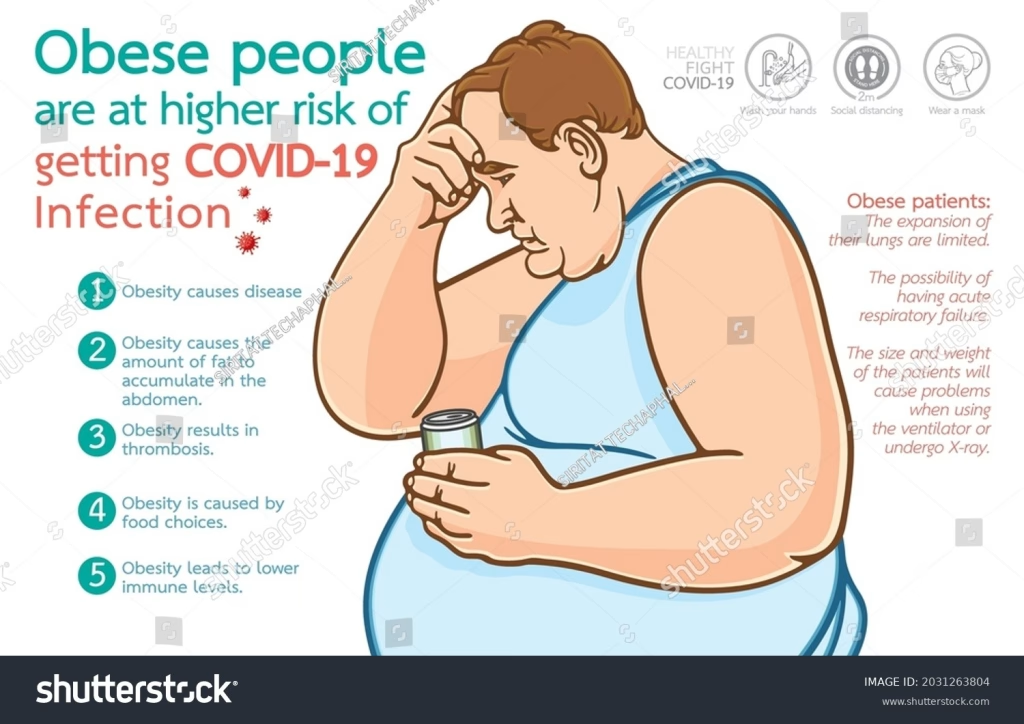
Obesity and infection risk are increasingly recognized as interconnected health issues, with recent studies indicating that those with obesity face a staggering 70% higher likelihood of severe infection-related outcomes. Research conducted by the University of Helsinki highlights that over 10% of adult infection-related deaths globally could be associated with obesity, underscoring its significance as a serious public health concern. With obesity classified using body mass index (BMI), individuals in higher classes are particularly vulnerable; those classified as having class 3 obesity are not only more likely to be hospitalized but also face significantly higher mortality rates from infections. As infection-related deaths continue to climb, particularly during events like the COVID-19 pandemic, the implications of obesity health risks become starkly apparent. It is crucial to address this alarming connection, as obesity may contribute to a growing burden of infection-related deaths and significant healthcare challenges.
When examining the relationship between excess body weight and susceptibility to infections, one cannot overlook the pressing issue of overweight individuals facing heightened risks for severe illness. Terms like body fat and cardiovascular complications showcase the broader implications of these health risks, as higher BMI is linked to numerous pathogens and infectious diseases. The impact of obesity on hospitalization due to infections reveals critical insights into how excess weight can impede the immune response, fostering conditions that favor disease progression. This highlights the significance of tackling overweight conditions, not just for individual health but as a collective goal in public health initiatives aimed at reducing transmission and mortality rates associated with infectious threats. Understanding how the prevalence of overweight populations correlates with infection risk is essential for shaping effective healthcare policies.
The Alarming Link Between Obesity and Infection-Related Deaths
Recent research has unveiled a concerning correlation between obesity and infection-related mortality, highlighting that more than 9% of infection-related deaths globally can be attributed to obesity. As obesity rates surge, particularly in developed countries, the implications stretch far beyond traditional health risks. Individuals with obesity are approximately three times more likely to be hospitalized or die due to infections compared to those who maintain a healthy weight. This trend urges public health officials to take a closer look at obesity not merely as a personal health issue but as a significant contributor to the global health crisis of infectious diseases.
