Gonorrhea ceftriaxone resistance is swiftly becoming a pressing public health issue, particularly highlighted by alarming findings in Cambodia. Recent studies reveal a concerning rise in ceftriaxone-resistant strains of Neisseria gonorrhoeae, alongside a threefold increase in extensively drug-resistant gonorrhea (XDR). As researchers from Cambodia’s National Center for HIV/AIDS and the World Health Organization (WHO) detail, nearly one-third of isolates tested showed elevated minimum inhibitory concentrations (MICs) for ceftriaxone, blurring the lines of effective gonorrhea treatment. This ongoing epidemic of gonorrhea resistance signals a significant threat, emphasizing the necessity for urgent action against antimicrobial resistance in Cambodia and beyond. As the situation evolves, the implications for public health and treatment strategies are profound, requiring immediate attention from both clinicians and researchers alike.
The emergence of ceftriaxone-resistant gonorrhea poses a substantial challenge to controlling sexually transmitted infections globally. This increase in antimicrobial resistance, particularly evident in regions like Cambodia, suggests that traditional treatment options are becoming less effective against the Neisseria gonorrhoeae bacterium. Recent findings indicate that not only are standard therapies failing, but also that extensively drug-resistant (XDR) variants are spreading at alarming rates. With a significant portion of isolates exhibiting high resistance profiles to essential antimicrobials, including ceftriaxone and azithromycin, the need for enhanced surveillance and innovative treatment approaches has never been more pressing. Tackling gonorrhea resistance will require a concerted effort to monitor and combat its spread to protect public health effectively.
The Growing Concern of Ceftriaxone Resistance in Gonorrhea
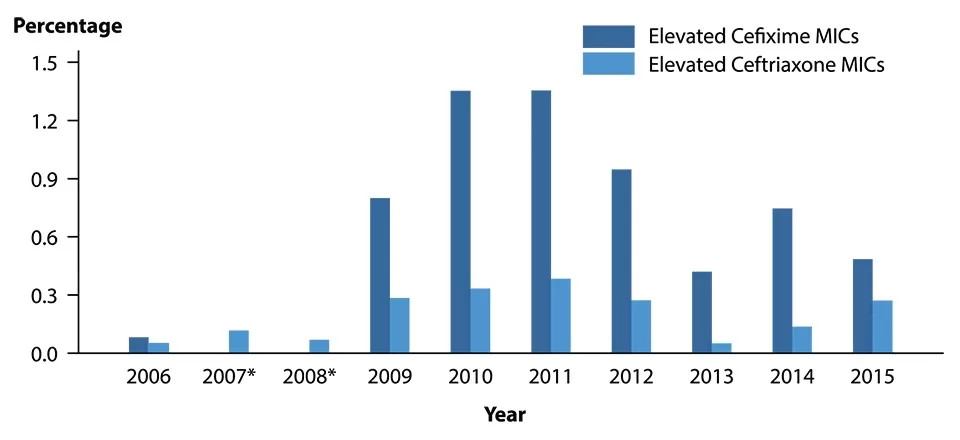
Recent analyses have shown a troubling trend in the rise of ceftriaxone-resistant strains of Neisseria gonorrhoeae in Cambodia. The study reported a significant proportion of isolates exhibiting resistance to ceftriaxone, a cornerstone of gonorrhea treatment. Specifically, researchers detected that 31% of the gonorrhea samples from 2023 showed minimum inhibitory concentrations (MICs) indicative of resistance. This alarming statistic highlights the continuing challenge of managing gonorrhea effectively, particularly as resistance patterns evolve.
The implications of ceftriaxone resistance are dire, not just for individual health outcomes but also for public health strategies aimed at controlling sexually transmitted infections (STIs). As gonorrhea increasingly demonstrates antimicrobial resistance, traditional treatments may become obsolete, forcing healthcare providers to seek alternative therapies, often at higher costs and with uncertain efficacy. The findings from this research reiterate the necessity for robust public health initiatives to monitor and combat the rise of drug-resistant gonorrhea.
