The Oropouche virus has emerged as a significant health concern following outbreaks reported from late 2023 into 2024 across South America and the Caribbean. This vector-borne virus, primarily transmitted by infected biting midges, poses risks not only to local populations but also to travelers, as cases linked to travel have been documented in the United States. With the potential for severe health implications, including transmission during pregnancy, public health authorities are closely monitoring the situation. The CDC has issued guidelines aimed at preventing Oropouche virus transmission, especially for pregnant women who are advised to avoid travel to affected areas. As the Oropouche outbreak 2024 continues, understanding how to protect oneself becomes increasingly vital.
The recent surge in cases of Oropouche virus disease highlights the urgent need for awareness regarding this emerging arboviral infection. Often referred to as a vector-borne illness, the Oropouche virus is transmitted via bites from infected midges and mosquitoes, raising concerns about its spread in regions previously unaffected. Health experts are particularly cautious about the implications for pregnant individuals, as the virus has been linked to adverse outcomes in pregnancy. Enhanced CDC Oropouche guidelines are in place to help mitigate risks associated with this virus, especially for those considering travel to areas with reported outbreaks. By focusing on preventing Oropouche virus, communities can better safeguard their populations against this infectious threat.
Understanding the Oropouche Virus and Its Transmission
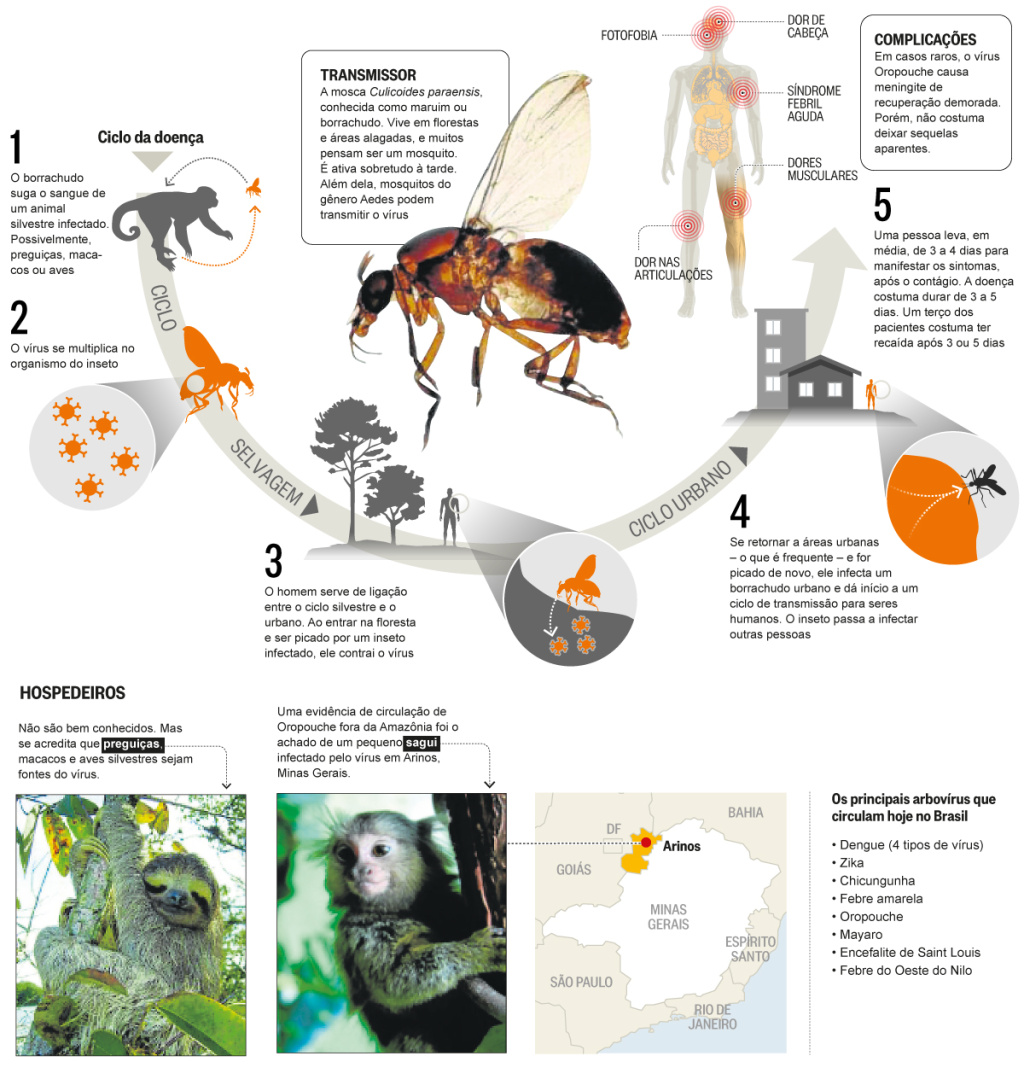
The Oropouche virus is an emerging arbovirus primarily transmitted by infected biting midges, particularly in tropical regions of South America and the Caribbean. In addition to midges, certain mosquito species have also been found to play a role in the transmission of this virus. The recent Oropouche outbreak in 2024 has raised significant public health concerns due to its ability to spread rapidly in affected areas. To prevent Oropouche virus transmission, individuals are advised to take precautions, especially when traveling to regions with reported cases of the virus.
