The uptake of the MMR vaccine is a critical public health concern, especially as the world grapples with the resurgence of measles outbreaks. Recent findings indicate a troubling trend of diminishing MMR vaccination rates, which heightens the risk of individuals contracting this highly contagious disease. Vaccine hesitancy plays a significant role in these trends, with parents increasingly hesitant to vaccinate their children against measles, mumps, and rubella. Public health interventions must address these concerns and reinforce the importance of MMR vaccinations to protect communities from rising measles cases. As researchers uncover detailed insights into vaccination patterns, it becomes ever more crucial to promote awareness and facilitate dialogue around the necessity of immunization in safeguarding public health.
Addressing the challenges surrounding the MMR immunization is essential, particularly given the growing alarm about recent measles outbreaks. Understanding the landscape of MMR inoculation among children has revealed concerning gaps in vaccination rates that could result in heightened vulnerability. Parental apprehensions, often driven by misinformation, have led to increased vaccine reluctance, making it vital for health officials to implement strategic public health campaigns. By highlighting the connection between MMR vaccination and community immunity, stakeholders can mitigate the incidence of measles cases effectively. Ultimately, fostering a culture of informed choice about vaccinations can empower parents to ensure their children are vaccinated, thus safeguarding community health.
Understanding MMR Vaccine Uptake Trends
The recent study published in Nature Health highlights a significant concern regarding MMR vaccine uptake, indicating an overall vaccination rate of only 64%. This low figure raises alarms among public health officials, as it falls well below the community immunity threshold of 92-94%. Regions such as West Texas and southern New Mexico are particularly troubling, where the low uptake correlates directly with rising measles cases. In comparison, areas in the Northeast and Upper Midwest show much higher vaccination rates, suggesting geographical disparities that need to be addressed to prevent outbreaks.
The study, drawing from a substantial sample of over 22,000 parents across more than 3,100 counties, reveals that MMR vaccination rates vary significantly depending on several factors such as parental age and socioeconomic status. This variance suggests that certain communities are at a higher risk for measles outbreaks, particularly where vaccine hesitancy is prevalent and misinformation concerning MMR vaccination persists. Understanding these trends is crucial for developing effective public health strategies tailored to individual community needs.
The Impact of Vaccine Hesitancy on MMR Rates
Vaccine hesitancy remains one of the primary obstacles to achieving higher MMR vaccination rates. Factors contributing to this hesitancy include misinformation, fear of vaccine side effects, and a general distrust in health authorities. The impact of this hesitancy extends beyond individual choices, as it can lead to significant gaps in community immunity, thereby increasing the risk of measles outbreaks. Public health officials must actively counter these narratives with accurate information to reassure parents about the safety and efficacy of the MMR vaccine.
In the face of vaccine hesitancy, targeted public health interventions are essential. These interventions could take various forms, including community outreach programs, collaborations with local health providers, and educational campaigns aimed at dispelling myths surrounding vaccines. By fostering an understanding of the importance of MMR vaccine uptake, health officials can facilitate better communication and trust between parents and healthcare providers, ultimately leading to increased vaccination rates and a reduction in measles cases.
Regional Disparities in MMR Vaccination Rates
The geographic analysis of MMR vaccination rates shows stark contrasts across different regions in the United States. For instance, states like Massachusetts exhibit uptake rates upwards of 79%, while others such as New Mexico report figures as low as 61.6%. This discrepancy underscores the complexity of public health challenges—some areas are more vulnerable to measles outbreaks than others. Such disparities often relate to socio-economic factors, access to healthcare, and public sentiment towards vaccines.
Addressing these regional disparities requires localized strategies that cater to the unique characteristics of each community. Public health interventions could be more effective if they consider factors like local culture, historical attitudes toward vaccination, and the presence of healthcare resources. Only by understanding and addressing these disparities can health officials implement successful measures to boost MMR vaccination rates, ultimately protecting children from preventable diseases like measles.
Community Immunity and Its Importance in Preventing Measles Outbreaks
Community immunity, also known as herd immunity, is critical in the prevention of measles outbreaks. For the MMR vaccine, achieving an immunization coverage of approximately 92% to 94% is necessary to prevent sustained transmission of the disease. The current average of 64% vaccine uptake illustrates the urgent need for public health campaigns to educate communities on the importance of maintaining high vaccination rates to ensure community immunity.
Without robust community immunity, not only do specific populations remain vulnerable, but the risk of outbreaks increases significantly. Recent data indicating a rise in measles cases correlates strongly with areas that fall short of this immunization threshold. Therefore, public health strategies must focus on encouraging vaccination through education, accessibility, and addressing vaccine hesitancy to ensure that communities move toward maintaining or exceeding the necessary immunization levels.