Understanding Extensively Drug-Resistant (XDR) Gonorrhea
Extensively drug-resistant (XDR) gonorrhea presents a critical challenge within the framework of gonorrhea treatment. In the recent study, 12.5% of the isolates were classified as XDR, indicating resistance not only to ceftriaxone but also to azithromycin, another key treatment option. This escalation from 4% in the previous year denotes a worrying trend, as XDR phenotypes make standard treatment regimens ineffective and place patients at greater risk for complications stemming from untreated infections.
The increased prevalence of XDR gonorrhea mirrors global trends in antimicrobial resistance and underscores an urgent need for enhanced surveillance and rapid response mechanisms. As health authorities grapple with this emerging threat, there is a pressing call for comprehensive strategies that integrate genomic surveillance and establish treatment guidelines that can adapt to evolving resistance patterns. Without immediate action, XDR gonorrhea could significantly impede efforts to control STIs.
Antimicrobial Resistance Patterns in Cambodia
Research conducted as part of the WHO’s Enhanced Gonococcal Antimicrobial Surveillance Program (EGASP) has brought to light the disturbing patterns of antimicrobial resistance in Cambodia. The genomic analysis of isolates revealed that a considerable number carried the same resistance mutation, suggesting a common lineage of ceftriaxone-resistant strains. Such findings highlight a critical focus area for both local and international health authorities in the fight against gonorrhea, where tracking these mutations is essential for understanding and controlling resistance.
Moreover, the ongoing transmission of these resistant strains indicates a broader public health crisis that could extend beyond Cambodia, particularly in the Asia-Pacific region. Reports of similar resistance patterns in neighboring countries amplify concerns and illustrate the need for a coordinated regional approach to tackle gonorrhea and its accompanying resistance issues. Understanding the local dynamics of antimicrobial resistance is paramount to designing effective interventions and treatment protocols.
The Impact of Antimicrobial Resistance on Gonorrhea Treatment
Antimicrobial resistance significantly complicates the treatment of gonorrhea, leading to increased rates of treatment failures and recurrent infections. As ceftriaxone resistance becomes more prevalent, healthcare providers are increasingly challenged to find effective alternatives when treating gonorrheal infections. The emergence of resistant strains limits treatment options and may lead to longer-term health complications for affected individuals due to the inability to manage the infection effectively.
Additionally, the diversity of resistance mechanisms observed in gonorrhea suggests an urgent need for ongoing research and development of new antimicrobial agents. Clinical outcomes for patients with multidrug-resistant gonorrhea may be severely compromised, as conventional therapies become ineffective. Therefore, investing in novel treatments and improving existing antibiotics is essential to address the issue of gonorrhea treatment challenges posed by emerging resistance.
The Role of Public Health in Monitoring Gonorrhea Resistance
Public health plays a pivotal role in the ongoing monitoring of gonorrhea resistance patterns. Programs like the WHO’s Enhanced Gonococcal Antimicrobial Surveillance Program (EGASP) are crucial for tracking resistance trends and notifying health authorities about emerging threats. These data-driven initiatives allow for timely public health alerts and appropriate responses to outbreaks of resistant strains, thereby minimizing their impact on community health.
In Cambodia, the findings from recent studies highlight the necessity for integrated surveillance systems to capture real-time data on gonorrhea resistance. By leveraging extensive genomic and antimicrobial susceptibility testing, public health agencies can better understand how these resistant strains spread and evolve, ultimately informing targeted interventions. Effective public health strategies will require collaboration between local, regional, and global stakeholders to combat the escalating threat of gonorrhea resistance.
Global Implications of Antimicrobial Resistance in Gonorrhea
The global implications of antimicrobial resistance in gonorrhea extend far beyond local incidences, posing risks to public health across nations. Cambodian studies showcasing increasing resistance to first-line treatments like ceftriaxone and azithromycin reflect similar trends documented worldwide, highlighting an interconnected health crisis. As gonorrhea becomes increasingly untreatable, the ramifications could affect population health, healthcare costs, and social dynamics related to STIs.