Oropouche virus transmission typically occurs when an uninfected individual is bitten by an infected midge or mosquito. The risk of contracting the virus increases in crowded urban settings or during outdoor activities where exposure to these insects is likely. The CDC recommends that travelers to affected areas adopt protective measures such as wearing long sleeves, using EPA-approved insect repellents, and avoiding peak biting times to mitigate the risk of Oropouche transmission.
Oropouche Virus Disease and Pregnancy Risks
Pregnant women face unique challenges when it comes to the Oropouche virus, as infection during pregnancy has been linked to severe outcomes such as fetal death and congenital birth defects. The transmission of the Oropouche virus from a mother to her fetus poses a significant risk, prompting health authorities to advise pregnant travelers to reconsider non-essential travel to areas under Level 2 Travel Health Notices for Oropouche. The CDC is actively researching the extent of risks associated with Oropouche infection during pregnancy to provide clearer guidelines.
The potential effects of Oropouche virus on pregnancy highlight the importance of preventive measures. Pregnant women should engage in discussions with their healthcare providers regarding travel plans and preventive strategies against insect bites. It is crucial for expectant mothers to stay informed about the latest CDC Oropouche guidelines and to understand the risks involved in traveling to endemic areas.
Preventing Oropouche Virus: Effective Strategies
Preventing Oropouche virus transmission requires a multifaceted approach, particularly for those traveling to endemic regions. The CDC emphasizes the importance of using EPA-registered insect repellents, wearing protective clothing, and employing other environmental control measures to minimize exposure to biting insects. Additionally, travelers are encouraged to review country-specific travel recommendations and health advisories related to Oropouche outbreaks.
Moreover, community participation in vector control efforts can significantly reduce the likelihood of outbreaks. This includes eliminating standing water where mosquitoes breed and maintaining clean environments to deter insect populations. Engaging in these preventive strategies not only protects individual health but also contributes to broader community efforts in controlling the Oropouche virus and preventing future outbreaks.
The CDC’s Role in Managing Oropouche Outbreaks
The Centers for Disease Control and Prevention (CDC) plays a critical role in managing outbreaks of the Oropouche virus through monitoring, research, and public health guidance. In response to the increasing cases of Oropouche disease, the CDC has been actively collaborating with state and local health departments to enhance disease detection and response strategies. This collaboration ensures that health officials are equipped with the knowledge and resources necessary to manage Oropouche cases effectively.
In addition to providing clinical consultations and testing support, the CDC is also focused on developing new diagnostic tests for Oropouche virus to improve detection rates. The agency’s commitment to funding research, particularly in regions most affected by the virus, is vital for understanding vector competence and enhancing regional capacity to respond to Oropouche outbreaks.
Travel Health Guidelines for Oropouche Virus
Travelers to areas affected by the Oropouche virus are urged to follow specific health guidelines to minimize their risk of infection. The CDC has issued clear recommendations, including avoiding travel to regions where there are known cases unless absolutely necessary. For those who must travel, taking precautions against insect bites is crucial, such as applying repellents, wearing appropriate clothing, and staying in accommodations with proper screens or air conditioning.
Furthermore, travelers should stay informed about the latest CDC travel advisories and health notices related to Oropouche virus activity. Being proactive in understanding the current outbreak status can help travelers make informed decisions and take necessary precautions to protect their health while traveling to at-risk areas.
Risks of Sexual Transmission of Oropouche Virus
Recent research has raised concerns about the potential for sexual transmission of the Oropouche virus, particularly following the detection of the virus in the semen of an infected individual. Although no cases of sexual transmission have been confirmed, the possibility highlights the need for further investigation and awareness among travelers. The CDC has responded by issuing interim recommendations for individuals traveling to areas with a Level 1 or 2 Travel Health Notice for Oropouche.
Travelers are advised to engage in safe practices to prevent possible sexual transmission, which includes discussing travel history and health status with partners. Understanding the risks associated with Oropouche virus transmission through sexual activity is essential for protecting both individual and public health during outbreaks.
Impact of Oropouche Virus on Public Health
The emergence of the Oropouche virus as a public health concern reflects the dynamic nature of infectious diseases in our globalized world. With increasing travel, urbanization, and changes in environmental conditions, the risk of outbreaks is heightened. Public health agencies like the CDC continue to monitor the situation closely to provide timely information and guidance to mitigate the impact of Oropouche virus on communities.
Furthermore, the Oropouche virus outbreak serves as a reminder of the interconnectedness of global health. Collaborative efforts between international health organizations and local agencies are critical in addressing the challenges posed by emerging viruses. By sharing data, resources, and best practices, we can work towards reducing the impact of Oropouche and similar diseases in vulnerable populations.
