As monkeypox updates continue to emerge, public health authorities are closely monitoring rising trends in monkeypox cases across the United States. Recently, Maine reported a pediatric monkeypox case, joining California and Florida in documenting infections among children. The CDC monkeypox report highlighted that the U.S. has over 10,768 confirmed cases, with New York leading the count. Despite concerns, health officials have reassured that adequate safety measures are in place for blood donations, minimizing the risk of transmission. In light of these developments, the community is urged to stay informed and vigilant against the spread of this virus while also keeping an eye on other pressing health issues, including influenza news and ongoing COVID-19 updates.
In the recent climate of infectious diseases, updates on the mpox outbreak are capturing significant attention. With a particular focus on cases involving young individuals, the emergence of pediatric monkeypox instances reflects a concerning trend seen in several states. The latest reports from the CDC highlight the critical need for continued vigilance and public awareness amid these developments. As health officials implement strategies to combat transmission, parallels are drawn with ongoing concerns about other respiratory viruses, including influenza and the long-term effects of COVID-19. Staying abreast of such health alerts is essential for communities striving to mitigate outbreaks and safeguard public health.
Understanding the Recent Pediatric Monkeypox Cases
The recent increase in pediatric monkeypox cases has become a significant public health concern, particularly highlighted by the new case reported in Maine involving a resident under the age of 18. As the CDC continues to track monkeypox infections, it is crucial to assess the implications of these adolescent cases. They contribute to the growing understanding of how monkeypox spreads and the necessary public health responses required to protect young populations, especially in states like California and Florida, which also reported similar pediatric cases.
Experts emphasize that monitoring monkeypox cases in children is essential, as these demographics may present unique challenges in treatment and public safety measures. Increased awareness and targeted education programs about monkeypox are vital to mitigate further outbreaks and ensure that both healthcare providers and parents are well-informed about the risks and symptoms. Greater vigilance can lead to timely interventions, safeguarding the health of children who may be more vulnerable during outbreaks.
Latest Monkeypox Updates from the CDC
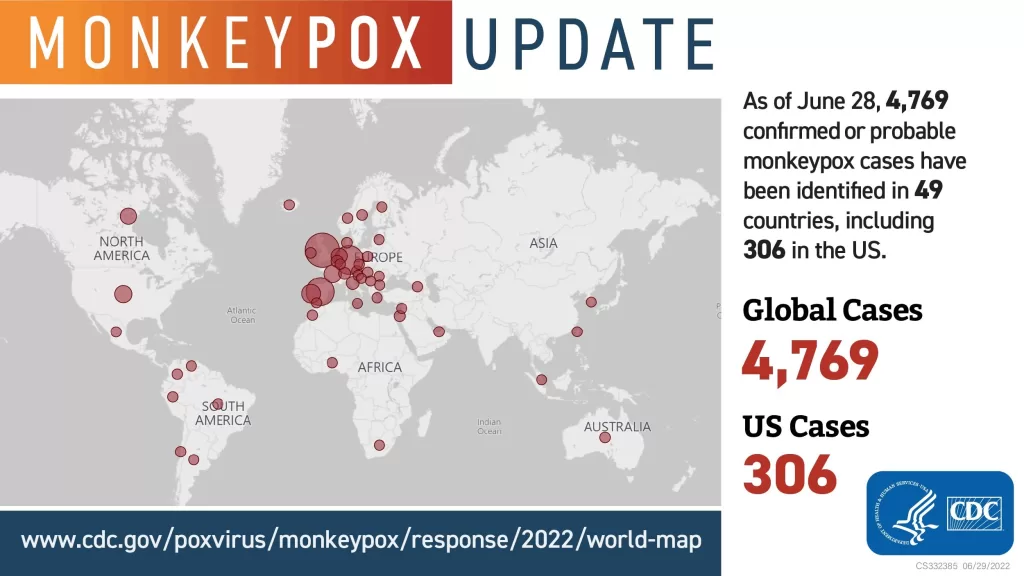
As of August 2022, the CDC has reported a total of 10,768 monkeypox cases across various states, with New York leading the count significantly. The CDC monkeypox report offers critical insights into how the virus is spreading, including geographical data and demographic breakdowns. These updates are vital for establishing targeted strategies to fight the outbreak and educate the public about prevention.
