Leishmania tropica, a parasite responsible for cutaneous leishmaniasis, is stirring concern among public health officials due to its rising prevalence in the Somali region of Ethiopia. This area, previously shielded from significant cutaneous leishmaniasis outbreaks, is now facing alarming cases as a result of migration and environmental changes. Genome sequencing of L. tropica has revealed unique variants, raising questions about drug resistance and the future management of this disease. The current situation calls for immediate genomic surveillance, which can identify the genetic signatures of this pathogen and inform effective treatment strategies. Additionally, the alarming rise of L. tropica highlights the pressing need to address public health challenges as they emerge in regions vulnerable to leishmaniasis.
The protozoan Leishmania tropica is increasingly recognized as a critical agent in the spread of skin infections known as cutaneous leishmaniasis. This parasite has taken center stage amid an outbreak in Ethiopia’s Somali region, an area where prior incidences of the disease were rare. As genomic studies uncover novel genetic variations within L. tropica, the implications for drug resistance and public health protocols become increasingly urgent. The evolution of this parasite underscores the need for enhanced genomic surveillance methods to track its spread and better understand its transmission dynamics. Furthermore, the resurgence of leishmaniasis in this region could signal a broader shift in disease patterns within East Africa, necessitating regional cooperation to combat this neglected tropical disease.
Understanding Leishmania tropica and Its Role in Cutaneous Leishmaniasis
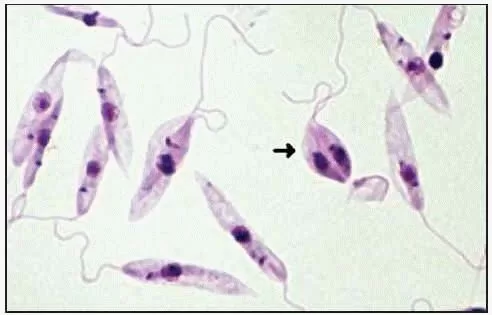
Leishmania tropica is a significant protozoan parasite responsible for one of the forms of cutaneous leishmaniasis (CL), a disease that manifests in various degrees of severity ranging from localized skin lesions to more extensive skin involvement. This parasite has distinct genomic properties that enable it to thrive in specific environments, especially in regions like the Somali area of Ethiopia. The current genomic characterization provided by recent studies reveals a unique variant of L. tropica that is closely associated with outbreaks of cutaneous leishmaniasis, further emphasizing the importance of understanding its transmission dynamics.
The presence of L. tropica in Ethiopia is particularly concerning due to the fact that the area was previously free of recorded CL cases. Biological and environmental factors, such as human migration and changes in land use due to conflicts, play a critical role in the emergence and spread of this pathogen. Furthermore, the potential for drug resistance, especially to treatments like antimony, highlights the need for effective genomic surveillance and innovative public health strategies to combat the spread of Leishmania infections.
Genomic Surveillance and Its Importance in Leishmaniasis Outbreaks
Genomic surveillance has emerged as a powerful tool in the management and understanding of infectious diseases, including leishmaniasis. By sequencing the genomes of pathogens from different geographical locations, researchers can track mutations and genetic variations that are indicative of drug resistance and transmission patterns. For instance, the 2023 findings of drug-resistant L. tropica variants in the Somali region underline the urgent requirement for advanced genomic surveillance systems in Ethiopia, which could drastically improve public health responses and treatment protocols.
Through whole-genome sequencing (WGS) technology, researchers can identify genetic markers related to virulence and resistance, which are crucial for developing targeted interventions against outbreaks of cutaneous leishmaniasis. In countries like Ethiopia, where the leishmaniasis epidemiological landscape is complex and influenced by various factors, genomic surveillance can provide insights that go beyond what traditional methods can offer. It can help in crafting robust public health strategies to contain and prevent outbreaks, particularly in regions where human and animal populations may intermix.
The Emergence of Cutaneous Leishmaniasis in the Somali Region
The recent outbreak of cutaneous leishmaniasis in the Somali region of Ethiopia serves as a wake-up call regarding the evolving nature of vector-borne diseases. Prior to this outbreak, the area had limited history of reported CL cases, illustrating how quickly the epidemiological landscape can change in response to factors like population displacement and environmental shifts. The emergence of cases with atypical clinical presentations, such as multiple wet lesions, points to the potential for new strains or variants of L. tropica to exploit both human and ecological changes.
Moreover, the Somali region’s unique environmental and socio-economic factors amplify the complications of managing emerging infectious diseases. Factors like inadequate healthcare infrastructure, coupled with the potential role of animal reservoirs in the leishmaniasis lifecycle, necessitate new strategies and collaborations between public health officials, researchers, and local communities to effectively control CL outbreaks. A holistic approach that considers genomic data along with epidemiological evidence will be essential in devising successful interventions.
