The intricate relationship between gut microbiota and viral respiratory infections reveals a fascinating aspect of infant health. Recent research indicates that the right mix of gut bacteria may be crucial for preventing severe viral lower respiratory tract infections (vLRTIs) in infants. These beneficial gut bacteria, particularly in those born vaginally, play an essential role in shaping the early-life microbiome, which directly influences immunity. Studies have found that a diverse microbiome during the first weeks of life is associated with lower hospitalization rates for vLRTI, highlighting the importance of infant gut bacteria. Thus, understanding the microbiome and immunity could lead to innovative strategies for vLRTI prevention and improved health outcomes for infants.
Exploring the connection between the microbial landscape in the gastrointestinal tract and respiratory viral infections opens a new frontier in pediatric health. Emerging evidence suggests that the composition of gut flora, especially in newborns, significantly impacts their resilience against severe respiratory illnesses. With a focus on early-life microbiome development, researchers are uncovering how specific strains of beneficial bacteria can bolster the immune response, particularly in infants during vulnerable stages. This insight paves the way for potential interventions, such as tailored probiotics, that may enhance vLRTI defense in young children. As science delves deeper into the gut-lung axis, the potential for revolutionary changes in infant health care becomes increasingly apparent.
Understanding the Role of Gut Microbiota in Infant Health
The gut microbiota, a complex community of microorganisms residing in the intestines, plays a pivotal role in the overall health and development of infants. Particularly, studies indicate that the right mix of gut bacteria can significantly shape immune responses, and this influence begins right from birth. Research highlights that infants delivered vaginally tend to have a richer diversity of beneficial gut bacteria, which is closely associated with a stronger immune system capable of combating various infections. Early exposure to a diverse microbiome is crucial for setting the stage for lifelong health, potentially protecting against conditions such as viral lower respiratory tract infections (vLRTIs).
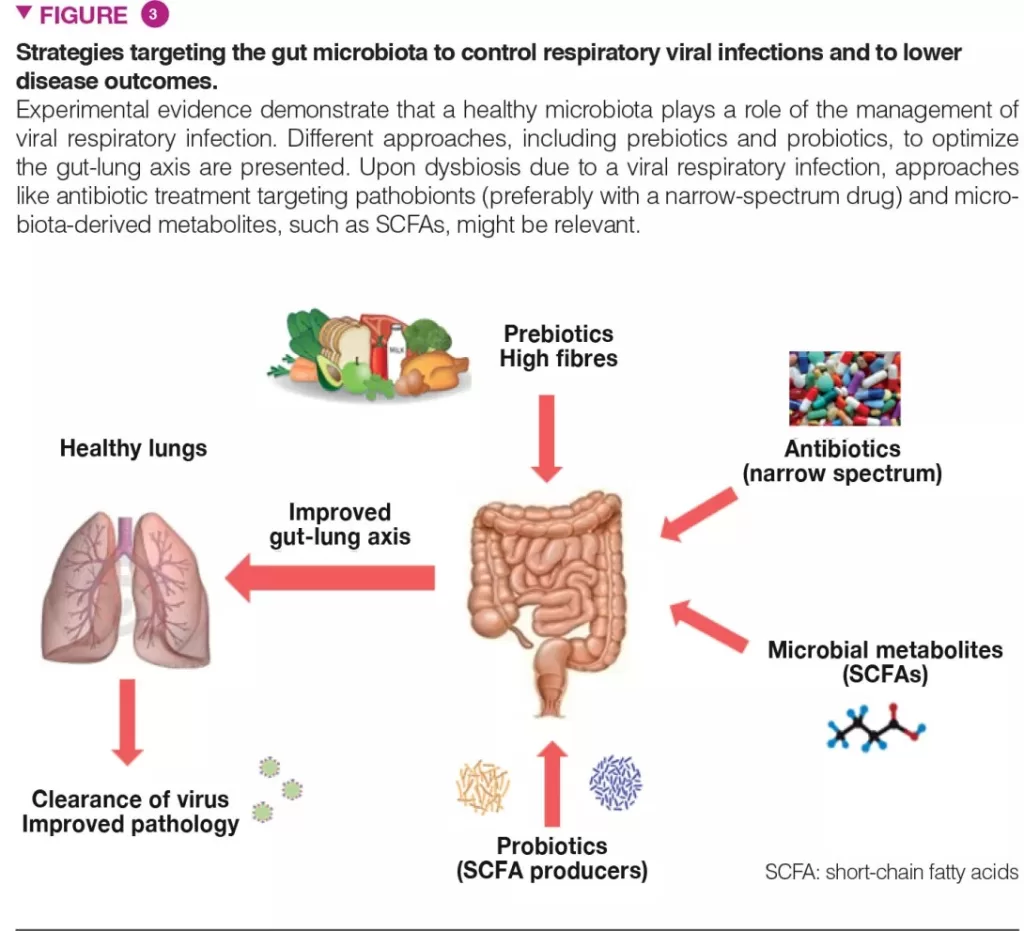
Furthermore, establishing a healthy balance of gut bacteria early in life not only aids in the development of the immune system but also fosters a robust gut–lung axis. This connection signifies how gut health directly influences respiratory functions. Infants with less microbial diversity might experience compromised immunity, increasing their vulnerability to respiratory infections. Hence, early-life microbiome development is an essential factor that deserves attention, particularly when considering preventive strategies for vLRTI in infants.