The CDC regularly updates guidelines regarding monkeypox, reflecting the evolving nature of the outbreak and its management strategies. Understanding these reports is crucial for healthcare professionals and the community, as they detail the risk factors associated with monkeypox and provide recommendations for vaccination and treatment. As cases are monitored closely, staying informed about the latest developments will empower communities to respond effectively.
Implications of Monkeypox and Influenza Co-Infections
The intersection of monkeypox epidemics with ongoing influenza cases presents a unique challenge to public health officials. Preliminary studies suggest that individuals infected with both viruses could face more severe health outcomes, necessitating a careful examination of patient management strategies. The CDC’s reports linking monkeypox updates with influenza news indicate a potential for complicated interactions that call for meticulous tracking and research.
Healthcare providers are urged to maintain high vigilance during the flu season, especially with a backdrop of rising monkeypox cases. Understanding how these infections may co-occur can inform best practices for diagnosis and treatment. Additionally, educational campaigns must stress the importance of vaccination not only against influenza but also for monkeypox to protect vulnerable populations and curb further spread.
Parental Guidance on Pediatric Monkeypox
For parents, the emergence of pediatric monkeypox cases calls for heightened awareness and vigilance. Understanding the symptoms and potential transmission routes of monkeypox can empower parents to take preventive measures, such as limiting contact with individuals known to have been infected. Additionally, educating their children about hygiene practices can play a significant role in preventing outbreaks.
Healthcare professionals should actively communicate with parents about monkeypox, advising them on the importance of reporting any symptoms in their children. Sharing accurate information about vaccination and prevention strategies is critical in increasing community resilience against this virus. Parental education initiatives can help mitigate fears and facilitate proactive health management.
Antimicrobial Stewardship in the Context of Monkeypox
The link between antimicrobial stewardship and emerging infections like monkeypox is a growing area of interest for researchers and public health officials. While monkeypox is a viral infection, the importance of managing antibiotics and other antimicrobials during viral epidemics cannot be overstressed. The use of antibiotics should be judicious, as misuse can lead to resistance, further complicating treatment efforts during outbreaks.
Investigating the impacts of antibiotic use during periods of heightened monkeypox activity can provide crucial insights into improving treatment protocols. As healthcare systems navigate complex scenarios involving viral and bacterial infections, integrating antimicrobial stewardship principles will be vital to safeguard patient health and optimize resource allocation effectively.
Impact of COVID-19 on Monkeypox Case Management
The ongoing COVID-19 pandemic significantly influences how public health departments manage monkeypox cases. Hospitals and healthcare infrastructures are still under pressure due to COVID-19 infections, which may hinder the ability to respond swiftly to monkeypox outbreaks. The integration of COVID-19 updates with monkeypox case management strategies is essential for ensuring adequate resource allocation and care delivery.
Understanding the crossover between these two infections can improve epidemiological models and response tactics. Healthcare providers are encouraged to consider the compounding effects of COVID-19 on monkeypox case progression, as individuals with COVID-19 may exhibit overlapping symptoms or face challenging health outcomes due to dual infections.
Healthcare Use Post-Infection and Monkeypox
Recent studies have shown that healthcare use remains elevated for six months post-infection for illnesses such as COVID-19, raising questions about the potential long-term healthcare impact of monkeypox infections. With the rise of monkeypox cases, understanding treatment pathways and healthcare utilization becomes crucial. These insights can guide public health strategies to improve patient care and outcomes among monkeypox and other viral infections.
Patterns of healthcare utilization post-infection can inform how resources should be allocated and where preventive measures may need to be enhanced. Tracking the healthcare journeys of monkeypox patients will provide valuable data to improve future outbreak responses and better allocate healthcare resources during such public health crises.
Evaluating the Safety of Vaccines During Monkeypox Outbreaks
With the emergence of new cases, debates regarding the safety and efficacy of vaccines for monkeypox are paramount. Recent studies have reinforced the notion that vaccinations can effectively prevent severe outcomes from infections. Public health messaging must evolve to communicate the advantages of vaccination clearly, especially during outbreaks.