Factors Contributing to Leishmania Dissemination in Ethiopia
Various factors contribute to the spread and persistence of leishmaniasis in Ethiopia, particularly in its complex socio-political landscape. Human migration due to factors such as famine and conflict can introduce L. tropica and other Leishmania species into new areas. This movement not only increases the potential for outbreaks but also complicates prevention and treatment efforts. Understanding the dynamics of human populations in relation to leishmaniasis transmission is vital for mitigating its spread.
Additionally, environmental changes, such as alterations in agricultural land use and urbanization, can create favorable conditions for sandflies, the primary vectors of leishmaniasis. Areas with high rates of deforestation or irrigation initiatives may inadvertently support the proliferation of these vectors. Consequently, public health strategies must consider these environmental factors and incorporate interdisciplinary approaches that combine public health, environmental management, and genomic surveillance to mitigate outbreaks effectively.
Clinical Victims: The Presentation of Cutaneous Leishmaniasis
In the context of the Somali region outbreak, patients presented with multiple wet lesions, differing from the typical single dry lesions observed in most Ethiopian cases. This clinical variation underscores the importance of tailored clinical approaches when dealing with leishmaniasis. Factors such as genetic susceptibility, immune response, and environmental influences could contribute to these diverse manifestations and must be considered when diagnosing and treating affected individuals.
Furthermore, the emergence of atypical presentations also highlights the need for enhanced clinical surveillance and the development of comprehensive guidelines for managing leishmaniasis in Ethiopia. Public health officials and healthcare providers should be equipped with training and resources to recognize these unique clinical features, facilitating timely diagnosis and treatment to prevent further spread among vulnerable populations.
Leveraging Genomic Data for Drug Resistance in Leishmania
One of the most critical insights from the 2023 genomic characterization study is the identification of specific mutations linked to drug resistance in L. tropica samples from the Somali region. Understanding these genetic markers is vital for the development of effective treatment options and for deploying appropriate drug regimens in the context of rising resistance. It is essential for health authorities to adopt genomic data into their therapeutic strategies to manage both current and future outbreaks efficiently.
This genomic data not only provides a snapshot of the current state of L. tropica in Ethiopia but also offers a template for evaluating the effectiveness of existing treatment protocols. By continuously monitoring genetic shifts in leishmaniasis pathogens, public health initiatives can better predict treatment failures and adapt management strategies accordingly, thereby enhancing patient outcomes and curtailing the progression of drug-resistant strains.
Public Health Strategies for Combatting Leishmaniasis
With the emergence of cutaneous leishmaniasis in the Somali region, public health strategies must evolve to address the diverse and complex nature of leishmaniasis transmission. Education and awareness programs aimed at local communities are crucial in empowering them to recognize symptoms and seek early treatment. This community-based approach can help reduce transmission rates and enhance the effectiveness of public health interventions.
Additionally, integrating genomic surveillance into existing public health frameworks can significantly improve the preparedness and response to leishmaniasis outbreaks. By utilizing genomic data to inform disease management practices, public health officials in Ethiopia can adopt a proactive stance, mitigating risks associated with the spread of L. tropica and enhancing overall health outcomes in affected regions.
Cross-Border Collaboration in Leishmaniasis Control
Given the transnational nature of leishmaniasis, particularly with the recent reports of L. tropica variants in the surrounding regions, cross-border collaboration among countries is essential. Collaborative efforts among Ethiopia, Kenya, and other neighboring nations can facilitate the sharing of surveillance data and best practices for managing leishmaniasis outbreaks. Such cooperation is particularly important in regions where human and animal populations frequently cross borders, creating potential hotspots for disease transmission.
Establishing joint research initiatives and collaborative public health campaigns can significantly increase the efficacy of interventions aimed at controlling leishmaniasis. It is vital for governments to recognize the importance of regional partnerships, harnessing shared knowledge and resources to combat the challenges posed by leishmaniasis in this ecologically and epidemiologically diverse area.
Research Directions for Future Leishmaniasis Studies
As the landscape of leishmaniasis continues to evolve, further research is essential for enhancing understanding and management of the disease. Key areas for exploration include the investigation of L. tropica’s genetic diversity, transmission dynamics, and resistance mechanisms. Such research efforts can provide valuable insights into the mechanisms behind the emergence of new variants and their implications for treatment efficacy.
Moreover, studies focusing on the socio-ecological factors influencing leishmaniasis outbreaks will be crucial in designing effective prevention programs. Collaborating with local communities and stakeholders can facilitate participatory research approaches that incorporate local knowledge and needs, ultimately leading to more effective strategies for managing and controlling leishmaniasis and its impact on public health in Ethiopia.
