Methicillin-Susceptible Staphylococcus aureus skin infections (MSSA) pose significant challenges, especially in pediatric populations. Recent case studies have highlighted the alarming role of Panton-Valentine leukocidin in exacerbating these infections, leading to increased severity and frequency of skin lesions. In a striking example, a 7-year-old girl in Japan suffered from recurrent skin infections linked to a specific MSSA strain that also infected multiple family members, indicating possible familial transmission of skin infections. The persistent nature of these skin issues, despite various treatment strategies including impetigo treatment and MSSA decolonization efforts, showcases the complexity of managing these infections. As public health concerns continue to rise, understanding the dynamics of MSSA infections is imperative for developing effective prevention and treatment protocols.
Skin infections caused by Methicillin-Susceptible Staphylococcus aureus (MSSA) are increasingly recognized as a public health issue, particularly in children. The virulence of strains associated with Panton-Valentine leukocidin complicates standard treatment approaches, necessitating a closer look at both direct and family transmission of skin infections. The recurrent nature of these conditions often leads to painful lesions, even when patients receive therapies such as mupirocin. Continued research into MSSA and its associated risks, especially among pediatric populations, is crucial for refining existing decolonization strategies and improving outcomes. Understanding the mechanisms behind these persistent infections will aid in better prevention and management strategies.
Understanding Methicillin-Susceptible Staphylococcus aureus Skin Infections
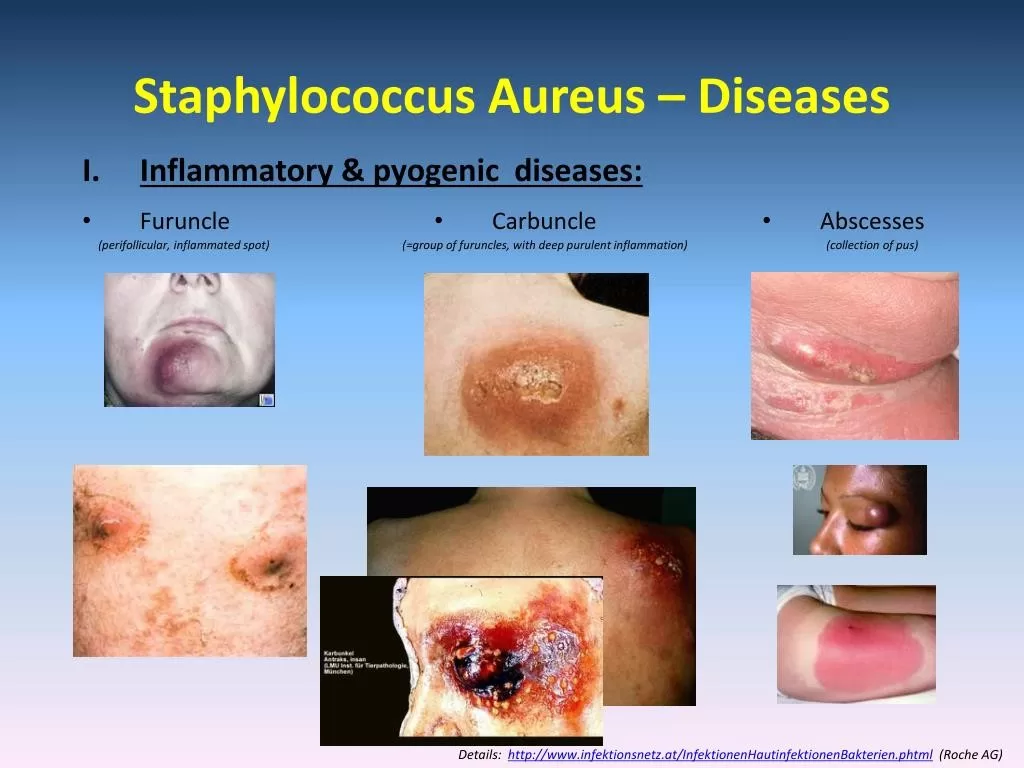
Methicillin-Susceptible Staphylococcus aureus (MSSA) skin infections are a significant concern, particularly among children with predisposed conditions such as atopic dermatitis. These infections can lead to severe dermatological issues, as observed in a case involving a 7-year-old girl from Japan. She displayed recurrent furunculosis and impetigo that resisted conventional treatments, a common scenario in pediatrics where skin integrity is often compromised due to underlying skin conditions. The strains of MSSA involved often contain virulence factors such as Panton-Valentine leukocidin, which exacerbate skin damage and promote further infection.
