Chlamydia and gonorrhea treatment is crucial in managing these common sexually transmitted infections (STIs) that continue to rise in incidence across the United States. Recent studies highlight disturbing trends in treatment adherence, with many patients not receiving care that meets established STI treatment guidelines, particularly those set by the CDC. Alarmingly, nearly 30% of individuals diagnosed with chlamydia and gonorrhea do not receive any treatment, while a significant portion who are treated do not follow the recommended protocols for their recovery. Understanding and addressing the barriers to timely and adequate treatment are essential for public health, as untreated infections can lead to serious long-term health complications and further transmission. Ultimately, adherence to chlamydia guidelines and effective gonorrhea treatment adherence must be prioritized to improve health outcomes in primary care settings.
When addressing the management of chlamydia and gonorrhea, we delve into the vital aspect of STI healthcare that demands significant attention. These infections, which pose serious health risks if neglected, require rigorous adherence to specific medical guidelines for effective treatment. Healthcare professionals must familiarize themselves with the CDC recommendations for STIs to ensure that patients receive optimal care. Issues surrounding treatment adherence, especially in primary healthcare environments, are paramount as they influence the likelihood of successful recovery. Moreover, understanding the social determinants of health is key to addressing disparities in treatment rates among different demographics.
Understanding Chlamydia and Gonorrhea Treatment Guidelines
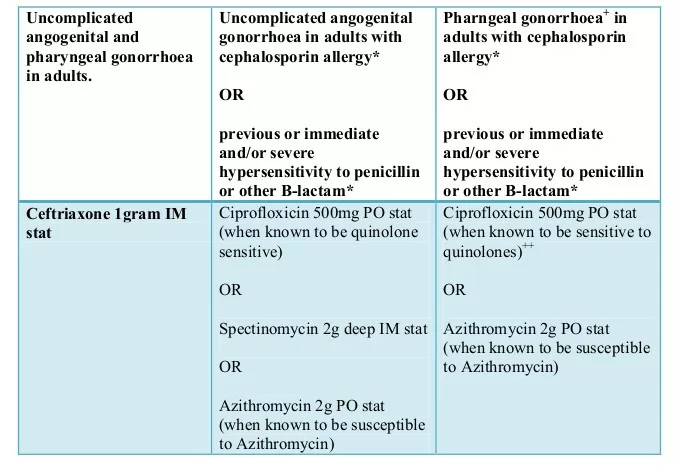
Effective treatment of chlamydia and gonorrhea is crucial for controlling these prevalent STIs. The Centers for Disease Control and Prevention (CDC) has established comprehensive guidelines to help primary care providers ensure that patients receive the most appropriate medications. According to the CDC recommendations, first-line treatment for chlamydia commonly includes doxycycline or azithromycin, while gonorrhea is typically addressed with ceftriaxone, often accompanied by azithromycin to prevent resistance. However, a recent study highlights that adherence to these guidelines in primary care settings is dangerously low, with many patients receiving suboptimal treatment that deviates from established protocols.
As indicated by the research conducted by Stanford University and the CDC, a significant portion of patients—30%—did not receive any treatment for their infections, which can lead to severe health complications and further transmission. This gap in treatment adherence underlines the importance of education and consistent practice among healthcare providers. Implementing tailored training programs on the latest STD treatment guidelines will equip clinicians with the necessary knowledge to provide effective care that aligns with CDC recommendations. Moreover, ensuring accessibility to these guidelines can further empower healthcare professionals to tackle the rising incidence of these STIs.
Barriers to STI Treatment in Primary Care Settings
Despite the availability of effective treatment options, numerous barriers prevent timely and appropriate care for patients diagnosed with chlamydia and gonorrhea. Factors such as racial and ethnic disparities play a significant role, as evidenced by the study’s findings that indicated longer treatment times for non-Hispanic Black patients compared to their non-Hispanic White counterparts. Additionally, socioeconomic determinants such as income, insurance status, and access to healthcare services can further complicate treatment adherence. Urban residents may experience delays in receiving care due to logistical challenges, while residents in suburban areas generally demonstrated higher treatment rates.
Moreover, the fear of stigma associated with STIs can deter patients from seeking immediate treatment. Public health initiatives focusing on reducing stigma and encouraging open discussions about sexual health can foster an environment where individuals feel comfortable seeking care. Additionally, enhancing communication between patients and providers will bridge knowledge gaps, enabling discussions that prioritize the necessity of adhering to STI treatment guidelines. By addressing these barriers with targeted strategies, healthcare systems can significantly improve treatment outcomes and help curb the spread of sexually transmitted infections.
