COVID-19 cardiovascular risk has emerged as a concerning factor in understanding the long-term health consequences of the pandemic. A recent NIH-funded study highlights that individuals infected with COVID-19, especially those who were unvaccinated during the initial wave, face a significantly elevated risk of heart attacks and strokes up to three years later. This increased cardiovascular risk, documented in the journal *Arteriosclerosis, Thrombosis, and Vascular Biology*, underscores the need for heightened awareness and preventive measures among those who contracted the virus. The findings reveal that people with a history of severe COVID-19 may experience nearly four times the risk of these life-threatening events compared to uninfected individuals. As the world continues to grapple with the implications of COVID-19, understanding its connection to heart health is critical for developing effective preventive strategies.
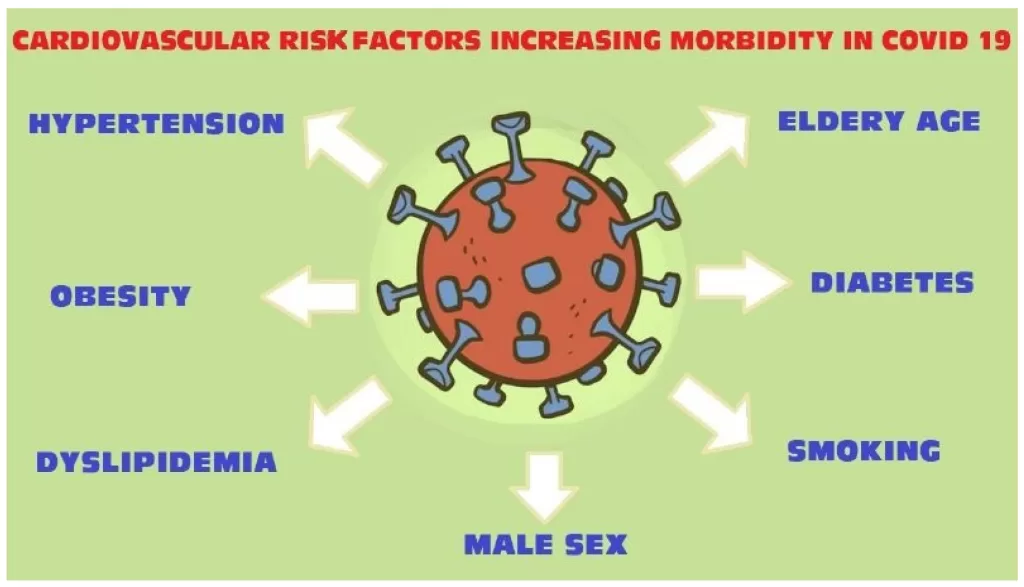
The impact of the COVID-19 pandemic on cardiovascular health has drawn significant attention, particularly regarding its long-lasting repercussions. Emerging evidence indicates that the virus may act similarly to other established risk factors for heart diseases, such as hypertension and diabetes, particularly for those who have not been vaccinated. The notion that infection with the virus could predispose individuals to future coronary events, like heart attacks or strokes, is a pivotal area of study. Additionally, what sets this research apart is its focus on those who experienced severe cases of the illness, suggesting an urgent need for public health strategies tailored to mitigate these risks. As researchers continue to delve into the relationship between COVID-19 and cardiovascular health, the findings reveal a complex interplay that could redefine our approach to heart disease prevention.
The Long-Term Cardiovascular Effects of COVID-19 Infection
Recent studies indicate that individuals who contracted COVID-19, particularly during its initial wave, may face significant long-term cardiovascular risks. Specifically, the NIH-funded study highlights that these individuals experience a doubled risk of heart attacks and strokes compared to those who never had the virus. This increase in risk persisted for up to three years after the infection, raising concerns about the long-term implications on heart health.
Moreover, the study emphasizes that the severity of the COVID-19 infection directly correlates with the extent of cardiovascular complications. Patients who suffered severe cases exhibited nearly a fourfold increase in the likelihood of experiencing adverse cardiovascular events. This data underscores the need for ongoing monitoring and preventative strategies targeting cardiovascular health in those who have recovered from COVID-19.