In your understanding of MSSA skin infections, it’s critical to acknowledge their transmission dynamics, particularly within families. As illustrated in the case study, family members displayed similar skin lesions indicating a common source of infection and emphasizing the importance of considering familial transmission in treatment strategies. In such situations, it’s essential to implement an integrated approach that includes educational components for families on hygiene practices and possible decolonization strategies to break the cycle of transmission.
Role of Panton-Valentine Leukocidin in Pediatric Skin Infections
Panton-Valentine leukocidin (PVL) is a critical virulence factor associated with severe skin infections caused by Staphylococcus aureus. In pediatric cases, such as the reported instance of a girl with recurrent MSSA infections, PVL presence played a key role in the manifestation of conditions like furunculosis and impetigo. This toxin promotes skin necrosis, leading to more complicated infections that necessitate aggressive treatment and management strategies. Understanding the mechanisms of PVL can significantly influence the approach taken by healthcare providers when managing such infections.
Furthermore, the implications of PVL presence are profound, not only affecting the patient’s recovery pace but also posing risks of intrafamilial transmission, as seen in this case. Multiple family members were diagnosed with similar infections, suggesting that the highly virulent MSSA strain may facilitate quick spread among close contacts. Thus, having an awareness of PVL’s impact is crucial in healthcare settings, particularly in pediatric wards where families often interact closely. Clinicians must be vigilant in monitoring for signs of transmission to ensure timely interventions.
Family Transmission of Skin Infections: Risks and Prevention
Skin infections, particularly those caused by MSSA, often exhibit a disturbing tendency to spread within families. The case of a 7-year-old girl in Japan highlights the challenges associated with intrafamilial transmission, as multiple family members were infected with the same strain. Such scenarios are common in pediatric contexts, given that children frequently share close living spaces, play areas, and personal items, which can facilitate the spread of pathogenic organisms. Understanding how these infections propagate emphasizes the necessity for practitioners to not only treat the affected individual but also to address the family as a unit.
Preventive measures must be prioritized to reduce the risk of ongoing transmission within families affected by MSSA skin infections. Strategies such as consistent hand hygiene, regular cleaning of shared spaces, and proper wound care education can make significant differences. Furthermore, implementing a decolonization protocol within households, while often challenging, is essential for limiting recurrent infections. Alternatives beyond conventional mupirocin ointment may need consideration to effectively break the cycle of infection and protect all family members.
Challenges in Treating Recurrent Impetigo in Pediatrics
Impetigo is a highly contagious skin infection common in pediatric populations, leading to significant challenges in treatment, particularly when caused by MSSA strains that possess virulence factors like PVL. The reported case of a young girl with persistent impetigo underscores the complexity of managing this condition when traditional antimicrobial therapies fail. Recurrences, despite initial treatment, suggest the need for a deeper exploration of underlying factors, including potential barriers to effective therapy and the immune response of the child.
Moreover, the difficulty experienced in eradicating the infection highlights the need for individualized treatment plans that may incorporate not only topical treatments but also systemic antibiotics if warranted. Education for parents about recognizing impetigo symptoms and an understanding of its transmissibility can empower families to take proactive measures in treatment and prevention, thus reducing reinfection rates among siblings and other family members.
