Energy metabolism disorders are at the core of many complex migraine conditions, intertwining with key factors like mitochondrial dysfunction and oxidative stress. Understanding these disorders reveals how disturbances in brain energy metabolism can trigger migraine episodes, influenced by common triggers such as stress, sleep deprivation, and even certain dietary habits. The link between insulin resistance and energy metabolism further complicates the clinical picture, as both are pivotal in determining the severity and frequency of migraines. Current research is delving into therapeutic repurposing strategies that aim to restore normal energy metabolism, providing hope for those affected by debilitating migraines. By addressing these underlying metabolic pathways, new interventions may finally offer effective relief for chronic migraine sufferers who have struggled with traditional treatments.
When we talk about metabolic disorders affecting energy utilization in the body, we often refer to conditions that disrupt normal mitochondrial function and contribute to oxidative stress, particularly in relation to migraines. These metabolic dysfunctions can manifest through various symptoms, often exacerbated by lifestyle factors such as inadequate sleep or high-stress levels. Approaching this issue from a broader perspective allows for a more comprehensive understanding of how nutrient deficiencies and insulin sensitivity play roles in the onset of migraines. Moreover, the exploration of alternative therapies focused on metabolic balance presents exciting possibilities for managing these neurological challenges. Such insights underscore the critical relationship between metabolic health and migraine management, opening pathways to new, innovative treatments.
Understanding Energy Metabolism Disorders in Migraine
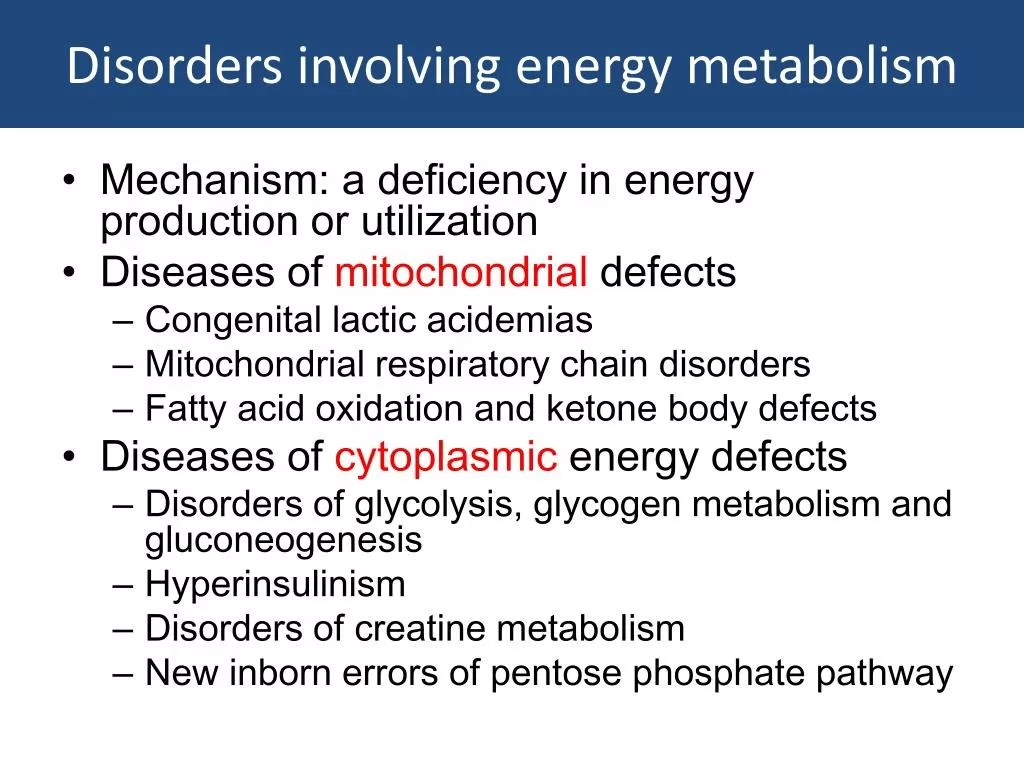
Energy metabolism disorders can play a significant role in the development and exacerbation of migraines. These disorders can disrupt the delicate balance of energy production in the brain, often resulting in a range of neurological symptoms including intense headaches. Factors such as mitochondrial dysfunction contribute to this imbalance, leading to insufficient energy supply for brain cells, which can trigger migraine episodes. Moreover, when energy metabolism is impaired, oxidative stress becomes a major concern, causing further cellular damage and inflammation in the brain.
In individuals suffering from migraines, understanding the pathways through which energy metabolism is affected is essential. Insulin resistance is a common metabolic dysregulation linked to migraines, exacerbating energy deficits and increasing oxidative stress. As such, recognizing how these disorders manifest can help inform better treatment strategies aimed at restoring normal energy metabolism and potentially reducing migraine frequency and severity.