The Role of Local Health Departments in Vaccine Distribution
Local health departments play a pivotal role in the oversight and distribution of the MMR vaccine. They are often the first point of contact for families seeking vaccination for their children. As the study noted, understanding local community constraints is essential for effective health interventions. Therefore, empowering local authorities with better data and resources will enable them to devise tailored vaccination campaigns that resonate more effectively with their populations.
Moreover, local health departments can collaborate with community organizations to identify underserved populations and improve health literacy around vaccines. By integrating their efforts with schools, childcare programs, and community outreach initiatives, local departments can enhance MMR vaccination rates and ultimately improve public health outcomes in their areas. This ground-up approach is paramount in combatting the rise of measles cases linked to low MMR coverage.
Effective Surveillance Systems for Vaccine Uptake
The need for effective surveillance systems to monitor MMR vaccine uptake has never been more pronounced. Current models relying on telephone surveys or school-entry data often miss critical insights, particularly from marginalized communities that may not have strong access to traditional healthcare systems. The study employing participatory surveillance provides a model for harnessing community data to get accurate estimates of vaccination coverage.
Utilizing innovative technology and community engagement can significantly enhance existing surveillance frameworks. By collecting real-time data on vaccination status at the community level, health authorities can quickly identify gaps in coverage and respond proactively to emerging vaccination concerns. This model not only empowers public health interventions but also engages communities in the collective effort of improving their public health outcomes.
Addressing Children’s Health Needs in Underserved Communities
Underserved communities face unique challenges regarding access to healthcare, which directly impacts MMR vaccine uptake. Factors such as lack of transportation, healthcare facilities, and knowledge about vaccination benefits perpetuate low vaccination rates in these areas. Public health officials must prioritize strategies to address these disparities to ensure all children receive necessary vaccinations.
By focusing on tailored outreach programs that engage underserved populations, health authorities can work to dismantle barriers that contribute to low MMR uptake. Availability of vaccines in community settings, targeted education sessions, and partnerships with local organizations can play significant roles in increasing vaccination rates and protecting vulnerable populations from measles outbreaks.
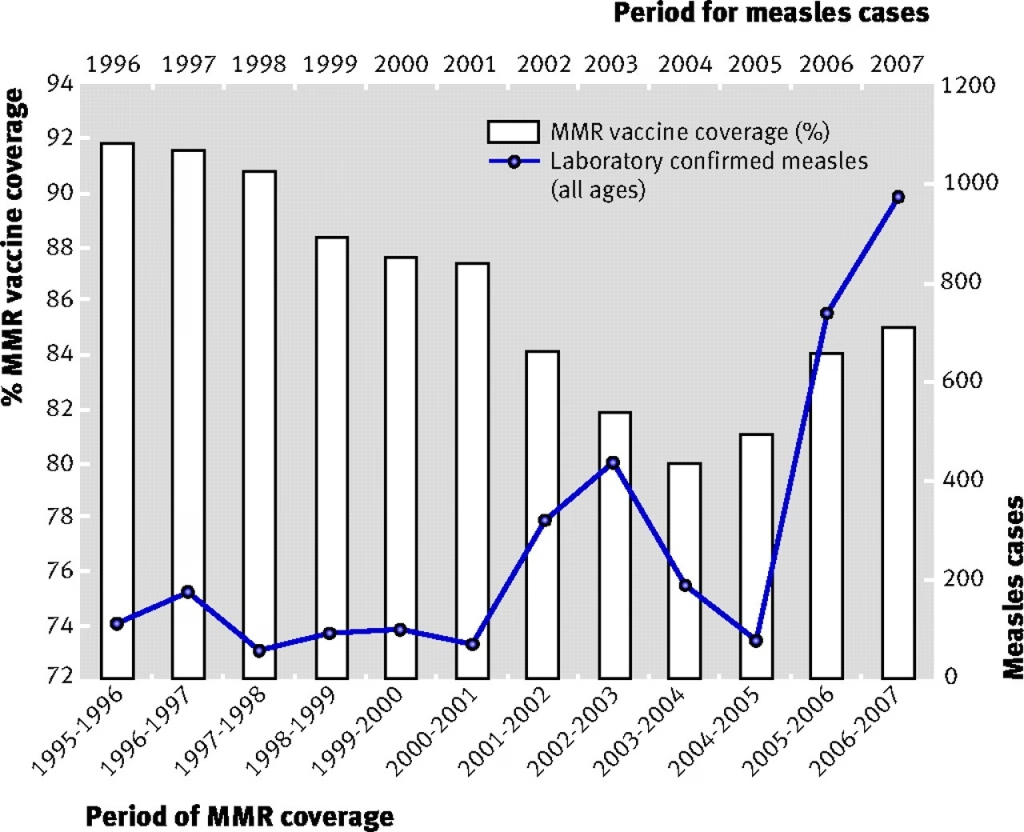
The Connection Between MMR Vaccine Coverage and Outbreaks
The direct correlation between MMR vaccine coverage and outbreaks of measles cannot be overstated. Regions with low vaccination rates often become hotbeds for disease transmission, as witnessed in recent measles cases linked to areas with inadequate vaccine uptake. As highlighted in the study, understanding these dynamics is essential for public health planning and outbreak prevention.
