COVID-19 pneumonia long-term effects are becoming increasingly recognized as a significant health concern for survivors of severe COVID-19. A recent follow-up study indicated that nearly one-third of participants reported persistent cough and dyspnea long after recovery, highlighting the serious pulmonary complications associated with the disease. Additionally, individuals exhibited long-term COVID sequelae, with cognitive impairment affecting over half of the study’s participants. These findings reinforce the notion that severe COVID-19 outcomes can extend far beyond the initial infection, emphasizing the need for ongoing monitoring and support. As the global health community navigates the implications of postacute COVID syndrome, attention to these long-term effects is crucial in advocating for patient care and recovery strategies.
The long-lasting impacts of pneumonia caused by COVID-19 have drawn attention to the broader challenges faced by those recovering from this viral illness. Characterized by ongoing symptoms and complications, these effects can include respiratory difficulties, fatigue, and notable cognitive deficits in some individuals. Such manifestations—often referred to as post-COVID conditions—underscore the need for comprehensive care and evaluation strategies for affected populations. Understanding the ramifications of severe respiratory infections as part of long-term COVID-19 recovery is vital in framing effective public health responses. As research continues to evolve, it becomes imperative to identify and address the nuances of these debilitating long-term consequences.
Understanding Long-Term Outcomes of COVID-19 Pneumonia
COVID-19 pneumonia has emerged as a critical public health concern, particularly regarding its long-term outcomes in survivors. Evidence from clinical studies indicates that many individuals hospitalized with severe COVID-19 experience lingering health issues known as long-term COVID sequelae. Symptoms such as persistent cough, dyspnea, and cognitive deficits, often referred to as “brain fog,” can significantly impair quality of life for patients recovering from this viral infection. Observational studies have shown that these symptoms can persist for months after acute infection, necessitating thorough follow-up and management.
The data reveals that morbidity rates related to severe COVID-19 pneumonia extend well beyond recovery from the acute phase. For example, over a third of participants in recent studies reported ongoing dyspnea while about 30% faced cognitive impairments even 12 months post-hospitalization. This burdensome health landscape underscores the importance of understanding the full spectrum of recovery from COVID-19 pneumonia, as many of those affected could develop complications like pulmonary abnormalities that require long-term monitoring.
Cognitive Impairment Associated with COVID-19
One of the notable long-term effects of COVID-19 pneumonia is cognitive impairment, which has emerged as a prominent concern for healthcare providers. Studies report that a significant proportion of survivors experience difficulties with memory, attention, and problem-solving, which often correlate with the severity of their initial illness. The prevalence of cognitive deficits not only impacts the individual’s ability to return to everyday tasks but also raises concerns about long-term neurological health.
Emerging evidence suggests that mechanisms behind cognitive impairments may involve inflammation, hypoxia during the acute phase, and even direct viral invasion of neural tissues. Further research is required to understand postacute COVID syndrome fully and develop targeted rehabilitation plans. Cognitive rehabilitation interventions could be vital in aiding recovery from these long-term neurological complications, thereby significantly improving the quality of life for individuals suffering from post-covid cognitive issues.
The Importance of Monitoring Pulmonary Complications Post-COVID-19
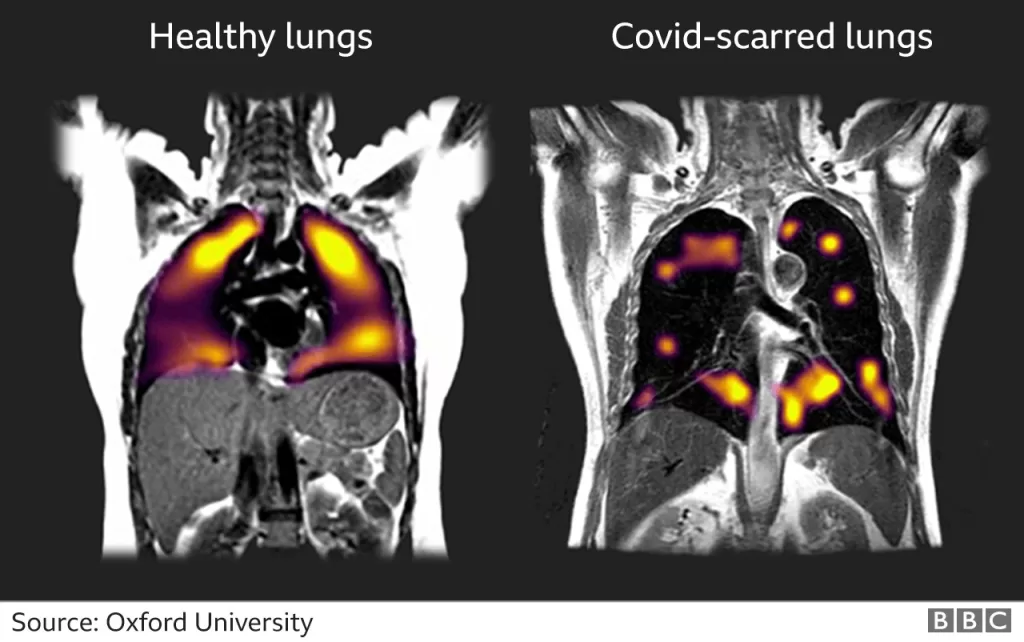
Pulmonary complications represent one of the most concerning health burdens following severe COVID-19 pneumonia. High-resolution CT scans in follow-up studies have revealed that a significant number of patients continue to display lung abnormalities long after their initial infection. These abnormalities, which include signs of lung fibrosis and reduced lung capacity, necessitate continuous pulmonary evaluation and intervention to manage symptoms effectively.