Exploring Migraine Triggers and Their Links to Energy Metabolism
Migraine triggers are often multifaceted, involving both intrinsic and extrinsic factors that disrupt brain energy metabolism. Stress, sleep deprivation, and fasting are significant triggers that can lead to increased oxidative stress and mitochondrial dysfunction. Because these conditions can hinder the brain’s ability to generate energy efficiently, they may heighten an individual’s susceptibility to migraines. By identifying and managing these triggers, patients may find relief from their symptoms and improve their overall energy metabolism.
Understanding the interplay between migraine triggers and energy metabolism is essential for both prevention and management strategies. For instance, dietary interventions that improve insulin sensitivity may aid in stabilizing energy levels in the brain, thus mitigating the risk of migraines. Therapeutic approaches that focus on enhancing mitochondrial function may also prove beneficial by addressing the underlying metabolic disturbances that exacerbate this condition.
The Role of Mitochondrial Dysfunction in Migraine Pathogenesis
Mitochondrial dysfunction is recognized as a crucial factor in the pathogenesis of migraines. It significantly impacts brain energy metabolism, contributing to both energy deficits and increased oxidative stress. Impaired mitochondrial function can lead to decreased ATP production, essential for proper neuronal function and signaling. Consequently, this can trigger cortical spreading depression—a wave of electrical activity linked to migraine attacks—thus highlighting the critical role that these organelles play in migraine susceptibility.
In addressing mitochondrial dysfunction as a component of migraine management, researchers are exploring therapeutic repurposing strategies. Medications that can enhance mitochondrial function are being evaluated for their efficacy in reducing migraine incidences. By restoring mitochondrial health, it may be possible to alleviate the oxidative stress and energy deficits that contribute to migraine pathophysiology, representing a promising area for future research and intervention.
Oxidative Stress and Its Implications for Migraine Sufferers
Oxidative stress is a significant contributor to the overall pathology of migraines. The imbalance between reactive oxygen species (ROS) and antioxidants in the brain can lead to neuronal damage and inflammation, which are often correlated with migraine attacks. Elevated levels of oxidative stress can exacerbate symptoms and increase the frequency of migraine episodes by further disrupting energy metabolism. Addressing oxidative stress is, therefore, a key component in developing effective migraine treatment strategies.
Interventions aimed at enhancing the body’s antioxidant defenses may provide relief for those suffering from migraines. Nutrients that bolster these defenses can improve mitochondrial function and modulate energy metabolism, potentially reducing oxidative stress levels in the brain. Such therapeutic measures could prove to be beneficial, especially in conjunction with established migraine treatments, offering a holistic approach towards managing this debilitating condition.
Therapeutic Repurposing in the Management of Migraines
Therapeutic repurposing refers to the practice of finding new uses for existing medications, and it holds significant potential in migraine management. Given the role of energy metabolism in migraines, drugs that influence mitochondrial function or aid in reducing oxidative stress are being explored. The aim is to provide migraine sufferers with effective treatments that can address the underlying metabolic issues rather than just alleviating symptoms.
Research into the effects of medications originally developed for other conditions is ongoing, particularly in how they can impact energy metabolism disorders and assist those with migraines. By focusing on repurposing established drugs that already have a known safety profile, there is potential for quicker and more efficient paths to treatment options for patients who continue to suffer from migraines despite standard therapies.
Insulin Resistance: A Dual Role in Migraine and Energy Metabolism
Insulin resistance is a condition characterized by the body’s reduced ability to respond to insulin, and it has been linked to increased migraine susceptibility. This metabolic dysfunction can contribute to both increased energy metabolism disorders and heightened oxidative stress, creating a cycle that exacerbates migraine symptoms. Understanding this connection can be vital for developing integrated treatment approaches that address both energy metabolism and the metabolic aspects of migraine.
Targeting insulin resistance through dietary changes, exercise, and medications may help stabilize energy levels in the brain, potentially reducing migraine frequency. Incorporating strategies that improve insulin sensitivity can play a crucial role in the holistic management of migraines, aligning metabolic health with pain management and prevention strategies.
Nutritional Interventions to Improve Mitochondrial Function in Migraine
Nutritional interventions are gaining traction as an important aspect of managing energy metabolism disorders associated with migraines. Specific nutrients have been identified as beneficial for enhancing mitochondrial function, which is crucial in maintaining energy levels in the brain. For instance, coenzyme Q10 and certain B vitamins support cellular energy production and may help alleviate symptoms in migraine sufferers.
