Understanding COVID-19 symptoms is crucial for distinguishing this illness from other respiratory infections like RSV and the flu. As cases of respiratory illnesses surge across the country, being able to identify the specific symptoms associated with COVID-19 can significantly impact your health and safety. Common symptoms include fever, cough, fatigue, and loss of taste or smell, which can overlap with flu symptoms and RSV symptoms, making diagnosis challenging. Knowing how to identify COVID-19 is essential, especially with the rise in emergencies reported by healthcare professionals. With various COVID-19 testing options available, timely testing can help determine the next steps for yourself and those around you.
When it comes to respiratory infections, differentiating between illnesses is vital, especially as we face challenges from COVID-19, influenza, and respiratory syncytial virus (RSV). Each condition presents a unique set of symptoms that can easily overlap, leaving many wondering about their health status. The flu, for example, typically manifests quickly with notable symptoms like chills and body aches, while RSV tends to cause gradual onset symptoms such as nasal congestion. Understanding these nuances can guide individuals to seek appropriate care and testing. Therefore, recognizing these respiratory virus signs becomes a key priority in safeguarding community health.
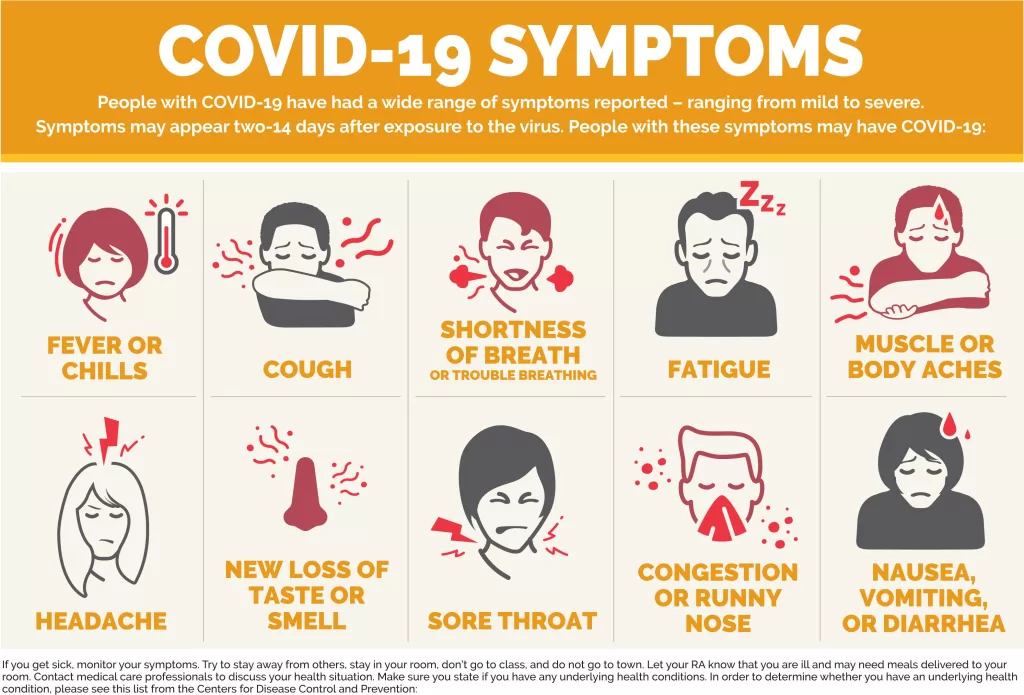
Recognizing COVID-19 Symptoms
Understanding the symptoms of COVID-19 is crucial for timely identification and treatment. COVID-19 symptoms often vary widely, with common indicators including cough, fatigue, and headaches. However, what sets COVID-19 apart from other respiratory illnesses like the flu and RSV is the potential for additional symptoms. For instance, nausea, vomiting, diarrhea, and the sudden loss of taste and/or smell are particularly associated with COVID-19, providing essential clues for those trying to determine their illness.
In contrast to traditional flu symptoms that typically manifest quickly and may include chills and body aches, COVID-19 symptoms can be milder and develop over a longer period. This can lead to confusion, emphasizing the need for individuals to remain vigilant. Identifying COVID-19 symptoms promptly allows for quicker testing and adherence to health guidelines, reducing the risk of transmission and complications.
Understanding RSV and Its Symptoms
Respiratory Syncytial Virus (RSV) is particularly concerning during respiratory illness seasons, especially for infants and the elderly. Symptoms of RSV can develop gradually, often starting with cold-like indicators such as congestion or a runny nose, followed by sneezing and occasionally wheezing. This gradual onset can sometimes make RSV harder to identify at first, contrasting sharply with the more acute presentation of the flu.