Effective MSSA Decolonization Strategies: A Need for Innovation
Decolonization of Methicillin-Susceptible Staphylococcus aureus (MSSA) is critical for managing skin infections effectively; however, traditional decolonization strategies often seem inadequate as highlighted by the unsuccessful attempts in familial cases of recombination infections. In the case of the 7-year-old girl, methods such as extensive cleansing regimens or topical mupirocin were ineffective in preventing recurrences, underscoring a significant hurdle in pediatric treatment protocols. Thus, the development of innovative decolonization methods is crucial to enhancing the quality of care for patients suffering from recurrent infections.
Exploring new avenues of decolonization could include the introduction of alternative topical agents with proven efficacy or the integration of systemic antibiotics specifically targeting MSSA. Additionally, comprehensive education regarding personal hygiene practices and environmental cleanliness within the household may offer supplementary benefits. For families grappling with recurrent MSSA infections, a concerted effort amongst healthcare professionals to customize decolonization strategies is necessary to prevent ongoing infections and reduce the risk of transmission to other family members.
Importance of Continued Research in Pediatric Skin Infections
Research into pediatric skin infections, particularly those caused by virulent strains like MSSA, is essential for advancing treatment protocols and improving patient outcomes. As evidenced in the outlined case study, lack of effective decolonization strategies necessitates a greater emphasis on scientific investigations that explore the relationship between specific virulence factors such as Panton-Valentine leukocidin and the clinical manifestations of skin infections. Continued study in this area can lead to a better understanding of infection dynamics and potential new therapies.
Moreover, analysis of family transmission patterns offers vital insights into preventive strategies, as highlighted by the confirmed familial links among the infected individuals in this case. Ongoing research is vital to assess the efficacy of various treatment modalities and the biological mechanisms underlying MSSA virulence, particularly in children predisposed to skin conditions. The ultimate goal is to generate robust evidence that translates directly into clinical practice and improves management strategies for pediatric patients facing recurrent infections.
Explaining the Pathophysiology of MSSA Skin Infections
The pathophysiology of infections caused by Methicillin-Susceptible Staphylococcus aureus (MSSA) is complex and involves multiple factors that contribute to the infection’s development and persistence, especially in pediatric patients. Understanding how MSSA invades the skin, produces toxins, and evades the immune response is essential for devising effective treatment strategies. The presence of virulence factors like Panton-Valentine leukocidin significantly exacerbates the inflammatory response, creating conditions that can lead to severe skin damage and facilitate the production of pus-filled lesions.
Moreover, this understanding aids in identifying high-risk patients, enabling healthcare providers to implement early and aggressive interventions. Recognizing skin infections as dynamic processes influenced by host factors such as age, immune status, and skin integrity is crucial in pediatric settings. A comprehensive grasp of the pathophysiology behind MSSA infections can inform both preventive and therapeutic strategies, reducing the incidence of recurrent infections among vulnerable populations.
Monitoring and Managing Antibiotic Resistance
The increasing prevalence of antibiotic resistance among pathogenic bacteria, including MSSA, poses significant challenges in treating skin infections. In cases where decolonization strategies fail, such as in the case of the 7-year-old girl, concerns over resistance to commonly used antibiotics like mupirocin arise. Continuous monitoring of resistance patterns is imperative for healthcare providers in order to adjust treatment protocols based on the evolving landscape of bacterial resistance, ensuring that effective therapies remain accessible for managing pediatric skin infections.
Furthermore, the rise of resistance can have widespread implications, extending beyond individual patients to affect families and communities at large. Policymakers and health organizations must work collaboratively to establish guidelines that promote appropriate antibiotic use and educate families on the importance of adhering to prescribed treatment plans to combat the development of resistance. By employing a proactive stance on antibiotic management, we can safeguard the efficacy of current treatments while also protecting future generations from the threat of resistant infections.