The study by researchers from the University of Helsinki analyzed data from nearly 68,000 adults and reinforced the narrative that obesity dramatically increases the risk of severe infections. This can be due to a variety of factors, including chronic low-grade inflammation and a compromised immune system, which make individuals with higher Body Mass Index (BMI) more susceptible to various pathogens. Furthermore, as healthcare systems become increasingly strained, tackling obesity could potentially alleviate some of the burdens associated with healthcare costs stemming from infectious diseases.
Understanding Severe Infections in Obesity: A Multi-Faceted Issue
Obesity is associated with a diverse array of severe infections, ranging from bacterial and viral to parasitic and fungal infections. The severity of these infections often correlates with the category of obesity, as individuals classified with class 3 obesity show significantly elevated risk factors. This understanding is not merely academic; it has direct implications for treatment, hospitalization, and preventive public health measures. The systematic review of nearly 925 infections sheds light on the complexity of conditions that are exacerbated by obesity, demanding a holistic approach to combat this multifaceted health challenge.
For effective intervention strategies, it is crucial to comprehend why individuals with obesity are particularly vulnerable to infections. Researchers speculate that anatomical, metabolic, and inflammatory factors converge to create an unfavorable environment for immune defense. Notably, lifestyle interventions aimed at weight loss and improving diet could potentially reduce hospitalization rates for infections. Thus, comprehensive strategies that address the behavioral, environmental, and medical components of obesity are essential to enhance overall public health and minimize infection risks.
The Role of BMI in Infection Risk Assessment and Management
Body Mass Index (BMI) plays a significant role in assessing both obesity and associated health risks, including infections. The categorization of individuals into classes based on their BMI provides a framework for understanding how weight can affect susceptibility to infectious diseases. By identifying those within the class 2 and class 3 obesity categories, healthcare providers can implement targeted preventive strategies. The staggering statistics indicate that obesity-related morbidity and mortality due to infections are not only significant but also preventable through effective weight management.
Moreover, the relationship between BMI and infection risks transcends simple statistics. For instance, hospitalizations for conditions such as pneumonia and COVID-19 have shown a stark difference in outcomes based on BMI classes. The implications are clear: healthcare systems must prioritize interventions that promote healthy weight, along with continuous monitoring of vaccination statuses for those at high risk. As the landscape of infectious diseases evolves, leveraging BMI as a part of risk assessment can play a critical role in improving patient outcomes and reducing the overall infection burden on society.
Preventable Infection-Related Deaths Linked to Obesity: A Call to Action
The staggering estimate that between 9% and 11% of global infection-related deaths could be prevented by addressing obesity calls for immediate action. This is particularly pressing as data suggests that obesity-related deaths due to infections have witnessed an increase in recent years. The connection between rising obesity rates and the increased risk of hospitalization and mortality from infectious diseases should kindle concern among policymakers and health professionals alike.
Effective strategies to combat obesity must encompass comprehensive public health policies focused on enhancing access to healthier food options and promoting physical activity. Furthermore, individuals at risk are encouraged to stay up to date with vaccinations to mitigate the chances of complications arising from infections. Emphasizing the need for community support structures and educational initiatives could substantially contribute to reducing obesity’s impact on public health. Addressing the obesity epidemic not only reduces personal health risks but also alleviates pressure on health systems managing preventable infectious diseases.
Emerging Research Trends: Obesity, Immunity, and Infection Resistance
Emerging studies explicitly indicate that obesity compromises immune function and increases vulnerability to various infections, reshaping our understanding of infection resistance. Traditional views of obesity as a static health condition are increasingly being challenged by findings showing that even individuals labeled as ‘healthy’ can experience significant immune impairment. This nuanced understanding emphasizes the need for a dynamic approach to obesity that considers its impact on overall health, particularly regarding infectious diseases.
With the changing landscape of diseases, such as the emergence of new viral strains, investment in research is critical. This research should not only focus on weight loss but also examine the biochemical pathways affected by obesity that lead to increased infection risk. As our understanding of these connections deepens, it may lead to novel therapeutic approaches and interventions tailored not just for obesity management but also for bolstering immune responses in at-risk populations.
