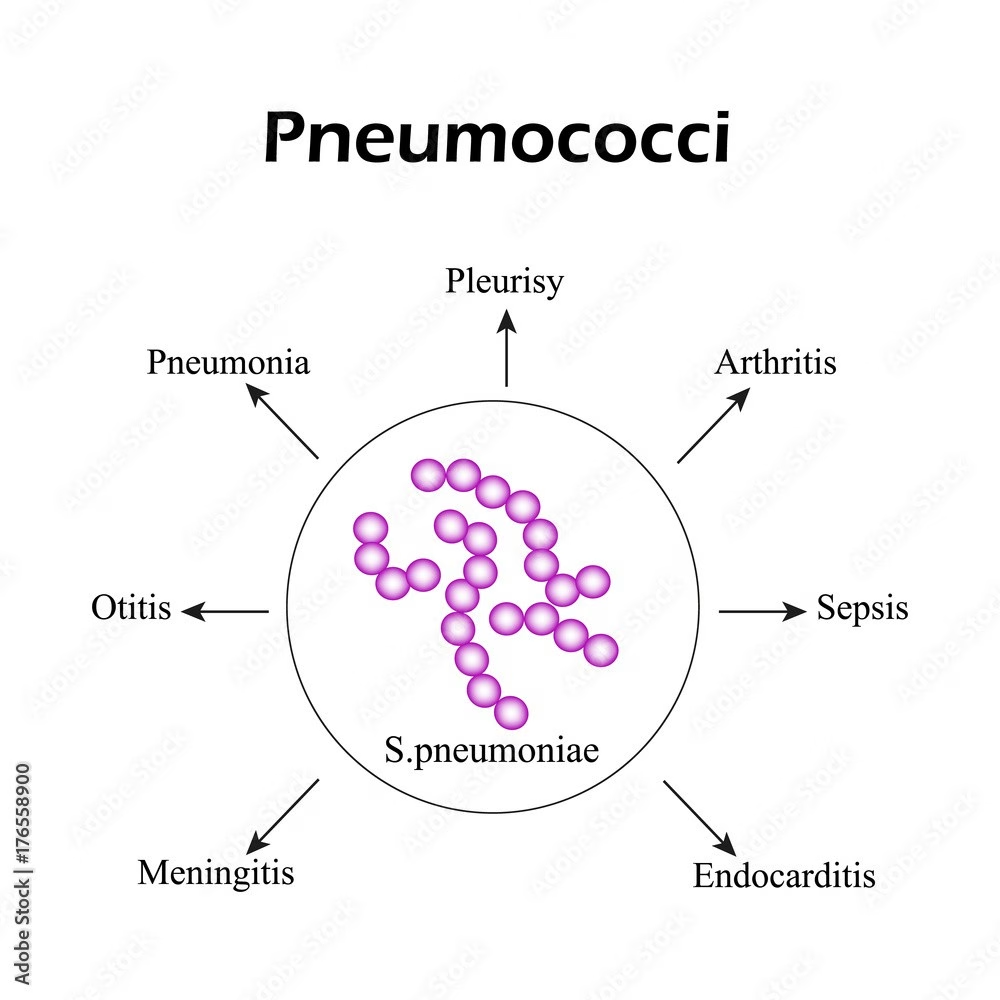
Pneumococcal disease, caused by the bacterium Streptococcus pneumoniae, poses significant health risks, particularly among vulnerable populations such as pregnant women and those in the postpartum period. Emerging research highlights that while pregnant women experience similar infection rates as their nonpregnant counterparts, the risk dramatically escalates post-delivery, suggesting the need for heightened awareness and preventive measures. The pneumococcal vaccine has been identified as a crucial tool in mitigating these risks, although its recommendations for pregnant and postpartum women remain limited. Understanding the relationship between infectious disease in pregnancy and pneumococcal disease is essential for improving maternal health outcomes, especially in the context of postpartum complications. Comprehensive data on pneumococcal disease incidence among these groups can guide healthcare providers in making informed vaccine recommendations to protect both mothers and their newborns.