The Importance of Prompt Treatment for STIs
Prompt treatment of chlamydia and gonorrhea is vital for preventing serious health complications, including infertility, pelvic inflammatory disease, and increased vulnerability to HIV. The recent study revealed that, on average, patients received treatment within three days of diagnosis; however, this timeframe varies widely among different demographic groups. Timely intervention not only protects the health of individuals but also plays a critical role in public health by reducing the overall incidence of STIs in the community. The report emphasized that substantial public health resources are expended to address STI-related care, which underscores the need for swift treatment.
As the study pointed out, the preference for antibiotics not recommended by the CDC—like azithromycin for chlamydia—highlights a lack of adherence to established treatment guidelines. Reducing the time to treatment and ensuring that patients receive the recommended antibiotics can significantly contribute to limiting the spread of these infections. Healthcare providers should be proactive in following CDC recommendations for STIs, as rapid diagnosis and administration of effective antibiotics are critical components in managing chlamydia and gonorrhea effectively. Clinician adherence to treatment guidelines should be reinforced through continuous medical education and systematic review of treatment practices.
Addressing Racial and Ethnic Disparities in STI Treatment
The findings from the study also revealed that racial and ethnic disparities significantly impact the treatment of STIs such as chlamydia and gonorrhea. Non-Hispanic Black patients, in particular, experienced longer waiting times for treatment compared to other racial groups. This discrepancy highlights a pressing public health issue that requires an urgent intervention to ensure equitable access to healthcare services. Understanding the social determinants that contribute to these disparities is essential in developing targeted strategies to improve treatment access and adherence.
To combat these inequities, healthcare systems should aim to implement culturally competent care that acknowledges and respects diverse backgrounds. Furthermore, increasing outreach efforts in communities disproportionately affected by STIs can promote awareness of treatment protocols and reduce barriers to care. By enhancing access to properly aligned STI treatment guidelines and fostering stronger relationships between healthcare providers and vulnerable communities, we can work towards eliminating the disparities that plague sexual health outcomes in marginalized populations.
The Role of Primary Care in STD Prevention
Primary care providers play a pivotal role in the prevention and treatment of STIs, including chlamydia and gonorrhea. They are often the first point of contact for patients and are in a strategic position to educate individuals about safe sex practices and the importance of screening. The recent study highlights a critical gap in the adherence to treatment guidelines, indicating that primary care settings need to be more proactive in addressing these infections. By implementing routine screening for STIs as part of regular health check-ups, clinicians can facilitate early detection and timely treatment, reducing the overall burden of these diseases.
Moreover, the integration of clinical practice guidelines into everyday patient interactions can help clinicians make informed decisions about treatment options. Continuing education initiatives that focus on current CDC recommendations can assist providers in improving their knowledge of STI management and treatment adherence. When primary care providers prioritize STI prevention strategies and conform to established treatment protocols, it will not only enhance patient outcomes but also contribute to the broader public health goal of reducing the incidence of STIs in the community.
Encouraging Adherence to CDC Recommendations for STIs
Encouraging adherence to the CDC recommendations for STI treatment is paramount for both individual and public health. The low rates of compliance seen in the study highlight the pressing need for healthcare providers to align their prescribing practices with current guidelines. Ensuring that first-line antibiotics are available and educating healthcare professionals about their efficacy can lead to improved patient outcomes. Continued efforts should be made to monitor treatment practices and adjust them according to best practices outlined by the CDC. By doing so, we can foster a culture of adherence that prioritizes the health and wellbeing of patients.
Additionally, healthcare systems can implement reminder systems or alerts within electronic health records (EHR) that prompt providers to follow guidelines when treating patients diagnosed with STIs. These tools can serve to reduce human error and increase the rates of appropriate prescribing. Patient education regarding their treatment options is equally important; informed patients are more likely to understand and appreciate the necessity of following treatment recommendations. Overall, reinforcing the importance of adherence to CDC guidelines will play a vital role in controlling the escalation of chlamydia and gonorrhea in our communities.
Public Health Implications of Untreated STIs
The consequences of untreated STIs extend far beyond individual health, influencing public health on a larger scale. The study reveals that a considerable number of young adults live with untreated chlamydia and gonorrhea, creating a cycle of transmission that endangers community health. The ongoing prevalence of these infections underscores the urgent need for effective public health strategies aimed at improving awareness and access to treatment. As STIs can lead to serious health complications, including increased infertility rates and higher susceptibility to other infections, untreated cases represent a significant public health challenge that must be addressed.