Additionally, RSV symptoms can escalate quickly in high-risk groups, leading to serious complications like bronchiolitis and pneumonia. Hence, monitoring symptoms closely in these vulnerable populations, such as infants and older adults, is essential for implementing timely medical interventions. Awareness of RSV’s characteristics helps caregivers and individuals seek appropriate care when symptoms arise.
Flu Symptoms and Their Importance
The flu typically presents with a sudden onset of symptoms, markedly distinguishing it from RSV and COVID-19. Common flu symptoms include fever, chills, body aches, and fatigue, often appearing abruptly within one to two days. Recognizing these symptoms is critical for determining the appropriate course of action, including seeking medical advice and possibly starting antiviral medications, especially for those at higher risk.
The CDC emphasizes that antiviral treatments are most effective when initiated early, ideally within the first couple of days after symptoms emerge. Therefore, anyone exhibiting flu symptoms, particularly high-risk individuals like the elderly or those with pre-existing health conditions, should be proactive in seeking medical evaluation to prevent serious complications.
COVID-19 vs. Flu: Key Differences
Distinguishing between COVID-19 and the flu is vital for effective treatment and containment. While both illnesses may share overlapping symptoms like cough, fatigue, and headache, other unique aspects help differentiate the two. For example, the flu is generally accompanied by a rapid onset of high fever and body aches, whereas COVID-19 might present with a more variable symptom profile that can include gastrointestinal symptoms and loss of taste and smell.
This understanding underscores the importance of COVID-19 testing options available, which can aid in accurately determining the illness. Testing can help differentiate COVID-19 from flu, thus guiding the appropriate treatment and reducing the potential spread of the virus.
Identifying COVID-19: Testing Options
When it comes to identifying COVID-19, various testing options are at the forefront of public health strategies. Individuals experiencing symptoms have access to several types of COVID-19 tests, including PCR and rapid antigen tests, which are crucial for accurate diagnosis. These tests can provide vital insights not only for individual care but also for controlling outbreaks within communities.
For optimal results, testing should be performed as soon as possible after symptom onset or following exposure to a confirmed case. As guidelines evolve, communities must remain informed about testing sites and the latest recommendations to ensure timely diagnosis and appropriate management of COVID-19, aiding both individual recovery and broader public health initiatives.
Monitoring Symptoms: A Critical Step
Regardless of the illness, keeping track of symptoms is vital for effective management and treatment decisions. Health professionals recommend paying close attention to the nature of your symptoms—whether they escalate or improve, how long they last, and any additional symptoms that may arise. This careful monitoring helps in differentiating between COVID-19, flu, and RSV, influencing the urgency to seek care.
In addition, documenting symptoms can assist healthcare providers in diagnosing and treating correctly, as patients present with unique variations in response to illness. Therefore, maintaining awareness of how respiratory symptoms evolve can guide treatment options and prevent complications associated with these common illnesses.
Preventative Measures Against Respiratory Illnesses
Prevention plays a fundamental role in controlling the spread of respiratory illnesses, particularly during peak seasons. Recommended measures include regular handwashing, wearing masks in crowded environments, and practicing physical distancing when symptoms arise. Vaccination is also a critical component, as vaccines for the flu and COVID-19 significantly reduce the risk of severe illness and complications.
Awareness of high-risk groups, such as the elderly or those with pre-existing conditions, highlights the importance of proactive vaccinations and preventive care. By adopting these strategies collectively, communities can work towards minimizing the impact of RSV, flu, and COVID-19, especially during challenging seasons when respiratory illnesses are prevalent.
Guidelines for Managing Respiratory Illnesses
Proper management of respiratory illnesses requires clear guidelines from health authorities. For illnesses like flu and COVID-19, staying informed about the latest recommendations on treatment options, quarantine measures, and when to seek medical attention is crucial. Following CDC guidelines can ensure patients receive the best possible care and minimize transmission risks.
In addition, health professionals advocate for awareness about individual self-care practices such as maintaining hydration, getting ample rest, and monitoring symptoms diligently. These practices not only aid in personal recovery but also reduce burdens on healthcare systems during peaks of respiratory illness outbreaks.
The Importance of Vaccination
Vaccination remains one of the most effective measures for preventing severe health outcomes associated with flu and COVID-19. The CDC emphasizes that everyone aged 6 months and older should receive the COVID-19 vaccine annually to ensure ongoing protection against emerging variants and potential severe illness. Furthermore, maintaining up-to-date flu vaccinations can play a pivotal role in decreasing hospitalizations and fatalities, particularly in vulnerable demographics.