As COVID-19 poses a significant threat to public health, understanding its long-term effects on cardiovascular health is crucial. This pandemic has revealed that the aftermath of infection can lead to conditions that traditionally affect older populations, including heart attacks and strokes. With over 1 billion cases worldwide, the potential burden on healthcare systems can be profound, necessitating a reevaluation of cardiovascular disease prevention protocols.
COVID-19 Cardiovascular Risk: Insights from Recent Research
The recent findings from the NIH-funded study serve as a critical reminder of the cardiovascular risks associated with COVID-19. For unvaccinated individuals, the spike in heart attack and stroke incidents poses a serious threat that could rival established risk factors such as Type 2 diabetes. This study adds weight to previous assertions that severe COVID-19 should be regarded as an independent risk for cardiovascular disease. As public health authorities aim to mitigate the impacts of the pandemic, these insights can inform new guidelines for heart disease prevention strategies.
Additionally, the research highlights the concerning association between blood types and the severity of COVID-19. This genetic connection indicates that those with A, B, or AB blood types are more susceptible to severe cardiovascular outcomes following infection, compared to those with O type blood. Such findings may pave the way for personalized healthcare and targeted prevention measures tailored to individuals based on their genetic predispositions.
As the world transitions out of acute COVID-19 management, the implications of these cardiovascular risks must not be overlooked. The studies pinpointing the connection between COVID-19 severity and cardiovascular complications can guide future research and policy decisions. Researchers are urging the medical community to consider not only immediate impacts of COVID-19 but also its potential long-term health repercussions on the cardiovascular system.
Understanding the Genetic Links to COVID-19 Severity and Cardiovascular Risk
Recent investigations have shed light on genetic factors that may influence both COVID-19 severity and subsequent cardiovascular risks. The NIH study found significant variations in cardiovascular event outcomes among different blood types, suggesting a genetic component to how COVID-19 affects heart health. For instance, individuals with A, B, or AB blood types appeared to have a heightened risk of major cardiovascular issues, like heart attacks and strokes, compared to those with type O blood.
These revelations prompt further exploration into the genetic markers that may predispose individuals to severe COVID-19 outcomes and long-term cardiovascular risks. Such insights could lead to distinguishing which populations are at greater risk, allowing for preventative strategies that are more effective and tailored to individual needs. Understanding these dynamics will be essential for healthcare providers as they navigate the complexities of post-COVID-19 cardiovascular health.
This genetic link prompted researchers to investigate the vital intersection between COVID-19 and cardiovascular disease further. The NIH scientists emphasize the importance of these findings as they call for larger-scale studies to validate these results and explore the underlying mechanisms. By unraveling the genetic factors at play, they hope to contribute to the development of targeted therapies and preventive measures that could significantly decrease the incidence of heart-related complications in COVID-19 patients.
The Impact of Vaccination on COVID-19 Cardiovascular Outcomes
As vaccinations against COVID-19 have become widespread, a pressing question arises: Do vaccines mitigate the cardiovascular risks associated with the virus? The original NIH study focused on unvaccinated individuals, providing an essential baseline for understanding these risks. However, ongoing research is needed to determine if vaccinated individuals experience significantly different cardiovascular outcomes after COVID-19 infection.
Preliminary evidence suggests that vaccinations may reduce not just the severity of illness caused by COVID-19 but also potential long-term cardiovascular risks. Observing patterns of heart attack and stroke incidence in vaccinated populations versus unvaccinated ones will be pivotal in forming guidelines on cardiovascular health monitoring post-infection.
Furthermore, understanding the interaction between vaccination status and cardiovascular risks could reshape the ongoing response to the pandemic. If vaccines are indeed found to significantly lower these risks, this could bolster vaccination campaigns, significantly altering how public health officials advise at-risk populations. Research in this area remains urgent as it seeks to evaluate the protective effects of vaccines on cardiovascular health and their role in preventing long-term complications.