This global concern necessitates a unified international response in addressing the problem of drug-resistant gonorrhea. Renaissance in research, development of new therapeutics, and improved surveillance systems can bridge the gap between current treatment failures and the urgent healthcare needs of affected populations. Collaborative efforts are essential to ensure that effective treatment options remain available to combat escalating gonorrhea resistance.
New Emerging Gonorrhea Strains and Their Resistance Mechanisms
The emergence of new strains of Neisseria gonorrhoeae with varying resistance mechanisms poses an ongoing challenge for the treatment of gonorrhea. Recent genomic analyses conducted in Cambodia have identified novel mutations in resistant isolates, suggesting a dynamic interplay of genetic factors contributing to ceftriaxone and azithromycin resistance. Understanding these intricacies is vital for the development of targeted interventions and tailored treatment approaches.
Furthermore, continued discovery of different resistance profiles across gonorrhea strains underlines the need for continuous genomic surveillance. Health authorities must remain vigilant in identifying and characterizing these emerging strains to adjust treatment protocols and public health responses swiftly. Failure to do so may lead to a harsher public health crisis, exacerbating the prevalence of resistant gonorrhea strains.
Ceftriaxone Resistance: A Challenge for Gonorrhea Control
Ceftriaxone resistance directly challenges existing gonorrhea control measures, necessitating urgent action from health authorities. Increased resistance rates among Neisseria gonorrhoeae isolates signal a shift in treatment efficacy. In this light, clinicians and public health officials must urgently explore new therapeutic interventions and enhance their approaches to managing these increasingly resistant infections.
Moreover, as studies indicate a growing number of cases resistant to both ceftriaxone and azithromycin, there is an escalating concern regarding public health strategies. Comprehensive frameworks that combine education, prevention, and treatment will be critical for reversing the trends in gonorrhea resistance. The situation is pressing, and immediate collaborative efforts are required to ensure that gonorrhea can be effectively treated in the future.
Future Directions in Gonorrhea Research and Treatment
The future of gonorrhea research must focus not only on understanding resistance mechanisms but also on developing innovative treatment protocols that can swiftly adapt to the evolving landscape of antimicrobial resistance. With the alarming rise of ceftriaxone-resistant and extensively drug-resistant (XDR) strains, research initiatives should prioritize novel therapeutic strategies that promise effective outcomes against resistant gonorrhea.
Furthermore, engaging in global collaboration and sharing research findings can accelerate the discovery of new treatment options. By establishing strong communication channels among researchers and health organizations, the global health community can create a structured and informed approach to tackle the growing challenge of gonorrhea resistance. Continuous investment in research is essential for safeguarding public health against these evolving bacterial threats.
Frequently Asked Questions
What is ceftriaxone resistance in gonorrhea and why is it concerning?
Ceftriaxone resistance in gonorrhea refers to the ability of Neisseria gonorrhoeae strains to survive treatment with ceftriaxone, a key antibiotic used to treat this sexually transmitted infection. This resistance is concerning because it limits treatment options and poses a threat to public health, as evidenced by a documented increase in ceftriaxone-resistant gonorrhea strains in Cambodia.
How prevalent is ceftriaxone resistant gonorrhea in Cambodia?
Recent studies indicate that approximately 31% of gonorrhea isolates in Cambodia display minimum inhibitory concentrations (MICs) for ceftriaxone that raise concerns about resistance. Alarmingly, there has been a noted increase in extensively drug-resistant (XDR) gonorrhea strains, with 12.5% of samples exhibiting resistance to both ceftriaxone and azithromycin.
What does the term XDR gonorrhea mean?
XDR gonorrhea, or extensively drug-resistant gonorrhea, refers to strains of Neisseria gonorrhoeae that show resistance to at least ceftriaxone and azithromycin. This type of resistance significantly hampers treatment effectiveness, highlighting a growing public health challenge as reported in recent studies in Cambodia.
What impact does antimicrobial resistance in Cambodia have on gonorrhea treatment?