Healthcare providers play an essential role in dispelling myths surrounding vaccines while fostering environments where patients feel confident in receiving their vaccinations. This is particularly important for frontline healthcare workers who will be directly involved in caring for monkeypox patients. Clear guidelines and educational resources will support action against misinformation and encourage vaccination adherence.
Antimicrobial Resistance and Its Relevance to Emerging Infections
Antimicrobial resistance (AMR) is a growing concern, particularly in the context of emerging infections like monkeypox. The simultaneous management of AMR and infectious disease outbreaks necessitates a comprehensive approach to infection control. Public health strategies must address the overlap between antibiotic use and the emergence of viral illnesses, as inappropriate antimicrobial use can exacerbate health crises.
Combatting AMR alongside managing monkeypox outbreaks can provide insights into better practices in infection prevention. By focusing on responsible antimicrobial use during outbreaks, healthcare facilities can play a crucial role in mitigating potential resistance patterns that complicate treatment for patients who contract monkeypox or other infectious diseases.
Frequently Asked Questions
What are the latest monkeypox updates from the CDC regarding cases in children?
As of August 12, 2022, the CDC reported that Maine confirmed a pediatric monkeypox case, adding to the cases in California and Florida. This brings attention to the ongoing monkeypox situation in the U.S., where the total number of monkeypox cases has reached 10,768. Parents are encouraged to stay informed about vaccination and prevention measures.
How does the CDC track monkeypox cases, and what are the current statistics?
The CDC actively monitors monkeypox cases across the United States, providing regular updates. As of August 12, 2022, the total number of monkeypox cases nationwide is 10,768, with New York leading at 2,187 cases, followed by California and Florida. For the most updated statistics, refer to the CDC monkeypox report.
Are there any recent studies on monkeypox transmission, particularly regarding animals?
Recent research published in *The Lancet* has indicated the possibility of human-to-dog transmission of monkeypox in France. This highlights the need for vigilance regarding animal reservoirs of the monkeypox virus as its transmission in humans increases.
What precautions should blood donation centers take concerning monkeypox?
According to the FDA’s recent updates, blood donation centers do not need additional screenings for monkeypox, as transmission through blood transfusion has not been documented. Centers routinely assess potential risks post-donation, ensuring safety for recipients.
How is monkeypox impacting pediatric populations, and what states have reported cases?
Pediatric monkeypox cases have been reported in several states, including Maine, California, and Florida. As the virus spreads, healthcare providers and parents should monitor for symptoms and follow public health guidance to protect children.
What are some important recent findings on monkeypox from health institutions?
Important findings include the confirmation of human-to-dog monkeypox transmission and insights into pediatric cases reported by states like Maine. Continuous updates from the CDC and other health bodies are crucial as new research emerges.
| Key Points | Details |
|---|---|
| Maine Reports Pediatric Monkeypox Case | A resident under 18 confirmed; now three states have pediatric cases (California, Florida, Maine). Total U.S. cases reach 10,768. |
| FDA Addresses Blood Donation Safety | The FDA affirms no additional screening for monkeypox is necessary for blood donors, citing no transmission through transfusion globally. |
| Research on Human-to-Dog Transmission | Evidence of monkeypox transmission from humans to dogs reported in France raises concern over new animal reservoirs. |
| Antimicrobial Stewardship Amid Flu Season | A study links inpatient antibiotic use in U.S. hospitals to influenza activity, emphasizing stewardship’s role in infection control. |
| H3N2v Flu Cases in West Virginia | Two new variant flu infections linked to an agricultural fair reported, both in individuals under 18. |
| Leptospirosis Outbreak in Tanzania | Outbreak sickens 20, with three fatalities; focused on farmers due to occupational exposure. |
Summary
Monkeypox updates indicate a rising concern as new pediatric cases appear in states like Maine, joining California and Florida. The CDC has reported a total of over 10,768 cases across the United States, highlighting the need for continued awareness and preventative measures. Recent findings also raise alarms about potential animal reservoirs following a documented transmission of monkeypox from humans to dogs in France. Amid these developments, public health authorities stress the importance of monitoring and managing both monkeypox and flu cases, reinforcing antimicrobial stewardship to mitigate the impact of the ongoing public health crisis.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.