Regular monitoring of lung function is critical for maintaining health among COVID-19 survivors, particularly for older adults and those with pre-existing conditions. Cases of residual lung disease could lead to chronic respiratory issues, making it crucial to implement comprehensive follow-up measures. Continuous assessment can help clinicians tailor treatment strategies accordingly, prevent further deterioration, and promote recovery in those who experienced severe pulmonary impact due to COVID-19.
The Role of Age and Comorbidities in COVID-19 Recovery
Demographic factors such as age and underlying health conditions play a significant role in the recovery trajectory of individuals after severe COVID-19 pneumonia. Older adults or those with comorbidities like hypertension and obesity often experience a higher prevalence of long-term symptoms, including fatigue and cognitive impairment. The correlation between health status prior to infection and outcomes post-illness stresses the need for specialized care tailored to those at higher risk.
Longitudinal studies show that as patients age, the likelihood of experiencing adverse health effects post-COVID-19 increases. Monitoring these individuals can facilitate early identification of complications and improve treatment outcomes. Tailored interventions, including physical and cognitive rehabilitation, may be essential for this demographic to address the lingering effects of the virus.
Fatigue as a Common Sequela of Severe COVID-19
Fatigue is one of the most commonly reported long-term effects experienced by survivors of COVID-19 pneumonia. Nearly half of the participants in recent studies reported persistent fatigue well after their recovery from the acute phase of the illness. This debilitating symptom can significantly interfere with daily activities and overall health, varying in intensity from mild to severe among individuals.
Understanding fatigue as a sequela of COVID-19 is crucial for healthcare providers aiming to improve the quality of life for patients. Interventions focused on energy conservation techniques, graded exercise therapy, and psychological support might help alleviate the fatigue experienced by many post-recovery. Addressing this common complaint is vital in the holistic recovery of COVID-19 patients.
The Link Between Severe COVID-19 Pneumonia and Long-Term Health Implications
The connection between severe COVID-19 pneumonia and long-term health implications is increasingly recognized in clinical research. The l ability of COVID-19 to cause lasting damage to organs, particularly the lungs and brain, reveals a critical need for ongoing care and surveillance for those impacted by the virus. Health complications such as chronic pulmonary diseases and cognitive dysfunction can emerge long after the initial infection period.
This establishes a compelling argument for integrating long-term health monitoring into post-COVID treatment plans. As we learn more about the multifaceted impacts of COVID-19, healthcare systems must evolve to include long-term follow-up strategies aimed at managing and mitigating the potential complications that arise from previously severe infections.
Emerging Treatment Protocols for Long COVID Symptoms
As research continues to unveil the full spectrum of long-term COVID symptoms, new treatment protocols are being developed to address chronic complications. Healthcare professionals are now focusing on personalized therapeutic strategies that encompass physical rehabilitation, cognitive therapy, and psychosocial support. The recognition of these prolonged effects, termed post-acute COVID syndrome, has accelerated the need for effective management plans tailored to individual patient needs.
Recent clinical guidelines emphasize the significance of multidisciplinary approaches, capturing interventions that facilitate physiological recovery alongside psychological support. Evidence-based practices, including physical exercises and cognitive behavioral therapy, appear to be beneficial for patients grappling with long-term effects like fatigue and cognitive impairment. By prioritizing comprehensive treatment protocols, providers can enhance recovery trajectories for individuals affected by severe COVID-19 pneumonia.