In addition to routine vaccines, healthcare providers are now recommending RSV vaccinations for specific groups, which adds another layer of protection against respiratory illnesses. For infants and at-risk adults, these proactive immunizations are essential to help safeguard public health and curb the spread of RSV, flu, and COVID-19.
Frequently Asked Questions
What are the primary COVID-19 symptoms to watch for?
Common COVID-19 symptoms include a dry cough, fatigue, headache, sore throat, fever, chills, and unexpected loss of taste or smell. Some individuals may also experience nausea, vomiting, or diarrhea. If you notice these symptoms, it is important to consider getting tested for COVID-19, especially if you have been exposed to someone who has tested positive.
How can I differentiate between COVID-19 symptoms and flu symptoms?
While COVID-19 symptoms such as fatigue, cough, and fever overlap with flu symptoms, COVID-19 may also present unique signs like sudden loss of taste or smell. The flu typically manifests rapidly with intense body aches and chills. In contrast, COVID-19 symptoms can develop gradually and vary extensively between individuals.
Can RSV symptoms be confused with COVID-19 symptoms?
Yes, RSV symptoms can sometimes mimic COVID-19 symptoms. Both may include cough and fatigue. However, RSV typically presents with more nasal congestion, runny or stuffy nose, and wheezing compared to COVID-19, which may have unique symptoms like loss of taste or smell. Monitoring the progression of symptoms is crucial for accurate identification.
What are some COVID-19 testing options available?
Testing options for COVID-19 include PCR tests, which are highly sensitive and considered the gold standard, and rapid antigen tests, which provide quicker results but might be less accurate. Home testing kits are also available for convenience. It is advisable to test if you exhibit COVID-19 symptoms or have been in contact with someone who has contracted the virus.
What steps should I take if I suspect I have COVID-19 symptoms?
If you suspect you have COVID-19 symptoms, you should isolate yourself and contact your healthcare provider for guidance. They may recommend getting tested and advising on whether to seek further medical attention based on the severity of your symptoms. It is also essential to monitor your health closely and avoid contact with others.
How do COVID-19 symptoms compare to flu symptoms?
COVID-19 and flu symptoms can be quite similar, as both may include cough, fever, body aches, and fatigue. However, COVID-19 is more likely to cause symptoms such as loss of taste or smell and gastrointestinal symptoms, like diarrhea. Understanding these distinctions can help you identify which illness you might be experiencing.
What are the most common symptoms of COVID-19 in children?
Children may exhibit COVID-19 symptoms such as fever, cough, fatigue, and a sore throat, similar to adults. However, younger children may also have gastrointestinal symptoms like vomiting or diarrhea. Since symptoms can overlap with RSV and flu, parents should monitor their child’s health closely and consult a pediatrician if concerns arise.
When should I seek medical advice regarding COVID-19 symptoms?
Seek medical advice if you experience severe symptoms such as trouble breathing, chest pain, confusion, inability to stay awake, or bluish lips or face. These symptoms may indicate a severe case of COVID-19, and prompt medical attention is essential.
How can I protect myself from COVID-19 if I have flu-like symptoms?
If you have flu-like symptoms, it’s important to stay home, avoid close contact with others, and practice good hygiene, such as frequent hand washing. Wearing a mask can also help prevent the spread of potential respiratory viruses, including COVID-19. Consulting your healthcare provider about your symptoms and any necessary testing is also crucial.
| Illness | Common Symptoms | Treatment | Prevention |
|---|---|---|---|
| COVID-19 | Cough, fatigue, headache, nausea, vomiting, diarrhea, loss of taste/smell, sore throat | Over-the-counter medications; antiviral medications for those at risk | Vaccination, wearing masks, hand hygiene, avoiding crowds |
| Flu | Fever, chills, body aches, fatigue, dry cough | Antiviral medications, especially within 1-2 days of onset | Annual flu vaccination, staying home when sick |
| RSV | Congestion, runny/stuffy nose, sneezing, wheezing | Monitor symptoms closely; supportive care for severe cases | Vaccination for older adults; advice for pregnant women and caregivers of infants |
Summary
COVID-19 symptoms can be challenging to identify as they can overlap with those of the flu and RSV. It’s crucial to recognize the differences in symptoms and respond appropriately to protect your health and the health of others. As respiratory infections rise, understanding how COVID-19 presents itself, alongside effective prevention and treatment options, can help mitigate the spread and severity of the illness.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.