Invasive pneumococcal disease is a serious concern for maternal health that can affect women during and after pregnancy. This bacterial infection, linked to the pathogen known as Streptococcus pneumoniae, can lead to severe complications, particularly in those who have recently given birth. As new parents navigate the postpartum landscape, it’s critical to recognize the vulnerabilities they may face regarding infectious diseases. Vaccination against pneumococcal disease is increasingly being discussed, especially given the higher susceptibility postpartum. Consequently, addressing these health risks can significantly contribute to enhancing overall maternal and infant well-being.
Understanding Pneumococcal Disease Risks in Childbearing Women
Pneumococcal disease is a significant health concern, particularly among women during pregnancy and the postpartum period. Streptococcus pneumoniae, the bacterium responsible for this disease, can cause severe infections, including pneumonia and meningitis. The incidence of invasive pneumococcal disease (IPD) appears to be similar for pregnant women compared to nonpregnant women but is notably higher for those in the postpartum phase, increasing the urgency for targeted preventive measures such as vaccination.
Research has shown that postpartum women face a 3.5 times higher risk of developing pneumococcal disease than their nonpregnant counterparts. This elevated risk can be attributed to the physiological changes that occur during and after pregnancy, which may compromise the immune system, making these women more susceptible to infections. Consequently, understanding the implications of these risks is essential for developing effective health recommendations and awareness programs aimed at protecting this vulnerable population.
The Role of Pneumococcal Vaccination in Pregnant Women
Vaccination against pneumococcal disease is critical, especially for pregnant women at increased risk due to underlying health conditions. While the Advisory Committee on Immunization Practices has not established specific guidelines for the pneumococcal vaccine in pregnant women, other authorities like the American College of Obstetricians and Gynecologists recommend it for those at higher risk. This underscores the importance of assessing individual risk factors in preventing the severe complications associated with pneumococcal infections.
The pneumococcal vaccine can provide crucial protection against various serotypes of the Streptococcus pneumoniae bacterium. By immunizing pregnant women, healthcare providers can help reduce the incidence of IPD not only in the mothers but also in their infants, as maternal antibodies can transfer through the placenta. Extensive education about potential postpartum complications resulting from pneumococcal disease must accompany vaccination efforts to ensure that women understand the benefits of immunization during pregnancy.
Postpartum Complications Associated with Pneumococcal Disease
The postpartum period poses unique health challenges for women, particularly concerning infectious diseases like pneumococcal disease. Instances of IPD are significantly higher among postpartum women, highlighting the necessity for vigilant monitoring and timely medical intervention. Not only does this increase the risk to the mother’s health, but it can also adversely affect the infant’s well-being, especially if the mother experiences severe complications.
Maternal health during the postpartum phase should be a priority for healthcare providers, as complications from infections can lead to extended recovery times and additional health concerns. Understanding the relationship between postpartum complications and pneumococcal disease can help healthcare practitioners develop comprehensive care strategies that mitigate risks and ensure better health outcomes for mothers and their newborns.
Infectious Diseases in Pregnancy: A Growing Concern
Infectious diseases during pregnancy represent a significant public health issue, with pneumococcal disease being a notable example. The physiological changes that occur throughout pregnancy can alter a woman’s immune response, making her more vulnerable to various infections. This has implications not only for the mother but also for fetal development and health, leading to increased attention to vaccination and preventive health measures.
As the rate of infectious diseases rises globally, understanding how these diseases interact with pregnancy is crucial. Pregnancy-related complications can arise from infections, impacting maternal and infant health outcomes. Addressing these challenges through education, surveillance, and targeted vaccination programs can help reduce the incidence of infectious diseases in pregnancy and ensure the well-being of both mothers and their children.
Analysis of Reporting Trends for Invasive Pneumococcal Disease
Despite the urgency of addressing invasive pneumococcal disease (IPD) risk among pregnant and postpartum women, reporting trends on this issue remain sparse. The data collected from active surveillance systems like the Active Bacterial Core surveillance (ABCs) provide valuable insight into the incidence rates and demographic characteristics associated with IPD cases in childbearing-age women. Enhancing these reporting practices will improve research accuracy and public health responses.
