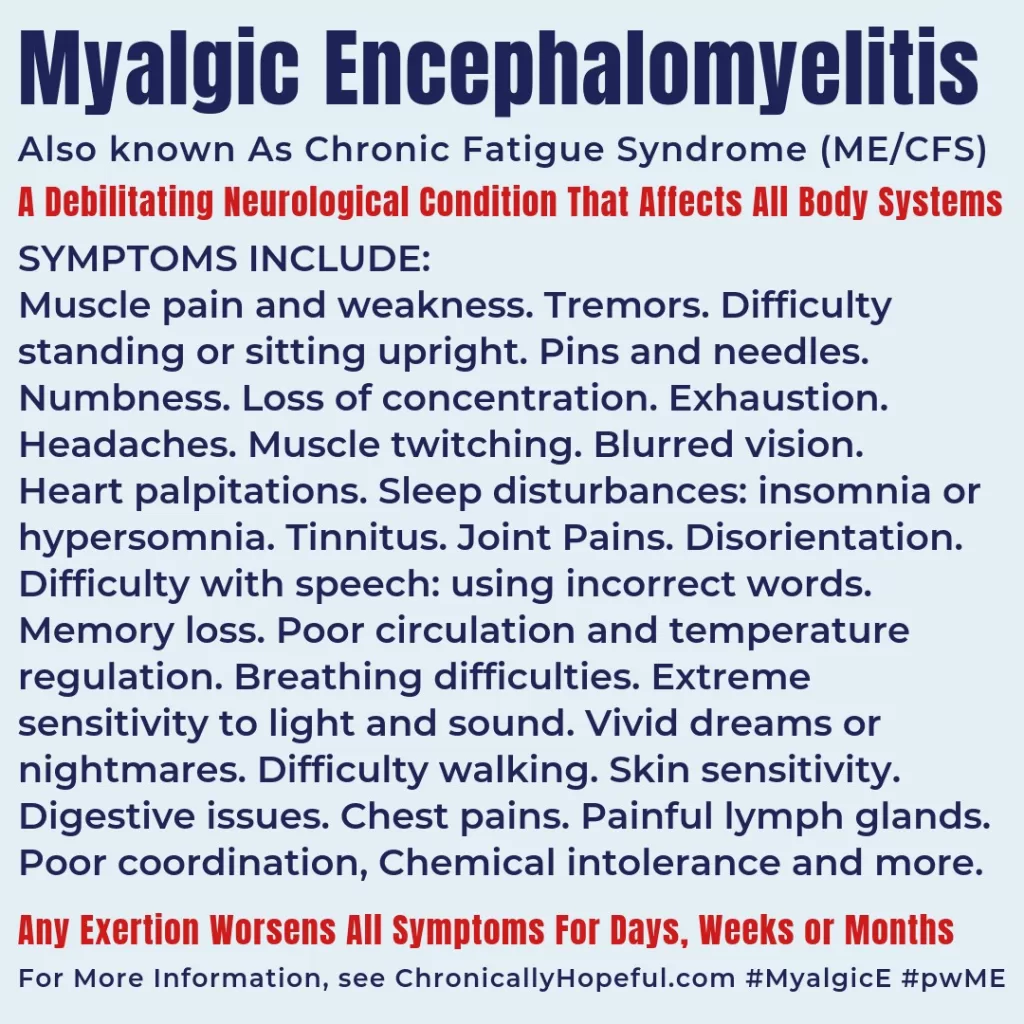
Coping with Myalgic Encephalomyelitis (ME), commonly referred to as Chronic Fatigue Syndrome (CFS), presents unique challenges that demand a proactive approach. Individuals with this debilitating condition often endure uncontrollable fatigue and cognitive issues that can dominate daily life. However, there are effective ME/CFS management strategies available that can aid in symptom relief and enhance overall quality of life. By employing pacing techniques and engaging in Cognitive Behavioral Therapy (CBT), you can better navigate the complexities of ME/CFS. Additionally, connecting with support groups for ME/CFS can provide a sense of community and understanding, making the journey slightly easier.