Viral Lower Respiratory Tract Infections and Gut Health
Viral lower respiratory tract infections (vLRTIs) pose significant health risks to infants, leading to hospitalizations which can be distressing for families. The emerging evidence suggests that the composition of an infant’s gut microbiota can have a preventive role against these infections. For instance, the study indicates that infants with a higher diversity of gut bacteria during the first week of life enjoy lower rates of hospitalization due to vLRTI. This suggests that fostering beneficial gut bacteria could be a key strategy in enhancing immunity and reducing the incidence of respiratory-related illnesses.
Moreover, specific strains of gut bacteria, such as *Bifidobacterium breve* and *Bifidobacterium longum*, have been highlighted as particularly beneficial for infant health. The presence of these bacteria is linked with expansive health benefits, suggesting that personalized interventions, like targeted probiotics, could serve to optimize the early-life microbiome. Such advancements could be critical in pediatric medicine, offering new avenues for vLRTI prevention through microbiota modulation.
The Importance of Early-Life Microbiome Development
The early-life microbiome sets the foundation for lifelong health, influencing everything from metabolic processes to immune system development. During the initial weeks and months after birth, infants are particularly susceptible to various health issues, making the establishment of a healthy gut microbiota crucial. The research underscores how newborns born vaginally possess a distinctive microbiome that is conducive to better health outcomes. The interconnectedness of the gut microbiome with the immune system highlights the importance of cultivating beneficial gut bacteria during infancy.
Understanding the dynamics of early-life microbiome development allows for the identification of critical factors that influence health. For instance, exposure to a diverse microbial environment during birth could play a significant role in bolstering the infant’s immune defenses against viral infections. This research opens up possibilities for interventions aimed at promoting a healthy microbiome during the first stages of life, potentially paving the way for innovative probiotic therapies that can further enhance infant health.
Identifying Beneficial Gut Bacteria for Infants
Identifying specific strains of beneficial gut bacteria can significantly impact infant health and development. Recent studies emphasize that strains like *Bifidobacterium longum* and *Bifidobacterium breve* not only enrich the gut microbiome but also enhance immunity in infants. These beneficial bacteria play vital roles in protecting against infections by enhancing the overall function of the immune system. The presence of such bacteria could be a deciding factor in determining how infants respond to pathogens, including those that cause vLRTIs.
Furthermore, the identification of these beneficial strains lends itself to future research and development aimed at creating targeted synbiotics and probiotics. Tailoring infant nutrition to include these beneficial gut bacteria could potentially reduce the risk of serious infections and illnesses. By focusing on the enhancement of the infant gut bacteria diversity early on, healthcare practitioners could devise nutritional plans that fortify the infant’s immune system, ultimately leading to better health outcomes.
The Gut-Lung Axis: A Connection Worth Exploring
The gut-lung axis is a fascinating area of research that elaborates on how gut health influences lung immunity. Recent findings suggest that a diverse gut microbiome can lead to better respiratory health outcomes in infants, particularly in the context of viral infections. As the body of evidence grows, it becomes increasingly clear that the interplay between gut bacteria and respiratory health could be vital for developing effective strategies against respiratory diseases like vLRTIs.
This connection highlights the potential benefits of focusing on gut health as a preventive strategy for respiratory illnesses. Thus, improving the diversity of beneficial gut bacteria in infants through diet, probiotics, or maternal health during pregnancy could enhance immune responses in the lungs. Understanding this link offers a multi-faceted approach to infant health, combining dietary interventions with a broader understanding of how gut microbiota directly influences respiratory immunity.
Hospitalization Rates and Microbiota Diversity
Hospitalization due to viral lower respiratory tract infections (vLRTIs) is a serious concern for families with infants, and recent studies shed light on the importance of gut microbiota diversity in this context. The research indicates that higher diversity in gut bacteria during the critical first week of life is associated with significantly lower hospitalization rates for respiratory infections. This direct correlation underscores the need to understand and promote the factors that contribute to a healthy microbiome in early infancy.
In particular, infants that harbor a diverse array of gut bacteria show enhanced resistance to infections, which may suggest that interventions designed to increase microbiota diversity could substantially reduce the rates of hospitalization due to vLRTI. By prioritizing understanding of gut bacteria development early on, healthcare providers can better equip new parents with strategies to enhance their child’s gut health, potentially lowering the overall incidence of respiratory complications.
The Future of Probiotics in Infant Health
The future of probiotics in infant health is a promising avenue for exploration, particularly regarding their role in optimizing gut microbiota for immune support. As research continues to unveil the importance of specific beneficial gut bacteria, there is significant potential for developing targeted probiotics that cater specifically to infants’ needs. Given that certain strains have demonstrated the ability to bolster immunity, especially in the context of vLRTIs, optimizing infant nutrition with these products could be revolutionary.