Frequently Asked Questions
What are the common symptoms of Methicillin-Susceptible Staphylococcus aureus skin infections in children?
Common symptoms of Methicillin-Susceptible Staphylococcus aureus (MSSA) skin infections in children include red, swollen lesions, pus-filled blisters, and pain at the infection site. Conditions like impetigo, furuncles, and cellulitis are often observed. Children may also experience itchiness and discomfort, especially in cases associated with conditions like atopic dermatitis.
How does Panton-Valentine leukocidin contribute to Methicillin-Susceptible Staphylococcus aureus skin infections?
Panton-Valentine leukocidin (PVL) is a toxin produced by some strains of Methicillin-Susceptible Staphylococcus aureus (MSSA), leading to increased virulence. It can cause severe skin infections, particularly in children, by destroying white blood cells and exacerbating tissue damage, resulting in more serious lesions and potential complications.
What strategies can be used for MSSA decolonization to prevent recurrent skin infections in children?
MSSA decolonization strategies often include daily use of antiseptic washes, regular hand hygiene, and intranasal mupirocin application. While these methods aim to reduce skin and nasal carriage of MSSA, effectiveness can vary, especially in family clusters where transmission is common.
How can families prevent the transmission of Methicillin-Susceptible Staphylococcus aureus skin infections?
To prevent family transmission of Methicillin-Susceptible Staphylococcus aureus (MSSA) skin infections, families should practice good hygiene, such as regular hand washing, avoiding sharing personal items (like towels and razors), and promptly treating any skin lesions. Monitoring and screening family members can also help identify and manage infections early.
What are the treatment options for pediatric impetigo caused by Methicillin-Susceptible Staphylococcus aureus?
Treatment options for pediatric impetigo caused by Methicillin-Susceptible Staphylococcus aureus (MSSA) typically include topical antibiotics like mupirocin and oral antibiotics if the infection is more extensive. Additionally, maintaining proper wound care and hygiene can support recovery and minimize symptom recurrence.
What role does atopic dermatitis play in susceptibility to Methicillin-Susceptible Staphylococcus aureus skin infections?
Atopic dermatitis can increase susceptibility to Methicillin-Susceptible Staphylococcus aureus (MSSA) skin infections due to broken skin barriers and itch-scratch cycles that exacerbate lesions. Children with atopic dermatitis are more prone to develop secondary skin infections, including impetigo, when MSSA is present.
Can Methicillin-Susceptible Staphylococcus aureus skin infections in children resolve spontaneously?
While some Methicillin-Susceptible Staphylococcus aureus (MSSA) skin infections may resolve on their own, especially mild cases, many require medical intervention to prevent complications. Monitoring the infection closely and consulting with a healthcare professional is essential to ensure appropriate management.
| Key Points | Description |
|---|---|
| Case Overview | A 7-year-old girl with recurrent skin infections caused by MSSA identified as clonal complex 188. |
| Family Transmission | Several family members also showed similar MSSA skin infections, indicating potential intrafamilial spread. |
| Decolonization Attempts | Standard decolonization strategies such as cleaning and mupirocin ointment proved ineffective. |
| Genetic Findings | Phylogenetic analysis showed strains were related, confirming familial transmission; no resistance to mupirocin was detected. |
| Patient Prognosis | The frequency of lesions decreased as the patient aged beyond 10 years. |
| Management Challenges | Highlights the need for refined or alternative decolonization strategies in managing MSSA SSTIs. |
Summary
Methicillin-Susceptible Staphylococcus aureus skin infections are significant in pediatric cases, as demonstrated by a study of a 7-year-old girl in Japan with recurrent infections. This case reveals the challenges faced when conventional treatment methods fail and emphasizes the importance of understanding family transmission dynamics. Managing Methicillin-Susceptible Staphylococcus aureus skin infections requires innovative approaches to effectively prevent recurrences and protect those at high risk, particularly in familial contexts.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.