Living with Myalgic Encephalomyelitis (also known as ME/CFS) can feel overwhelming, but understanding the disorder and its management options is crucial. This condition, characterized by extreme fatigue and a variety of other symptoms, can leave individuals searching for answers and effective coping strategies. Utilizing holistic approaches, such as pacing and alternative therapies, forms a comprehensive plan that addresses both physical and mental health. Furthermore, engaging in support networks can significantly improve emotional resilience, providing essential encouragement to those affected. Exploring various coping methods can empower individuals to regain control and improve their overall well-being.
The Importance of Pacing Techniques in Managing ME/CFS
Pacing techniques are crucial for individuals coping with Myalgic Encephalomyelitis (ME/CFS) as they help prevent the exacerbation of symptoms. By carefully balancing activity with rest, patients can learn to manage their energy levels effectively. Recognizing the limits of one’s physical and mental endurance is fundamental in the fight against chronic fatigue. Implementing a well-structured routine that includes scheduled breaks can make a substantial difference in daily functioning.
In practice, pacing means scheduling your day and breaking tasks into manageable segments to avoid over-exertion. This approach not only aids in symptom management but also fosters a more positive outlook on daily activities. As individuals begin to track their energy levels and recognize patterns, they can refine their pacing strategies, ultimately leading to improved quality of life.
Cognitive Behavioral Therapy (CBT) for ME/CFS
Cognitive Behavioral Therapy (CBT) offers significant benefits for those managing the challenges of ME/CFS. This therapy focuses on changing negative thought patterns that often accompany chronic illness, which can further exacerbate stress and emotional distress. By adopting healthier coping mechanisms, individuals may find relief from symptoms and an enhanced sense of control over their condition.
Engaging in CBT with a trained therapist can provide personalized guidance tailored to the unique experiences of ME/CFS patients. This professional support can help individuals develop practical skills to address the emotional challenges of living with chronic fatigue, ultimately contributing to a better overall quality of life.
Lifestyle Modifications to Alleviate Myalgic Encephalomyelitis Symptoms
Making thoughtful lifestyle modifications can substantially alleviate symptoms of Myalgic Encephalomyelitis (ME/CFS). Gentle exercises, such as yoga and tai chi, promote physical health without triggering exacerbations of fatigue. These low-impact activities not only help maintain mobility but also improve mental well-being, making them essential components of a comprehensive management plan.
Additionally, focusing on nutrition and sleep hygiene plays a pivotal role in managing sensitive symptoms. A balanced diet rich in essential nutrients can fortify the body’s defenses, while prioritizing quality sleep ensures that individuals can recover effectively. Together, these lifestyle changes create a supportive environment for those navigating the complexities of ME/CFS.
Building a Community Support Network for ME/CFS
Connecting with others who understand the struggles of Myalgic Encephalomyelitis (ME/CFS) can be incredibly empowering. Support groups provide invaluable opportunities for individuals to share experiences and coping strategies, thereby fostering a sense of community. Engaging with online or in-person groups not only offers validation but also helps to alleviate feelings of isolation commonly experienced by patients.
Participation in these networks can lead to new friendships and emotional support, while also empowering members to exchange educational resources. This ongoing connection with others facing similar challenges is a vital component in managing the psychological aspects of chronic fatigue syndrome, significantly enhancing one’s resilience and overall quality of life.
Exploring Alternative Therapies for Myalgic Encephalomyelitis Management
While traditional treatments are important, exploring alternative therapies for Myalgic Encephalomyelitis (ME/CFS) can also provide symptomatic relief. Techniques such as acupuncture and massage therapy may alleviate pain and enhance relaxation, thus contributing to improved overall well-being. These methods can complement conventional therapies and provide diverse options for managing symptoms.