Frequently Asked Questions
What is Leishmania tropica and its role in cutaneous leishmaniasis in Ethiopia?
Leishmania tropica is a protozoan parasite responsible for cutaneous leishmaniasis (CL), particularly observed in the Somali region of Ethiopia. This variant has been linked to a recent outbreak characterized by unique genomic features and potential drug resistance, highlighting its significance in public health.
How is genomic surveillance used to combat Leishmania tropica outbreaks in the Somali Region?
Genomic surveillance plays a vital role in monitoring Leishmania tropica outbreaks by sequencing its genomes to identify mutations associated with drug resistance. This data helps public health officials implement timely interventions to control the spread of cutaneous leishmaniasis in Ethiopia and beyond.
What are the implications of drug resistance in Leishmania tropica for treatment of cutaneous leishmaniasis?
The identification of drug resistance mutations in Leishmania tropica poses significant challenges for treating cutaneous leishmaniasis (CL). Understanding these resistance patterns is crucial for developing effective treatment protocols and ensuring that patients receive appropriate care.
Why has Leishmania tropica gained attention in the context of emerging cutaneous leishmaniasis in Ethiopia?
Leishmania tropica has gained attention due to a recent outbreak of cutaneous leishmaniasis in the Kenyan border region of the Somali Region in Ethiopia, where it has emerged as a significant health concern. The genomic characteristics of the identified strains indicate a need for focused public health efforts.
What distinguishes Leishmania tropica from other species of Leishmania found in Ethiopia?
Leishmania tropica is distinct from other species like L. donovani and L. aethiopica primarily in terms of its clinical manifestations and genetic profile. The recent outbreak in Ethiopia revealed a genetically homogeneous variant of L. tropica not previously encountered, marking it as a variant of concern.
How does environmental change influence the epidemiology of Leishmania tropica in Ethiopia?
Environmental changes, such as human displacement and alterations in habitat, significantly impact the epidemiology of Leishmania tropica. These factors can facilitate the transmission of cutaneous leishmaniasis by affecting host and vector dynamics, especially in regions like the Somali region of Ethiopia.
What are the clinical manifestations of cutaneous leishmaniasis caused by Leishmania tropica?
Cutaneous leishmaniasis caused by Leishmania tropica typically presents with multiple wet lesions, contrasting with the more common single dry lesions seen with other Leishmania species in Ethiopia. This difference is crucial for clinical recognition and response to outbreaks.
What measures are recommended to mitigate the spread of Leishmania tropica in Ethiopia?
To mitigate the spread of Leishmania tropica, public health officials are urged to enhance genomic surveillance across humans and vectors, deploy effective diagnostic tools, and implement community awareness programs, particularly in regions experiencing outbreaks of cutaneous leishmaniasis.
What genomic findings were reported for Leishmania tropica in the recent Ethiopian outbreak?
In the recent outbreak of cutaneous leishmaniasis in the Somali region, genomic analyses indicated that the Leishmania tropica variants exhibit significant genetic homogeneity and unique mutations linked to drug resistance, suggesting a specific adaptation to the region.
What role does host and vector dynamics play in the transmission of Leishmania tropica?
The dynamics of hosts and vectors are crucial in the transmission of Leishmania tropica, as the interaction between environmental changes, human migration, and the presence of vectors can facilitate outbreaks of cutaneous leishmaniasis in previously unaffected areas.
| Key Point | Details |
|---|---|
| Genomic Sequencing | Eight genomes of Leishmania tropica were sequenced from cutaneous leishmaniasis samples in Ethiopia. |
| Drug Resistance | A variant with unique genomic signatures indicating drug resistance to antimony was identified. |
| Recent Outbreak | An outbreak was detected among recently deployed militia, marking a change in chronic exposure. |
| Geographical Focus | The focus of leishmaniasis has shifted to East Africa, specifically Ethiopia, after the success of kala-azar elimination in the Indian subcontinent. |
| Clinical Forms | Leishmaniasis features various clinical forms: Visceral (VL) and three types of cutaneous leishmaniasis: localized, diffuse, and muco-cutaneous. |
Summary
Leishmania tropica plays a critical role in the current landscape of cutaneous leishmaniasis outbreaks, especially in Ethiopia. Recent genomic studies have revealed significant insights, particularly regarding the unique drug-resistant variants of L. tropica that have emerged in the Somali region. As the epidemiological landscape shifts due to environmental changes and human migrations, continuous genomic surveillance is essential to effectively manage and mitigate the impacts of this disease.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.