Conclusion: The Urgency of Addressing Obesity and Its Infection Risks
In conclusion, the alarming connection between obesity and increased infection risks demands urgent attention and action from both healthcare providers and policymakers. Given the documented correlation between higher BMI and severe infection outcomes, there is an essential need for multifaceted approaches targeting obesity as a means of decreasing infection-related morbidity and mortality rates. By prioritizing obesity management and understanding its implications on public health, communities can protect vulnerable populations and mitigate the effects of infectious diseases that disproportionately impact those with higher BMI.
As global health challenges continue to evolve, addressing obesity with urgency and compassion not only safeguards individual health but also fortifies societal resilience against infectious diseases. Through education, awareness, and proactive health initiatives, we can foster a healthier future free from the burdens of both obesity and its associated risks.
Frequently Asked Questions
What is the relationship between obesity and infection-related deaths?
Recent studies show that obesity may be responsible for more than 10% of adult deaths linked to infections globally. Obesity significantly increases the risk of severe infections, with individuals classified as having class 3 obesity (BMI 40.0 kg/m² or higher) being three times more likely to be hospitalized or die from infectious diseases compared to those with a healthy weight.
How does obesity increase the risk of severe infections?
Obesity can increase infection risk due to various anatomical, metabolic, and immunological factors. These changes create an environment that promotes microbial persistence and disrupts immune pathways, making it harder for the body to fight off infections. Individuals with higher BMI levels tend to experience more severe outcomes from both bacterial and viral infections.
What infections are more common in people with obesity?
Individuals with obesity are at an increased risk for a wide range of infections, including COVID-19, pneumonia, urinary tract infections, skin and soft-tissue infections, and influenza. Specific studies have indicated higher hospitalization rates for these infection types among obese individuals compared to those with healthy body weight.
What is the impact of BMI on infection hospitalization rates?
Research indicates that as BMI increases, so does the likelihood of hospitalization due to infections. For instance, individuals with class 3 obesity have a hospitalization risk that increases by approximately 2.7 to 3.1 times compared to those with normal weight, reflecting a clear correlation between higher BMI and severe infection outcomes.
Can obesity-related deaths from infections be prevented?
Yes, experts estimate that 9% to 11% of global infection-related deaths could be preventable through effective obesity management and health interventions. Addressing obesity with policies promoting healthy eating and physical activity, along with maintaining current vaccinations, can significantly mitigate the risk associated with infections.
What role does chronic inflammation play in obesity and infection risk?
Chronic low-grade inflammation prevalent in obesity can impair immune function, making individuals more susceptible to severe infections. This inflammatory state can promote pathogen growth and disrupt immune responses, highlighting the need for effective obesity management to decrease infection-related risks.
| Key Findings | Details |
|---|---|
| Obesity Risk Increase | Obesity increases the risk of severe infections by 70%, leading to higher rates of hospitalization and death. |
| Statistics from Studies | Analysis included 67,766 adults from Finland and 479,498 from the UK. Follow-up found significant hospitalization and death rates among those with class 3 obesity. |
| Obesity Classifications | Obesity is categorized into three classes based on BMI: Class 1 (30.0-34.9 kg/m²), Class 2 (35.0-39.9 kg/m²), and Class 3 (40.0 kg/m² or higher). |
| Infection-Related Deaths | Approximately 8.6% to 15% of infection-related deaths are attributable to obesity, especially during the COVID-19 pandemic. |
| Global Impact | The highest obesity-related infection death rates were in North Africa and the Middle East, while South Asia reported the lowest. |
Summary
Obesity and infection risk is a critical public health issue, as research indicates that obesity can increase the likelihood of severe infections by up to 70%. This alarming statistic highlights the correlation between rising obesity rates globally and the increased burden of infectious diseases. With over 10% of adult infection-related deaths worldwide linked to obesity, addressing this preventable risk factor becomes imperative. By encouraging healthier lifestyles and ensuring access to medical care, including vaccinations, we can mitigate the dangerous effects of obesity on infection risk and improve overall public health. Immediate action is necessary to combat these trends as we look forward to a healthier future.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.