The Impact of Public Health Policies on COVID-19 Outcomes
Public health policies have played a vital role in shaping COVID-19 outcomes, particularly in the context of hospitalizations and long-term health consequences. Access to early treatment and preventive measures, such as vaccinations, can significantly influence the severity of illness experienced by individuals who contract the virus. Communities with robust public health initiatives typically report better overall health outcomes compared to those with limited healthcare resources.
As we navigate the ongoing impact of COVID-19, the development of targeted public health strategies aimed at minimizing severe COVID-19 outcomes is crucial. Policymakers must prioritize resources for vaccination campaigns, public health education, and access to treatment facilities to alleviate the burden of long-term sequelae associated with COVID-19 infections, particularly in marginalized populations.
Research Directions for Future COVID-19 Studies
Future research directions in tackling long-term effects of COVID-19 pneumonia should focus on understanding the underlying mechanisms driving prolonged symptoms and developing effective treatment options. More comprehensive longitudinal studies are essential to disentangle the complex relationships between acute infection severity, long-term sequelae, and the efficacy of various rehabilitation interventions. As knowledge in this area expands, evidence-based frameworks for care will become increasingly critical.
Engaging diverse populations in research will also be crucial to ensure findings are generalizable. As we gain insights into the experiences of individuals from varying demographics, including age and comorbid conditions, tailored health interventions can be designed. This personalized approach can pave the way for improved healthcare outcomes, ultimately reducing the long-term health burden associated with COVID-19 pneumonia.
Frequently Asked Questions
What are the long-term effects of COVID-19 pneumonia?
The long-term effects of COVID-19 pneumonia can include persistent cough, dyspnea (difficulty breathing), cognitive impairment, fatigue, and pulmonary complications such as lung texture abnormalities. These long-term sequelae can significantly affect the quality of life and may extend well beyond the acute infection phase.
How does severe COVID-19 pneumonia impact pulmonary health in the long term?
Severe COVID-19 pneumonia can lead to lasting pulmonary complications, including impaired lung function and structural abnormalities detected via high-resolution CT scans. About 34.7% of individuals may experience residual lung issues even 12 months after recovery from the virus.
What is postacute COVID syndrome and how does it relate to COVID-19 pneumonia?
Postacute COVID syndrome, also known as long-COVID, encompasses a range of symptoms that persist after the initial COVID-19 infection, including those stemming from severe COVID-19 pneumonia. Patients may report ongoing fatigue, cognitive difficulties, and respiratory issues as part of this syndrome.
How common is cognitive impairment after COVID-19 pneumonia?
Cognitive impairment is surprisingly common among individuals recovering from COVID-19 pneumonia. Studies have shown that approximately 30.1% of participants report cognitive issues even up to a year post-hospitalization, indicating significant long-term effects on brain health.
What factors are associated with long-term effects following COVID-19 pneumonia?
Factors such as the severity of the initial COVID-19 infection, age, obesity, and underlying health conditions like hypertension are linked to a higher prevalence of long-term effects. Older adults and those with comorbidities are particularly at risk for persistent symptoms and complications.
How often should patients monitor for long-term effects after recovering from COVID-19 pneumonia?
It is recommended that individuals recovering from severe COVID-19 pneumonia undergo regular monitoring for long-term effects, especially during the first year post-discharge. This follow-up is crucial for detecting complications early and managing ongoing health concerns.
What are the implications of long-term COVID sequelae for healthcare systems?
The long-term sequelae of COVID-19 pneumonia pose significant challenges for healthcare systems, as many patients continue to require ongoing care and monitoring. Addressing these needs may strain resources, emphasizing the importance of preparedness for future public health crises.
| Key Point | Details |
|---|---|
| Study Design | Multicenter, observational, 12-month follow-up study. |
| Study Participants | 173 participants hospitalized for COVID-19 pneumonia; 134 (77.5%) completed the study. |
| Key Findings | 29.5% reported cough, 34.7% dyspnea, 30.1% cognitive impairment, 15.0% impaired lung capacity, 44.5% fatigue. |
| Associated Risk Factors | Disease severity, hypertension, age, and obesity linked to long-term effects. |
| Implications | Highlights need for ongoing monitoring and treatment for those recovering from severe COVID-19. |
Summary
COVID-19 pneumonia long-term effects can significantly impact patients’ health and quality of life. The recent study has shown that a notable portion of individuals who were hospitalized due to severe COVID-19 pneumonia experience ongoing symptoms such as cough, dyspnea, cognitive impairment, and fatigue even after one year. The correlation between disease severity and persistent lung abnormalities, alongside age and obesity as contributors to long-term cognitive issues, underscores the importance of continued medical follow-up. Regular evaluations are essential for managing these lasting effects and improving outcomes for patients recovering from COVID-19 pneumonia.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.