The Baby Biome Study suggests that different microbiota compositions can lead to varied health outcomes, making the case for a more tailored approach to probiotics. Future probiotic formulations might include strains like *Bifidobacterium longum*, customizing them to deliver the maximum health benefits. As we enhance our understanding of the intricate relationship between gut microbiota and immunity, we can leverage this knowledge to implement preventive strategies that safeguard infants against respiratory infections.
Maternal Influence on Infant Gut Microbiota
Maternal health and diet are critical factors influencing the development of an infant’s gut microbiota. The composition of the microbiome that an infant inherits during childbirth can be substantially different based on whether the delivery occurred vaginally or via cesarean section. Mothers who maintain a healthy diet rich in probiotics can positively impact their baby’s gut microbiome, potentially reducing the infant’s risk of respiratory infections and promoting general health.
Moreover, the maternal microbiome during pregnancy may play an integral role in shaping the infant’s microbiota. Research suggests that maternal factors, including nutrition, antibiotic use, and overall health, can have lasting impacts on the infant gut’s bacterial composition. Understanding this maternal influence presents an opportunity for educational interventions aimed at guiding new mothers toward lifestyles that promote the establishment of a beneficial gut microbiota in their newborns.
The Importance of Environmental Factors in Microbiome Development
Environmental factors significantly influence the development of the infant gut microbiome. Elements such as exposure to pets, siblings, and different types of diets can shape the microbial diversity that infants experience during their formative months. Research indicates that a more diverse environment might lead to a more resilient microbiome, thus potentially offering improved defense against vLRTIs and other infections.
Additionally, external factors like antibiotic exposure during early life can disrupt microbiota development, leading to less diversity and increased susceptibility to respiratory infections. Ensuring that infants are exposed to a wide range of environmental microbes and limiting unnecessary antibiotic use can help foster a healthier gut microbiota. As awareness of these influences grows, there is potential for family-oriented interventions that support optimal microbiome development.
Frequently Asked Questions
How does gut microbiota impact viral respiratory infections in infants?
Research indicates that the composition of gut microbiota, particularly in infants, plays a crucial role in immune system development. This affects the lung immune response and may help prevent severe viral lower respiratory tract infections (vLRTIs) during early life.
What is the significance of beneficial gut bacteria in preventing vLRTIs?
Beneficial gut bacteria, such as *Bifidobacterium breve* and *Bifidobacterium longum*, contribute to a healthy gut microbiota. These bacteria are associated with lower hospitalization rates for vLRTIs, highlighting the importance of a diverse microbiome in infants’ early life.
Can the early-life microbiome influence the risk of hospitalization for viral respiratory infections?
Yes, studies show that higher diversity in the early-life microbiome correlates with reduced hospitalization rates for vLRTIs. Infants with a healthier microbiota are better equipped to resist severe respiratory infections.
What factors may affect the development of gut microbiota in infants?
Delivery method significantly influences gut microbiota composition, with vaginally born infants typically exhibiting more beneficial gut bacteria compared to those born via cesarean section. Other factors include diet, environment, and antibiotic exposure.
Is there a potential for developing probiotics targeting early-life gut microbiota?
Yes, understanding the specific strains of infant gut bacteria that confer health benefits could lead to targeted probiotics that support early microbiome development and improve immune responses against viral respiratory infections.
What outcomes have been observed in infants with diverse gut microbiota in relation to viral infections?
Infants displaying greater gut microbiota diversity in their first week of life have shown significantly lower rates of hospitalization for viral lower respiratory tract infections, indicating that microbial diversity is protective.
How can parents promote a healthy gut microbiome in infants?
To promote a healthy gut microbiome, parents can encourage breastfeeding, maintain a clean environment, and consult healthcare providers regarding the safe use of antibiotics, as these practices promote the growth of beneficial gut bacteria.
| Key Points |
|---|
| The right mix of gut microbiota can prevent hospitalization for viral respiratory infections in infants. |
| Infants born vaginally have more beneficial gut microbiota than those born via cesarean section. |
| Higher gut microbiota diversity is linked to lower hospitalization rates for viral lower respiratory tract infections (vLRTIs). |
| The study identified three microbiota clusters; Cluster 3 is the most beneficial and is found only in vaginally born infants. |
| Understanding infant gut bacteria can lead to the development of targeted probiotics to promote healthy microbiome development. |
Summary
Gut microbiota and viral respiratory infections are intricately linked, as research indicates that the right combination of gut bacteria can significantly reduce the risk of hospitalization due to viral lower respiratory tract infections in infants. Specifically, infants who are delivered vaginally tend to have a more beneficial gut microbiota composition, which is associated with improved immune responses. This research highlights the importance of microbiota diversity in early life and its potential role in preventing serious respiratory infections. By understanding these microbial benefits, it may be possible to develop targeted probiotics that support infant health during critical developmental stages.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.