Lupus symptoms often serve as a perplexing puzzle for those affected, manifesting in various forms such as joint pain, fatigue, and rashes. This chronic autoimmune disease can create significant challenges as it frequently leads to delays in a proper lupus diagnosis, leaving many in the dark about their health. With an estimated 16,000 new cases diagnosed each year in the United States alone, awareness of lupus symptoms is critical for timely intervention. Common indicators can resemble those of other conditions, causing even seasoned healthcare professionals to overlook key signs, which can result in dangerous lupus flare-ups and long-term organ damage. Understanding these symptoms is essential not only for patients facing this mysterious illness but also for healthcare providers aiming to offer effective lupus treatment and support.
When discussing the manifestations of systemic lupus erythematosus, terms like autoimmune responses and chronic inflammatory conditions often arise. Individuals may face a diverse symptom profile that encompasses pain, fatigue, and distinct rashes, making it difficult to pinpoint the underlying issue. The erratic nature of lupus can mirror other health problems, raising concerns among patients and their families. Recognizing these fluctuations and seeking timely lupus diagnosis become crucial steps in managing one’s health effectively. Ultimately, comprehensive knowledge of these signs can empower patients, guiding them towards appropriate lupus treatment strategies.
Understanding Lupus Symptoms: The Silent Signals of an Autoimmune Disease
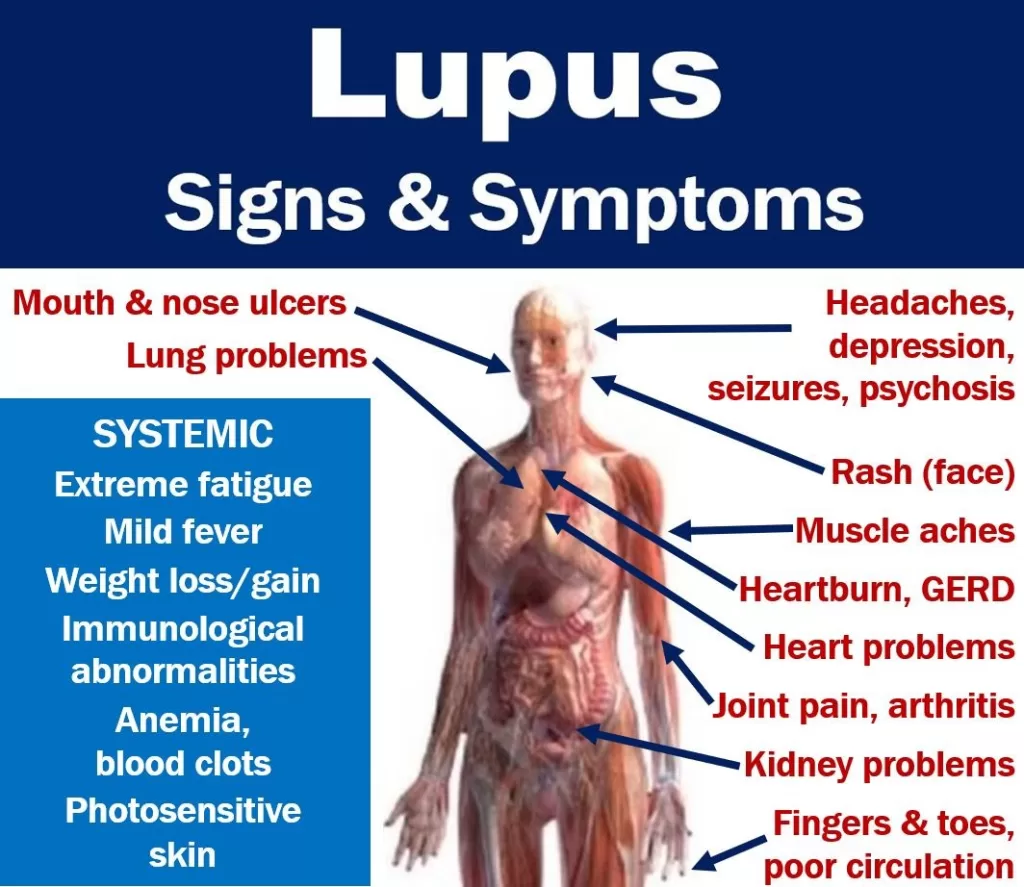
Lupus symptoms vary widely among individuals and can often be mistaken for other medical conditions. The most common symptoms include joint pain, fatigue, and rashes. Patients may notice a distinctive butterfly-shaped rash across their cheeks and nose, which is often one of the first visible signs of the disease. However, due to the non-specific nature of many symptoms, such as low-grade fever or hair loss, individuals might not realize they need a lupus diagnosis until damage has been done. Recognizing these subtle signs is essential for timely intervention.
Chronic fatigue is another frequent complaint among lupus patients, and it can be debilitating. For some, this overwhelming exhaustion can seem disproportionate to the level of activity they engage in, leading them to believe it is caused by simple lifestyle factors. Additionally, systemic symptoms like Raynaud’s phenomenon, which causes fingers and toes to turn white or blue in cold conditions, may go unnoticed but are significant indicators of lupus. Understanding and acknowledging lupus symptoms is crucial, as they can lead to serious health consequences if left unchecked.