Furthermore, incorporating foods rich in omega-3 fatty acids and antioxidants can combat oxidative stress while supporting brain health. A balanced diet that addresses both energy metabolism and oxidative stress may significantly contribute to reducing the occurrence and severity of migraine episodes. Such dietary frameworks can be part of a comprehensive management strategy for individuals prone to migraines.
The Importance of Regular Exercise in Managing Migraines
Regular physical activity plays a vital role in managing migraines, particularly through its effects on energy metabolism and reducing oxidative stress. Exercise has been proven to improve insulin sensitivity and enhance mitochondrial function, aiding in the regulation of energy levels. Engaging in consistent exercise routines can lead to significant improvements in overall metabolic health, which is beneficial for those experiencing chronic migraines.
Additionally, exercise can act as a natural stress reliever, addressing one of the primary triggers for migraines. The endorphins released during physical activity provide natural pain relief and can lead to better overall mental health, reducing the likelihood of experiencing migraine attacks. Developing an individualized exercise plan can therefore be an integral part of a holistic approach to migraine management.
Future Directions in Migraine Research and Treatment
The future of migraine treatment lies in a deeper understanding of energy metabolism disorders and their intricate relationship with migraine pathology. Ongoing research is focused on revealing the complex mechanisms that link mitochondrial dysfunction, oxidative stress, and insulin resistance in individuals at risk for migraines. As therapeutic modalities evolve, there is strong potential for personalized approaches that consider a patient’s specific metabolic profile and migraine triggers.
Additionally, advancements in therapeutic repurposing and new nutritional interventions will likely emerge as vital components in the holistic management of migraines. By integrating knowledge of energy metabolism into treatment strategies, healthcare providers can improve the quality of care offered to patients, ultimately enhancing their ability to manage chronic migraines effectively.
Frequently Asked Questions
What are the common migraine triggers linked to energy metabolism disorders?
Common migraine triggers that are associated with energy metabolism disorders include factors like stress, sleep deprivation, fatigue, and strenuous exercise. These triggers can disturb brain energy metabolism and lead to mitochondrial dysfunction, ultimately exacerbating migraine symptoms.
How does mitochondrial dysfunction relate to energy metabolism disorders in migraines?
Mitochondrial dysfunction plays a critical role in energy metabolism disorders as it affects the brain’s ability to produce energy efficiently. In individuals with migraines, impaired mitochondrial function can lead to increased oxidative stress and contribute to the frequency and intensity of migraine attacks.
Can oxidative stress be a factor in energy metabolism disorders associated with migraines?
Yes, oxidative stress is a significant factor in energy metabolism disorders related to migraines. It results from an imbalance between the production of free radicals and the body’s ability to counteract their harmful effects. This oxidative stress can aggravate mitochondrial dysfunction, thereby influencing migraine pathology.
What role does insulin resistance play in energy metabolism disorders for migraine sufferers?
Insulin resistance is often observed in individuals with migraines and is linked to energy metabolism disorders. It can disrupt glucose metabolism and result in metabolic alterations that aggravate migraine attacks, ultimately impacting the overall energy balance and brain function.
How is therapeutic repurposing being used to address energy metabolism disorders in migraine treatment?
Therapeutic repurposing involves using existing medications to treat energy metabolism disorders associated with migraines. This approach targets metabolic pathways and aims to improve mitochondrial function and oxidative stress responses, potentially offering new avenues for migraine management.
What dietary changes can help improve energy metabolism in migraines?
Incorporating nutrients that support mitochondrial function, such as omega-3 fatty acids, antioxidants, and specific vitamins, can help improve energy metabolism in individuals suffering from migraines. These dietary adjustments may alleviate oxidative stress and enhance overall brain energy efficiency.
| Key Points |
|---|
| Migraine triggers include stress, sleep deprivation, fatigue, strenuous exercise, and fasting, linked to brain energy metabolism disturbances. |
| Prophylactic treatments targeting brain energy metabolism are gaining attention, though evidence in current guidelines is weak. |
| Explores metabolic alterations in migraine, including glucose and insulin metabolism, insulin resistance, lipid metabolism, and imaging markers. |
| Highlights the role of oxidative stress and antioxidant defenses alongside mitochondrial dysfunction in migraine. |
| Emphasizes potential of nutrients to improve mitochondrial function and mitigate energy metabolism deficits. |
Summary
Energy Metabolism Disorders are crucial in understanding the underlying mechanisms of migraine. This condition involves various triggers that may disrupt brain energy metabolism, including stress and fatigue. Current research emphasizes the importance of identifying metabolic alterations associated with migraine, such as issues in glucose and lipid metabolism. Furthermore, addressing mitochondrial dysfunction and oxidative stress may provide new avenues for therapeutic strategies. Understanding these elements is essential for developing more effective treatments and improving patients’ quality of life.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.