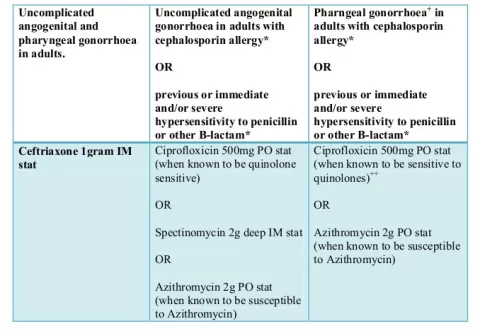
Antimicrobial resistance in Cambodia poses a serious challenge for gonorrhea treatment by leading to a decreased efficacy of first-line antibiotics, like ceftriaxone and cefixime. With rising rates of ceftriaxone resistance reported, it becomes increasingly crucial to monitor and adapt treatment strategies to combat the spread of resistant strains.
What are the signs of increased gonorrhea ceftriaxone resistance in studies?
Signs of increased gonorrhea ceftriaxone resistance include the detection of elevated minimum inhibitory concentrations (MICs) in gonorrhea isolates, as observed in studies where 31% of isolates in Cambodia showed resistance. The emergence of XDR strains, which notably increased from 4% to 12.5%, further indicates a troubling rise in resistance.
How can we address ceftriaxone resistant gonorrhea in public health strategies?
Addressing ceftriaxone resistant gonorrhea requires strengthened surveillance and monitoring of antimicrobial resistance patterns, enhanced public health alerts for resistance detection, and development of new treatment guidelines to effectively manage and control the spread of resistant strains, especially in high-risk regions like Cambodia.
Why is monitoring antimicrobial resistance in gonorrhea important for the Asia-Pacific region?
Monitoring antimicrobial resistance in gonorrhea is crucial for the Asia-Pacific region due to the increasing rates of resistance observed, such as in Cambodia and China. Early detection of resistance patterns is essential to inform treatment protocols and prevent widespread outbreaks of resistant gonorrhea strains.
What mutations are associated with ceftriaxone resistant gonorrhea?
A significant mutation associated with ceftriaxone resistant gonorrhea is the penA-60.001 allele. Studies have shown that this mutation is prevalent among resistant strains, highlighting the need for continuous genomic analysis to track emerging resistance mechanisms.
What actions are recommended in response to the rise of ceftriaxone resistance in gonorrhea?
In response to the rise of ceftriaxone resistance in gonorrhea, public health officials recommend enhancing surveillance programs, such as the WHO’s Enhanced Gonococcal Antimicrobial Surveillance Program, increasing awareness and education about gonorrhea treatment options, and encouraging regular testing and treatment for sexually transmitted infections.
| Key Points |
|---|
| Ongoing transmission of ceftriaxone-resistant strains found in Cambodia, indicating a serious public health threat. |
| A threefold increase in extensively drug-resistant (XDR) Neisseria gonorrhoeae strains was reported compared to previous years. |
| 22 out of 72 isolates (31%) showed minimum inhibitory concentrations (MICs) nearing resistance for ceftriaxone and cefixime. |
| 12.5% of isolates exhibited the XDR phenotype, representing a significant increase from 4% in 2022. |
| Genomic analysis revealed that most resistant strains share a specific mutation (penA-60.001 allele), complicating treatment options. |
| Emerging strains present a challenge as they cluster phylogenetically differently from previously documented resistant clones. |
| There is an urgent need for increased monitoring of antimicrobial resistance in gonococcal infections, particularly across the Asia-Pacific region. |
Summary
Gonorrhea ceftriaxone resistance remains a pressing issue in public health. Recent studies from Cambodia illustrate alarming trends in ceftriaxone-resistant Neisseria gonorrhoeae strains, with a notable rise in extensively drug-resistant (XDR) cases. The findings, based on antimicrobial susceptibility tests and genomic analysis, highlight that over 30% of isolates now show elevated resistance levels, prompting concerns about whether current treatment protocols will remain effective. These developments underline the critical need for enhanced surveillance and continued research to mitigate the risk of widespread gonorrhea resistance, especially in an interconnected global health landscape.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.