Addressing the Cardiovascular Risk in Unvaccinated Individuals
The data emerging from the NIH study emphasizes a critical public health concern for unvaccinated individuals: an intensified risk of heart disease following COVID-19 infection. This demographic is facing a twofold increase in their chances of experiencing severe cardiovascular events, compared to those who have not been infected with the virus. Considering the global vaccination rollout, addressing the specific needs of unvaccinated populations remains paramount while nurturing a plan to mitigate these risks further.
Health officials are urged to integrate cardiovascular health awareness into public discussions surrounding COVID-19, especially focusing on the conditions faced by unvaccinated individuals. Implementing community-wide educational programs could help convey the importance of vaccination and its potential protective effects against cardiovascular complications.
Moreover, healthcare practitioners should focus not only on the immediate treatment of COVID-19 symptoms but also on the long-term care and cardiovascular monitoring of unvaccinated patients. Establishing protocols that include regular heart health screenings and risk assessments will be essential for managing and mitigating these elevated risks.
Strategizing Future Cardiovascular Health Initiatives Post-Pandemic
The potential long-term cardiovascular impacts of COVID-19 underline the necessity for healthcare systems worldwide to reassess their approaches to heart disease prevention. The findings from the NIH study call for the integration of COVID-19 histories into cardiovascular risk assessments. Health officials must prioritize research that explores the lingering effects of COVID-19 on heart health and develop interventions aimed at reducing these risks for those who experienced severe infections or remain unvaccinated.
As countries move forward in their pandemic responses, it is critical to include cardiovascular health as a major component of recovery strategies. This could entail campaigns focused on healthy lifestyle interventions, routine health screenings, and increased access to preventative cardiology services for those impacted by COVID-19.
In the context of a global health crisis, these initiatives must also consider the diverse implications of COVID-19 on various populations, taking into account factors like ethnicity and socioeconomic status. Tailoring approaches that address vulnerability in populations that were disproportionately affected by the virus will enhance overall public health outcomes.
Monitoring Heart Health in Recovering COVID-19 Patients
As the healthcare community continues to navigate the repercussions of the COVID-19 pandemic, close monitoring of heart health among recovering patients takes on new importance. The NIH study highlights the need for ongoing cardiovascular evaluations in patients with a history of COVID-19 infection, especially those who were unvaccinated during the early stages of the pandemic. Regular screenings could help identify and manage increased risks of heart attacks or strokes that may arise in these individuals.
Incorporating routine cardiovascular assessments for former COVID-19 patients can facilitate early intervention strategies to mitigate long-term complications. By collaborating across primary care, cardiology, and rehabilitation sectors, healthcare providers can create comprehensive care plans tailored to the unique heart health needs of patients recovering from COVID-19.
Patients who have experienced severe COVID-19 require specialized follow-up care, particularly if they present with pre-existing conditions or exhibit risk factors for cardiovascular disease. Healthcare providers should foster an environment in which patients feel empowered to discuss their cardiovascular health concerns, promoting a proactive approach to post-COVID-19 care.
Collaborative Efforts in COVID-19 Cardiovascular Research
The results of the NIH study prompt the necessity for ongoing collaborative efforts in cardiovascular research related to COVID-19. Researchers are called upon to broaden the scope of investigations, addressing the cardiovascular implications of COVID-19 across diverse populations and settings. By pooling resources and expertise, the scientific community can enhance understanding of the virus’s cardiovascular impact and develop practical interventions for prevention and treatment.
Transdisciplinary research initiatives could facilitate breakthroughs in understanding how COVID-19 infection correlates with cardiovascular morbidity. Engaging with specialized cardiovascular researchers, public health experts, and epidemiologists will be essential in creating comprehensive studies that accurately reflect the long-term implications of COVID-19 on heart health.
By fostering collaboration among institutions and leveraging large datasets procured from various populations, researchers can derive insights that support the advancement of cardiovascular medicine in the context of post-COVID health. These collective efforts will enhance the ability to ascertain the true scope of the cardiovascular crisis triggered by the pandemic and inform better strategies for managing risks moving forward.
Frequently Asked Questions
What is the relationship between COVID-19 and cardiovascular risk?