Oropouche Virus Outbreaks: Key Statistics
The 2024 Oropouche outbreak has highlighted several alarming statistics that underscore the urgency of addressing this emerging virus. As of early 2025, there were 108 reported cases of Oropouche disease, including two neuroinvasive cases, across six states and territories. These numbers not only indicate the spread of the virus but also reflect the need for increased awareness and preventive measures to curb future outbreaks.
Understanding the epidemiology and transmission dynamics of the Oropouche virus is essential for effective public health interventions. By analyzing case data and outbreak patterns, health officials can develop targeted strategies to prevent further spread and protect at-risk populations, particularly in areas with a high incidence of Oropouche virus infections.
Community Engagement in Preventing Oropouche Virus
Community engagement is vital in preventing the spread of the Oropouche virus. Local health departments and organizations can play a key role in educating the public about the risks associated with the virus and the importance of protective measures. Initiatives that promote awareness about vector control and personal protective strategies can significantly reduce the incidence of Oropouche disease.
Additionally, involving community members in surveillance and reporting of Oropouche cases can enhance monitoring efforts. Encouraging individuals to report symptoms and seek medical attention can lead to quicker responses and containment of outbreaks, thereby safeguarding public health and reducing the overall impact of the Oropouche virus in affected regions.
Frequently Asked Questions
What are the latest updates on the Oropouche outbreak in 2024?
As of 2024, there have been 108 reported cases of Oropouche virus disease across six states and territories, primarily associated with travel. The CDC is monitoring the situation closely due to the emerging nature of the Oropouche virus.
How is the Oropouche virus transmitted?
The Oropouche virus is primarily transmitted to humans through the bites of infected biting midges, with some mosquito species also capable of spreading the virus. Travelers to affected regions should take precautions to prevent Oropouche virus transmission.
What are the risks of Oropouche virus during pregnancy?
Infection with the Oropouche virus during pregnancy can lead to serious outcomes, including fetal death and birth defects. Pregnant women are advised to avoid non-essential travel to areas with a Level 2 Travel Health Notice for Oropouche.
What guidelines does the CDC provide for preventing Oropouche virus?
The CDC recommends using EPA-registered insect repellents, wearing protective clothing, and controlling mosquito populations around homes to prevent Oropouche virus transmission. Travelers should also stay informed about country-specific health advisories.
Is there a risk of sexual transmission of the Oropouche virus?
Recent studies have detected the Oropouche virus in semen, raising concerns about potential sexual transmission. Although no cases have been confirmed, travelers are advised to adhere to CDC recommendations to minimize risks.
What should I do if I am pregnant and planning to travel to an area affected by Oropouche?
Pregnant travelers should consult with their healthcare providers to discuss travel plans and the associated risks of Oropouche. If travel is unavoidable, strict measures to prevent insect bites must be followed.
How does the CDC monitor and respond to Oropouche virus activity?
The CDC collaborates with public health officials to monitor Oropouche virus activity, provides guidance on managing cases, and develops diagnostic tests. They also disseminate information through their website and health advisories.
What are the symptoms of Oropouche virus disease?
Symptoms of Oropouche virus disease may include fever, headache, joint pain, and rash. In severe cases, it can cause neuroinvasive diseases such as encephalitis or meningitis.
What areas are currently experiencing the Oropouche virus outbreak?
The Oropouche virus outbreak has been reported in several South American and Caribbean countries. Specific areas with active transmission may be outlined in CDC travel health notices.
How can travelers protect themselves against Oropouche virus?
Travelers should use insect repellent, wear long-sleeved clothing, and take precautions against mosquito bites to reduce the risk of Oropouche virus infection while visiting affected areas.
| Key Points | Details |
|---|---|
| Oropouche Virus Outbreaks | Outbreaks reported in South America and the Caribbean from late 2023 to 2024, with travel-associated cases in the U.S. but no local transmission detected. |
| Transmission | Spread by infected biting midges and some mosquitoes. Travelers should protect against bites. |
| Pregnancy Risks | Oropouche virus can be transmitted from mother to fetus, linked to adverse pregnancy outcomes including fetal death. |
| Sexual Transmission | First report of Oropouche in semen raises concerns about possible sexual transmission, but no cases confirmed. |
| Spread in the U.S. | Low likelihood of widespread spread in the continental U.S., some cases may occur in limited areas. |
| Preventive Measures | Use EPA-approved repellents, wear protective clothing, and control insect populations. |
| CDC Actions | Collaborating with public health partners for disease detection, providing guidance, and funding research. |
Summary
The Oropouche virus is a significant emerging health concern, particularly in South America and the Caribbean, due to its potential for severe outcomes, especially during pregnancy. It is crucial for travelers to be aware of the risks associated with this virus and to take preventive measures against insect bites. The CDC is actively monitoring the situation and providing guidance to ensure public safety. As the understanding of Oropouche virus evolves, staying informed about updates and health advisories is essential.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.