Lupus Diagnosis: The Struggles to Identify an Autoimmune Disease
Diagnosing lupus can be a complicated and lengthy process, often taking years before an accurate diagnosis is made. Initially, physicians typically rely on blood tests, such as the antinuclear antibody (ANA) test, which can indicate the presence of various autoimmune diseases. However, a positive ANA test alone is not definitive for lupus; therefore, doctors must evaluate a combination of lab results and clinical symptoms. Many patients experience a frustrating journey of misdiagnoses, adding to the complexity of obtaining appropriate lupus treatment.
Healthcare professionals often also assess kidney function through urine tests since lupus can severely affect kidney health. Patients may present with protein or blood in their urine—indicators of potential kidney involvement. This multifaceted approach to lupus diagnosis highlights the importance of a comprehensive evaluation by specialists. Rheumatologists play a critical role in deciphering this complex puzzle, ensuring patients receive the correct diagnosis and appropriate management.
Treatment Options for Lupus: Managing an Autoimmune Disease
Although there is currently no cure for lupus, effective management strategies have emerged that focus on controlling the overactive immune system. Treatment usually begins with medications like hydroxychloroquine, which is widely used due to its mild side effects. It helps reduce systemic inflammation, particularly beneficial for patients experiencing joint pain and skin rash. However, for some individuals, especially those with more severe manifestations, stronger immunosuppressive drugs may be necessary despite associated risks such as increased susceptibility to infections.
Ongoing research into targeted therapies offers promising avenues for lupus treatment. Unlike traditional immunosuppressants which broadly dampen immune responses, these new drugs aim to specifically address faulty immune mechanisms. Early studies indicate a possible path to remission, allowing some patients to reduce or discontinue their medication safely. This evolving landscape of lupus treatment reflects a shift towards more personalized approaches that could enhance patient quality of life and reduce long-term health complications.
Preventing Lupus Flare-Ups: Tips for Patients
Lupus flare-ups can significantly impact a patient’s daily life, sometimes occurring unexpectedly and leading to serious complications. Preventative measures are critical in managing this unpredictable condition. One effective strategy includes avoiding excessive sun exposure and using a broad-spectrum sunscreen with a high SPF. Ultraviolet (UV) rays can trigger an autoimmune response, thus triggering a flare-up. Additionally, patients are encouraged to maintain consistent vaccinations to prevent infections that could instigate lupus activity.
In addition to sun protection, adopting an anti-inflammatory diet may contribute to overall health and potentially minimize flare-ups. Although more research is needed to provide specific dietary guidelines, a focus on healthy eating can bolster the immune system’s resilience against stressors. Moreover, managing stress is crucial; both emotional and physical stress can exacerbate lupus symptoms. By actively participating in their care and maintaining a collaborative relationship with healthcare providers, lupus patients can better navigate their condition and improve their quality of life.
The Impact of Risk Factors on Lupus Development
Understanding lupus risk factors is essential for prevention and awareness. While the exact cause of lupus remains elusive, several known factors may influence the likelihood of developing this autoimmune disease. Genetic predisposition plays a significant role; lupus often runs in families, indicating a possible hereditary component. Environmental triggers also seem to be involved, such as certain infections or exposure to sunlight, which can activate the immune system in individuals who are genetically susceptible.
Furthermore, hormonal influences are noteworthy, as around 90% of lupus patients are women. The onset of symptoms often correlates with hormonal changes, such as those occurring during menstruation or pregnancy. This suggests that hormonal factors may increase the likelihood of lupus flare-ups, necessitating careful observation in these periods. Understanding these risk factors helps not only in awareness but also in targeting preventive strategies for those at higher risk, thereby diminishing the impact of this chronic condition.
Living with Lupus: Emotional and Physical Challenges
Living with lupus entails coping with both physical and emotional challenges. The unpredictability of symptoms can lead to anxiety and depression, as patients frequently question when another flare-up might occur. Chronic pain, fatigue, and the threat of complications can strain relationships and affect social interactions. Patients often feel isolated due to the invisible nature of their illness, making understanding by friends and family crucial. Support networks, such as lupus support groups, can provide companionship and valuable coping strategies.
Moreover, managing daily activities can become more complex when dealing with lupus. Simple tasks may seem overwhelming during flare-ups, necessitating a flexible approach to work and personal commitments. Encouragingly, many patients learn to adapt by pacing themselves and prioritizing self-care. Techniques like mindfulness, gentle exercise, and seeking psychological support can enhance emotional well-being, helping patients lead fulfilling lives despite the challenges posed by lupus.
Understanding the Importance of Regular Check-ups for Lupus Patients
Regular check-ups with healthcare providers are vital for individuals living with lupus. These visits allow for monitoring the disease’s progression and adjusting treatment plans accordingly—a critical component in minimizing the risk of serious complications such as kidney disease and cardiovascular issues. Rheumatologists often perform routine blood tests to assess inflammation markers and overall health, ensuring timely interventions if needed. Keeping open lines of communication with healthcare teams can empower patients in managing their condition effectively.