In light of rising measles cases, public health measures must be implemented to reinforce the importance of vaccination. By increasing awareness and fostering an environment that encourages vaccination through multiple channels, communities can significantly mitigate the risk of outbreaks and protect public health.
Future Public Health Considerations for MMR Vaccination
Looking ahead, it is imperative for public health officials to consider innovative solutions that address the factors contributing to declining MMR vaccination rates. This includes strategic partnerships with primary healthcare providers to ensure they provide consistent, evidence-based information on the importance of vaccinations.
Additionally, public health campaigns that leverage social media and grassroots initiatives can substantially influence parental attitudes towards vaccinations. By creating a supportive environment that prioritizes children’s health and addresses concerns raised by vaccine hesitancy, we can work towards raising overall MMR vaccine uptake and preventing future outbreaks.
Frequently Asked Questions
What are the current MMR vaccination rates across the United States?
Current estimates indicate that MMR vaccination uptake stands at 64.0%, reflecting about 71.1% of eligible children vaccinated with at least one dose. This rate is significantly below the community immunity threshold of 92% to 94%, highlighting a public health concern amid rising measles cases.
How does low MMR vaccine uptake contribute to measles outbreaks?
Low MMR vaccine uptake has been associated with an increased risk of measles outbreaks. Areas with vaccination rates below the community immunity threshold are particularly vulnerable, as evidenced by ongoing outbreaks in states like New Mexico and Texas, where low immunization correlates with significant measles cases.
What factors contribute to vaccine hesitancy regarding the MMR vaccine?
Vaccine hesitancy concerning the MMR vaccine can be attributed to various factors including misinformation about vaccine safety, fear of side effects, and cultural beliefs. This hesitancy negatively impacts MMR vaccination rates, increasing susceptibility to measles outbreaks.
What public health interventions can increase MMR vaccination rates?
Effective public health interventions to boost MMR vaccination rates include targeted outreach programs, community engagement initiatives, and educational campaigns aimed at addressing vaccine hesitancy. These strategies can help build trust between parents and healthcare providers, ultimately promoting higher vaccination uptake.
Which regions in the U.S. have the highest and lowest MMR vaccination rates?
High MMR vaccine uptake has been documented primarily in the Northeast, Midwest, and Pacific regions, while low coverage is notably found in West Texas, southern New Mexico, and parts of Mississippi. This geographic disparity is crucial to understand for addressing local vaccine-related challenges.
Why is detailed county-level data important for MMR vaccine uptake?
Detailed county-level data on MMR vaccine uptake is essential as it reveals significant variations in vaccination coverage that can inform tailored public health responses. It aids in identifying communities at higher risk for measles outbreaks, making targeted interventions more effective.
What specific populations are often excluded from MMR vaccination analyses?
Current surveillance systems may overlook vulnerable populations such as homeschooled children and uninsured families, leading to underestimations of MMR vaccination rates. Addressing these gaps is crucial for enhancing public health initiatives aimed at increasing overall vaccine uptake.
How have measles cases changed with the current MMR vaccination levels?
As MMR vaccination levels have declined, measles cases have notably increased, with 171 cases reported in 2025, the majority linked to outbreaks. This trend underscores the direct correlation between MMR vaccine uptake and the incidence of measles in vulnerable communities.
| Key Point | Details |
|---|---|
| Study Purpose | To map MMR vaccine uptake and identify areas of low coverage, indicating outbreak risks. |
| Data Collection | Survey of 22,062 parents across 3,109 U.S. counties from July 2023 to April 2024. |
| Vaccine Uptake Statistics | Overall uptake at 64.0%. Coverage varies widely across states and counties: 61.6% in New Mexico to 79.1% in Massachusetts. |
| Risk Groups | Counties categorized into five groups based on vaccination coverage: very high, high, medium, low, and lowest risk. |
| Geographical Insights | High coverage in Northeast and Midwest; low coverage in West Texas, Mississippi, and rural Southeast. |
| Current Public Health Implications | Need for targeted public health interventions to address low vaccine uptake and counteract declining coverage. |
| Vaccine Hesitancy Factors | Declining MMR coverage is fueled by multifaceted vaccine hesitancy and misinformation. |
Summary
MMR vaccine uptake is critically low across many areas in the United States, which increases the risk of measles outbreaks. A recent comprehensive study reveals that the overall vaccination rate stands at only 64%, significantly below the community immunity threshold of 92-94%. The alarming variations in uptake across different states and counties underscore the need for public health interventions tailored to specific communities. Furthermore, addressing vaccine hesitancy is essential to rebuild trust and ultimately improve the MMR vaccination rates.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.