Mindfulness practices, including meditation, offer additional benefits by reducing stress and promoting a sense of calm. Integrating such alternative therapies into a holistic management approach can empower individuals to take an active role in their health and wellness journey. Consulting healthcare providers helps ensure safety and optimal combination of therapies to best address ME/CFS symptoms.
Frequently Asked Questions
What are effective pacing techniques for coping with Myalgic Encephalomyelitis (ME)?
Pacing techniques for coping with Myalgic Encephalomyelitis (ME) involve balancing activities with periods of rest. Schedule your day by breaking tasks into manageable segments, ensuring you allocate time for both activity and rest. Recognize your body’s limits to prevent exacerbation of symptoms, and consider using a daily planner to help visualize your activities and identify patterns that may aid in adjusting your approach.
How can Cognitive Behavioral Therapy help in managing Myalgic Encephalomyelitis (ME/CFS)?
Cognitive Behavioral Therapy (CBT) can aid in managing Myalgic Encephalomyelitis (ME/CFS) by improving coping mechanisms and helping to change negative thought patterns associated with illness. This therapeutic approach promotes healthier strategies for managing stress and may enhance emotional well-being, ultimately improving the quality of life for individuals coping with ME/CFS.
What lifestyle modifications can support individuals coping with Myalgic Encephalomyelitis (ME)?
Lifestyle modifications for coping with Myalgic Encephalomyelitis (ME) include incorporating gentle exercise like yoga or tai chi, prioritizing sleep hygiene by establishing a regular sleep schedule, and consuming a balanced diet rich in nutrients. Staying hydrated and avoiding stimulants can also significantly improve overall well-being and help manage ME symptoms.
What role do support groups play in coping with Myalgic Encephalomyelitis (CFS)?
Support groups are crucial for individuals coping with Myalgic Encephalomyelitis (CFS) as they provide a safe space for sharing experiences, challenges, and coping strategies. Engaging with online communities or local in-person meetings fosters emotional support and can lead to valuable connections that enhance the coping process for those affected by ME/CFS.
What alternative therapies might help alleviate symptoms of Myalgic Encephalomyelitis (ME)?
Alternative therapies that may help alleviate symptoms of Myalgic Encephalomyelitis (ME) include acupuncture, which can reduce pain and fatigue, therapeutic massage to relieve tension, and mindfulness practices such as meditation to reduce stress. Consider consulting a healthcare provider before starting any alternative treatments to ensure they align with your overall management plan.
| Strategy | Key Points |
|---|---|
| Understanding ME/CFS | Characterized by persistent fatigue, sleep disturbances, pain, and cognitive issues. Symptoms vary widely, necessitating personalized coping strategies. |
| Pacing and Activity Management | Involves balancing activities with rest to avoid exacerbation of symptoms. Tips include scheduling, recognizing limits, and using a daily planner. |
| Cognitive Behavioral Therapy (CBT) | Helps change negative thought patterns, improves coping strategies, and promotes emotional well-being. |
| Medications and Supplements | No cure, but antidepressants, pain relievers, and certain supplements like magnesium may ease symptoms. |
| Lifestyle Modifications | Include gentle exercise, improving sleep hygiene, and a nutritious diet to support overall health. |
| Building a Support Network | Engaging with support groups provides emotional support and practical coping strategies. |
| Exploring Alternative Therapies | Options like acupuncture and mindfulness practices may help reduce symptoms. |
| Recent Research Developments | Ongoing studies on immune dysfunction offer hope for targeted therapies. |
Summary
Coping with Myalgic Encephalomyelitis requires a multifaceted approach combining various strategies tailored to individual needs. Effective management involves understanding the complexities of the illness and utilizing techniques such as pacing, cognitive behavioral therapy, and lifestyle modifications to improve day-to-day functioning. Building a supportive network and exploring alternative therapies can further enhance quality of life. With ongoing research shedding light on potential new treatments, those living with ME/CFS can remain hopeful for advancements in care and support.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.