Research indicates that COVID-19 significantly increases cardiovascular risk, particularly for heart attacks and strokes. A NIH-funded study found that unvaccinated individuals who contracted COVID-19 during the pandemic’s first wave had a doubled risk of these events, with severe cases leading to nearly a fourfold increase in risk.
How long does the increased cardiovascular risk from COVID-19 last?
The increased risk of cardiovascular events such as heart attacks and strokes can persist for up to three years after recovering from COVID-19, particularly in unvaccinated individuals who were infected during early waves of the pandemic.
Are unvaccinated individuals at greater risk for heart attacks and strokes after COVID-19?
Yes, unvaccinated individuals who contracted COVID-19 early in the pandemic exhibited a significantly higher risk for heart attacks and strokes compared to those who did not have the virus, emphasizing the importance of vaccination for reducing cardiovascular risks.
What are the long-term effects of COVID-19 on heart health?
Long-term effects of COVID-19 on heart health include an increased risk of cardiovascular events such as heart attacks and strokes, especially among those with severe cases. Studies suggest that this risk could last for years and highlights the need for cardiovascular disease awareness and preventative measures.
How does the severity of COVID-19 infection affect cardiovascular risk?
Individuals who experience severe COVID-19 have a markedly higher risk of cardiovascular events. Research shows they face almost a fourfold increase in the chance of heart attacks and strokes compared to those who had mild or no symptoms, emphasizing the seriousness of severe infections.
Is there a genetic component to COVID-19 cardiovascular risk?
Preliminary findings suggest there may be a genetic link related to blood type that influences cardiovascular risk after severe COVID-19 infections. Patients with blood types A, B, or AB had a higher risk of heart attack or stroke compared to those with type O blood, pointing to a potential area for further study.
How does COVID-19 infection compare to other cardiovascular disease risk factors?
COVID-19 infection may be considered an equivalent risk factor for cardiovascular disease, similar to recognized factors like Type 2 diabetes. Those with a history of severe COVID-19 could benefit from focused heart disease prevention strategies due to their heightened risk.
Will vaccination provide protection against COVID-19 related cardiovascular risk?
While current research primarily involves unvaccinated individuals, it remains unclear how vaccination affects cardiovascular risk after COVID-19. Further studies are needed to explore the impact of vaccines on long-term heart health outcomes.
What steps should individuals take to manage cardiovascular risk after COVID-19?
Individuals recovering from COVID-19, especially those who were severely affected, should consult with healthcare professionals to assess their cardiovascular health and discuss potential preventive measures for heart disease. Regular monitoring and lifestyle modifications can help manage risks.
Where can I find more information about COVID-19 and heart health?
For more information regarding COVID-19 and heart health, resources such as the National Heart, Lung, and Blood Institute (NHLBI) and research published in medical journals like *Arteriosclerosis, Thrombosis, and Vascular Biology* provide valuable insights and updates.
| Key Points |
|---|
| COVID-19 significantly increases cardiovascular risks for up to three years post-infection, particularly for unvaccinated individuals during the first pandemic wave. |
| Doubling of heart attack and stroke risk for COVID-19 survivors; severe cases increase risk nearly fourfold. |
| Study utilized data from 10,000 UK Biobank participants aged 40-69, tracking health outcomes over nearly three years. |
| Patients with A, B, or AB blood types have a significantly higher risk of heart attack or stroke compared to those with O type blood. |
| Implications for public health are vast, emphasizing the need for cardiovascular disease prevention strategies in COVID-19 patients. |
| Future studies needed to explore the effects of COVID-19 vaccination on cardiovascular risk and racial/ethnic differences in findings. |
Summary
COVID-19 cardiovascular risk has been shown to be significantly heightened for up to three years after infection, especially among unvaccinated individuals from the initial pandemic wave. As studies reveal alarming correlations between COVID-19 and increased rates of heart attacks and strokes, it is essential to recognize the long-term implications of this virus on cardiovascular health. Continued research is crucial for developing preventive strategies and understanding the complexities of this relationship, particularly regarding various patient demographics and vaccination effects.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.