Moreover, as STI incidence continues to rise in the United States, public health authorities must allocate resources effectively to combat this trend. Investments in educational campaigns that promote sexual health awareness, free or low-cost STI testing, and treatment facilities are essential in reducing the burden of these infections. Equally important is the collaboration between public health agencies, healthcare providers, and community organizations to foster an environment that supports preventive care and treatment adherence. Ultimately, successful management of STIs hinges on a comprehensive strategy that addresses both education and access to care.
Future Directions in STI Research and Treatment
As the study indicates, there is a pressing need for further research into the barriers surrounding STI treatment adherence, especially in vulnerable populations. Understanding the dynamics that contribute to disparities in treatment access and adherence will inform the creation of tailored interventions aimed at improving care delivery. Future studies should explore innovative approaches to enhance patient engagement, such as telemedicine and mobile health applications, making care more accessible, particularly in underserved areas.
Additionally, expanding research on the effectiveness of new and existing treatment protocols will help healthcare providers stay informed about the best practices for managing STIs. Investigating the development of rapid diagnostic tests that facilitate immediate treatment can also be a game-changer in addressing the delays witnessed in primary care settings. By prioritizing research that addresses these gaps, the healthcare community can make substantive progress in improving treatment outcomes for chlamydia and gonorrhea, ultimately leading to a reduction in STI prevalence across the nation.
Frequently Asked Questions
What are the CDC recommendations for chlamydia and gonorrhea treatment?
The CDC recommends treating chlamydia with doxycycline or azithromycin, and gonorrhea with ceftriaxone. It’s crucial that treatment adheres to these guidelines to prevent complications and the spread of these STIs.
Why is adherence to STI treatment guidelines essential for chlamydia and gonorrhea?
Adhering to STI treatment guidelines for chlamydia and gonorrhea is vital as it ensures effective treatment, reduces the risk of long-term health issues, and minimizes the ongoing transmission of these infections.
How does primary care affect chlamydia and gonorrhea treatment outcomes?
Primary care plays a significant role in chlamydia and gonorrhea treatment outcomes, as many patients may not receive timely treatment adhering to established guidelines, impacting both individual health and public health metrics.
What factors influence gonorrhea treatment adherence in primary care?
Factors such as patient demographics, including race and gender, as well as the choice of antibiotics, greatly influence gonorrhea treatment adherence in primary care settings, often leading to lower usage of CDC-recommended treatments.
What are the implications of untreated chlamydia and gonorrhea infections?
Untreated chlamydia and gonorrhea infections can result in severe long-term health issues, including infertility and increased susceptibility to other STIs, highlighting the urgency of following treatment guidelines.
What social determinants may affect chlamydia and gonorrhea treatment in patients?
Social determinants such as socioeconomic status, access to healthcare, and cultural factors can significantly impact chlamydia and gonorrhea treatment adherence and timeliness among patients.
How effective are rapid diagnostic tests in improving chlamydia and gonorrhea treatment rates?
Rapid diagnostic tests can significantly reduce the turnaround time for treatment and improve adherence to guidelines for chlamydia and gonorrhea, thus enhancing care outcomes.
What challenges do primary care providers face in following chlamydia guidelines?
Primary care providers often face challenges including patient adherence issues, misalignment with recommended antibiotic treatments, and variability in treatment based on demographic factors that complicate guideline adherence.
What are the treatment rates for chlamydia and gonorrhea among different demographics?
Treatment rates for chlamydia and gonorrhea differ significantly across demographics, with studies showing higher rates among women and non-Hispanic White patients as compared to other racial and ethnic groups.
Why do treatment rates for chlamydia and gonorrhea vary by race and ethnicity?
Treatment rates for chlamydia and gonorrhea vary by race and ethnicity due to a combination of factors including access to care, cultural perceptions of STIs, and healthcare provider biases.
| Key Findings | Details | |
|---|---|---|
| Study Analysis | Conducted by Stanford University and CDC on US primary care patients. | |
| Treatment Adherence | 30% of patients with chlamydia and gonorrhea did not receive treatment. | |
| Antibiotics Used | Only 14% of chlamydia and 38.7% of gonorrhea patients received first-line antibiotics. | |
| Demographic Variations | Treatment rates varied by race, ethnicity, gender, and age. | |
| Time to Treatment | Median time to treatment was 3 days post-positive test result. | |
| Need for Improvements | More efforts are needed to understand and address treatment delays. | |
Summary
Chlamydia and Gonorrhea Treatment must be prioritized to address the staggering rates of untreated infections identified in a recent study. This analysis reveals critical gaps in adherence to treatment guidelines, highlighting the need for reinforcing public health initiatives. By ensuring timely and appropriate treatment for these common sexually transmitted infections (STIs), we can significantly reduce long-term health complications and the spread of infections in the population.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.