Recent analyses covering the years 2007-2023 indicate that while the incidence of IPD is notably higher in postpartum women compared to their nonpregnant counterparts, pregnant women show similar rates, which prompts further investigation into protective measures. The absence of robust data specific to pregnant women in existing frameworks complicates the development of clear public health recommendations and highlights the need for ongoing surveillance to better protect this vulnerable population.
Long-Term Consequences of Pneumococcal Disease in Postpartum Women
The long-term consequences of developing pneumococcal disease during the postpartum period can be severe, affecting both the mother and child. Among postpartum women, the higher incidence of IPD necessitates careful consideration of a mother’s health and potential long-lasting effects on psychological and physical well-being. Studies indicate that significant infections can lead to complications, including chronic health issues and reduced quality of life.
Moreover, understanding these long-term effects is crucial in developing better care pathways for women who have experienced IPD. Comprehensive post-illness evaluations and supportive care interventions can assist in recovery, which, combined with awareness and preventive measures like vaccination, could significantly improve outcomes for postpartum women facing such serious health threats.
Understanding Serotypes of Streptococcus pneumoniae in Epidemiology
The epidemiology of Streptococcus pneumoniae is complex, with various serotypes contributing to disease incidence. During the research period, the association between specific serotypes and IPD among pregnant and postpartum women has raised questions about the effectiveness of existing vaccines. Surveillance data reveals that certain serotypes—particularly those covered by newer pneumococcal vaccines—are more prevalent among the cases analyzed, thus informing vaccination strategies.
It is crucial for healthcare professionals to stay informed about the changing landscape of serotype distribution and its implications for public health strategies. Understanding which serotypes are responsible for most IPD cases can aid in refining vaccine recommendations, ultimately leading to improved health outcomes for pregnant and postpartum women, as well as the broader community.
Recommendations for Pneumococcal Vaccination During Pregnancy
Based on the existing research findings, recommendations concerning pneumococcal vaccination for pregnant women are essential in guiding healthcare practices. While some women may not be at high risk, those with certain pre-existing health conditions or who live in high-incidence areas should definitely consider vaccination. The evidence suggests that immunizing pregnant women can significantly lower the risk of serious disease during and after pregnancy.
Healthcare providers should prioritize educating women of childbearing age about the pneumococcal vaccine’s benefits, emphasizing the importance of vaccination not just for their health but also for the benefit of their infants. Recommendations should encompass thorough reviews of medical history and individual risk factors to create tailored vaccination plans that enhance maternal and infant health outcomes.
Implications for Future Research on Infection Control in Pregnancy
The ongoing need for additional research on infection control during pregnancy cannot be overstated, given the critical gaps in data concerning pneumococcal disease risks among pregnant and postpartum women. Future studies should aim to delineate the impacts of existing vaccination programs and seek to explore the mechanisms behind the increased susceptibility observed postpartum. Understanding these dynamics can lead to enhanced preventive strategies tailored to this demographic.
Furthermore, collaboration among researchers, public health officials, and healthcare providers is essential in developing comprehensive surveillance systems that monitor infectious diseases in pregnancy. Future research initiatives should incorporate diverse populations and address variable health outcomes related to immunization, ultimately leading to improved guidelines and healthcare practices that protect mothers and their infants from serious Infectious diseases.
Frequently Asked Questions
What are the risks of pneumococcal disease for postpartum women?
Postpartum women experience a 3.5 times higher incidence of invasive pneumococcal disease (IPD) compared to nonpregnant women of childbearing age. This elevated risk highlights the importance of awareness and potential pneumococcal vaccine recommendations to protect maternal health during the postpartum period.
How can the pneumococcal vaccine benefit pregnant women?