During these check-ups, discussions about lifestyle modifications, symptom management strategies, and potential new treatments may take place. Since lupus can affect various body systems, interdisciplinary approaches that involve dermatologists, nephrologists, and immunologists may be necessary. Regular evaluations foster collaborative care, allowing for comprehensive management of lupus that addresses both medical and psychological aspects. This proactive approach equips patients with the knowledge and support they need to navigate their lupus journey confidently.
Exploring Current Research on Lupus Treatment Innovations
Research into lupus is rapidly progressing, with scientists exploring innovative treatment options that could change the management of this autoimmune disease significantly. Current studies focus on better understanding the immune pathways involved in lupus, aiming to develop therapies that directly target these mechanisms. For instance, researchers are investigating biologic medications that specifically inhibit the overactive immune cells implicated in lupus, moving beyond conventional treatments that suppress the entire immune system.
Furthermore, clinical trials are vital for unveiling new drugs and assessing their effectiveness in managing lupus symptoms. Patients participating in research studies often gain access to cutting-edge therapies not yet widely available, thus offering hope for improved disease management. As studies continue to expand our understanding of lupus, there is optimism that new insights will lead to more effective, tailored treatments that not only manage symptoms but also target the disease at its core.
The Role of Family and Social Support in Managing Lupus
The support of family and friends plays a crucial role in the management of lupus. Emotional support helps patients cope with the challenges of living with a chronic condition, as understanding and empathetic listeners can alleviate feelings of isolation. Close relationships offer encouragement during difficult periods, and family members who are informed about the disease can assist in recognizing symptoms, thus playing a proactive role in patient care.
Additionally, social support can enhance compliance with treatment regimens and encourage a healthy lifestyle. Patients often benefit from shared activities, such as gentle exercise or joining support groups, which foster a sense of community. Open conversations about lupus within families help demystify the disease and encourage constructive approaches to managing flare-ups. Ultimately, a strong support network significantly contributes to a higher quality of life for lupus patients.
Frequently Asked Questions
What are the most common symptoms associated with lupus?
Lupus symptoms can vary widely, but the most common include joint pain, fatigue, skin rashes (notably the butterfly rash across the cheeks and nose), and hair loss. Other symptoms may include fever, sensitivity to sunlight, and Raynaud’s syndrome, where fingers or toes change color in cold conditions. Due to the vague nature of these symptoms, they are often overlooked, leading to delays in lupus diagnosis.
How do lupus symptoms differ during flare-ups?
During lupus flare-ups, patients may experience a worsening of their symptoms, such as increased joint pain, more pronounced rashes, and heightened fatigue. These flare-ups can be triggered by various factors, including stress, UV exposure, or infections. Recognizing these triggers is important for managing lupus symptoms effectively and preventing severe complications.
What role do lupus risk factors play in symptom development?
Lupus risk factors, such as genetic predisposition, gender (with a higher prevalence in women), and environmental triggers like sunlight and viruses, can significantly influence the onset and severity of symptoms. Being aware of these risk factors can help individuals anticipate potential symptoms and seek earlier intervention for lupus.
How can lupus symptoms affect daily life?
The symptoms of lupus, such as fatigue, joint pain, and skin rashes, can have a profound impact on daily activities and quality of life. Patients may find themselves unable to perform routine tasks or engage in social activities during flare-ups. Effective symptom management is crucial to maintaining a good quality of life for individuals with lupus.
Can lupus symptoms lead to diagnosis delays?
Yes, lupus symptoms can often lead to diagnosis delays because they are frequently vague and may resemble other conditions. Common symptoms like joint pain, fatigue, and skin rashes can be misattributed to other illnesses, making it essential for patients to communicate their experiences clearly with healthcare providers for appropriate lupus diagnosis.
What treatments are available to manage lupus symptoms?
While there is no cure for lupus, treatments focus on managing symptoms and controlling the immune system. Commonly prescribed medications include hydroxychloroquine for mild symptoms and stronger immunosuppressants for more severe cases. New targeted therapies are also emerging that specifically address the faulty immune responses in lupus, promising fewer side effects for patients.
| Symptom | Description | Additional Notes |
|---|---|---|
| Joint Pain | Pain from red, hot, swollen joints | Common symptom often overlooked as simple overuse or injury. |
| Rashes | Butterfly rash across cheeks and nose; discoid rash on skin | Can be mistaken for other skin conditions like rosacea. |
| Fatigue | Persistent tiredness | Vague and often can occur in individuals without lupus. |
| Hair Loss | Loss of hair in patches or thinning | Not always directly linked to lupus. |
| Raynaud’s Syndrome | Fingers or toes change color in cold temperatures | Can occur in people without lupus. |
Summary
Lupus symptoms are often subtle and can lead to delayed diagnoses, making awareness crucial. Early detection is key to managing this chronic autoimmune disease effectively. Due to the complexity and variety of symptoms like joint pain, rashes, fatigue, and hair loss, patients often face challenges in receiving timely treatment. Understanding these symptoms and taking proactive measures can significantly improve the quality of life for those affected by lupus.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.