The pneumococcal vaccine is recommended for pregnant women who are at increased risk for severe disease. Vaccination can help prevent infections caused by Streptococcus pneumoniae, which can lead to serious health complications during and after pregnancy.
Are pregnant women at risk for infectious diseases like pneumococcal disease?
Research indicates that the incidence of pneumococcal disease is similar for pregnant women compared to nonpregnant peers. However, postpartum women are at greater risk, suggesting that enhanced monitoring and vaccination may be critical for ensuring maternal health.
What is the incidence of pneumococcal disease in pregnant versus postpartum women?
While the incidence of pneumococcal disease in pregnant women is not significantly different from that of nonpregnant women, postpartum women show a marked increase in incidence, making it crucial for healthcare providers to consider pneumococcal vaccine recommendations after childbirth.
What should pregnant women know about Streptococcus pneumoniae risks?
Streptococcus pneumoniae can cause serious bacterial infections, including invasive pneumococcal disease. Pregnant women should be informed about these risks, especially if they have underlying health conditions, to take necessary precautions and consider vaccination.
Why is vaccination against pneumococcal disease important during pregnancy?
Vaccination against pneumococcal disease is important for pregnant women, especially those with underlying health issues, to reduce the risk of serious infections. It plays a significant role in protecting maternal and fetal health against complications related to Streptococcus pneumoniae.
What is the role of the pneumococcal vaccine in reducing postpartum complications?
The pneumococcal vaccine can significantly reduce the risk of invasive pneumococcal disease, which is higher in postpartum women. By vaccinating, we can potentially decrease complications and improve health outcomes for women recovering from childbirth.
How does invasive pneumococcal disease affect maternal health?
Invasive pneumococcal disease can lead to severe complications for mothers, particularly in the postpartum period where the risk is significantly elevated. Awareness and vaccination could mitigate risks associated with severe infections after delivery.
What recommendations exist for the pneumococcal vaccine for women of childbearing age?
While the Advisory Committee on Immunization Practices has not reviewed pneumococcal vaccine use specifically for pregnant or postpartum women, the American College of Obstetricians and Gynecologists recommends it for pregnant women at higher risk, emphasizing the need for targeted recommendations.
What findings support the need for pneumococcal vaccine recommendations during pregnancy?
Research indicates that while pregnant women do not show increased pneumococcal disease risk, there is a significant increase in risk for postpartum women. Consequently, these findings inform the need for specific pneumococcal vaccine guidance for women during and after pregnancy.
| Category | Incidence in Pregnant Women | Incidence in Postpartum Women | Incidence in Nonpregnant Women | Risk Comparison (Postpartum vs Nonpregnant) | PCV Recommendation for Pregnant Women |
|---|---|---|---|---|---|
| Overall Incidence | 0.017 cases per 1,000 person-years (not significantly different from nonpregnant) | 0.088 cases per 1,000 person-years (higher risk) | 0.025 cases per 1,000 person-years | 3.5 times higher for postpartum women | Recommended for those at increased risk by ACOG, no ACIP guidance yet. |
| Demographic Differences | Mean age 29 years, fewer underlying conditions (45.2%) | Mean age 30 years, fewer underlying conditions (41.0%) | Mean age 35 years, more underlying conditions (69.9%) | Women are younger in both pregnant and postpartum groups | ACOG recommends PCV for increased risk groups. |
| Clinical Outcomes | IPD case-fatality rate 2.1% | Favorable outcomes in >75% of cases | IPD case-fatality rate 7.9% (p = 0.014) | Lower case-fatality ratio in pregnant women | No significant variation in serotype caused IPD by pregnancy status. |
Summary
Pneumococcal disease is a significant concern among women of childbearing age, as evidenced by our findings on the incidence of invasive pneumococcal disease (IPD). The research indicates that while pregnant women show similar incidences to nonpregnant women, postpartum women experience a notably higher risk. This highlights the importance of understanding the differences in IPD risk during and after pregnancy. The findings may contribute to future pneumococcal vaccine recommendations, particularly emphasizing the need for guidance for pregnant and postpartum women at risk.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.