Cervical spondylosis is a prevalent degenerative condition affecting the cervical spine, primarily due to the natural aging process. As individuals grow older, the wear and tear on the neck’s vertebrae and discs can lead to spinal complications, including compression of the spinal cord, a condition known as myelopathy. Recognizing the symptoms of cervical spondylosis—such as neck pain, stiffness, and neurological deficits—is crucial for early intervention and effective cervical myelopathy treatment. Understanding cervical spine health becomes increasingly important as it plays a fundamental role in overall well-being and mobility, particularly in aging populations. Through this post, we will explore further into the intricacies of cervical spondylosis and its implications for spinal health, highlighting the key symptoms, diagnostic approaches, and modern treatment options available.
Cervical spondylosis, commonly referred to as neck arthritis or cervical osteoarthritis, encompasses age-related degenerative changes within the cervical spine. As time progresses, these changes can lead to significant discomfort and functional impairments, manifesting as a syndrome that can severely impact quality of life. This condition is often linked with various neurological symptoms, including those associated with cervical myelopathy—an alarming scenario where spinal cord pressure can cause weakness or sensory deficits. As we delve deeper into the topic, it’s essential to discuss the nuances of aging and spinal health, as well as the available treatment methodologies to manage symptoms effectively.
Understanding Cervical Spondylosis: Causes and Risk Factors
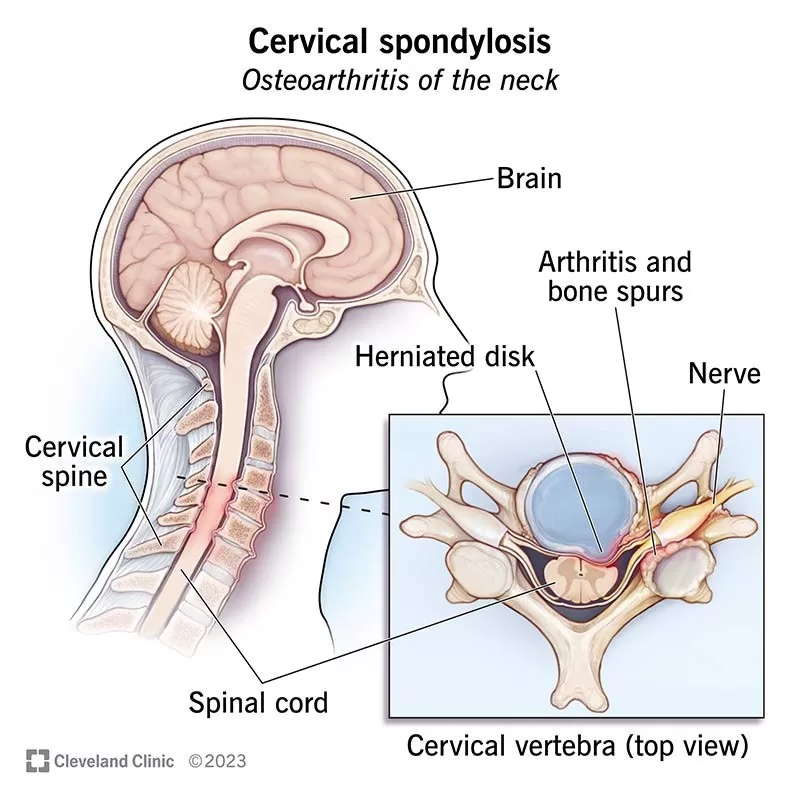
Cervical spondylosis is largely considered a wear-and-tear condition that develops as we age. This degenerative process results in the deterioration of the cervical spine’s structural integrity, characterized by changes such as bone spurs, disc thinning, and loss of flexibility. As age progresses beyond 40, risk factors including genetics, lifestyle, and prior injuries become increasingly significant contributors. Individuals with a history of neck trauma, rigidity, unaddressed postural anomalies, or certain occupations may experience accelerated degenerative changes.
Moreover, it is essential to link cervical spondylosis with systemic aging conditions. Factors such as obesity and sedentary lifestyles further exacerbate spinal health issues and can lead to conditions like myelopathy. Individuals must remain proactive about their cervical spine health by engaging in regular physical activity and maintaining a healthy weight, both of which can mitigate risk factors and support overall spinal functionality.
Symptoms of Cervical Spondylosis: Recognizing the Warning Signs
Recognizing the symptoms of cervical spondylosis early is crucial for effective intervention. Common clinical manifestations include chronic neck pain, localized stiffness, and potential radiating discomfort into the shoulders and arms. Patients may also encounter neurological symptoms such as tingling or numbness in the limbs—indicative of nerve compression, a frequent occurrence in cervical spondylosis cases. If left untreated, these symptoms may progress and lead to more significant issues like cervical myelopathy.
Myelopathy symptoms, arising from cervical spondylosis, can greatly affect an individual’s quality of life. Patients may notice weakened grip strength, difficulty performing tasks requiring fine motor skills, or imbalance while walking. In severe cases, dysfunction of bowel and bladder control can occur. Thus, monitoring for these symptoms and seeking timely medical evaluation is imperative for anyone over 40 or with known cervical issues.
Cervical Myelopathy Treatment: Options and Approaches
Treatment strategies for cervical myelopathy largely depend on the severity of symptoms and the underlying cause. Initially, non-surgical methods such as physical therapy and chiropractic care can be beneficial, helping to relieve pain and improve neck function. These conservative measures include guided exercises designed to enhance strength and flexibility in the cervical region while promoting ergonomic practices. Additionally, pain management may involve anti-inflammatory medications to help control discomfort.
However, for patients experiencing profound symptoms or progressive myelopathy, surgical options may become necessary. Surgical interventions include decompression techniques and spinal fusion, carefully tailored to the specific anatomical challenges faced by the patient. Advancements in surgical techniques have also introduced innovative procedures, such as artificial disc replacement, which allow for continued motion in the spine while alleviating compressive forces on the spinal cord.
Current Research Trends in Cervical Spine Health
Recent research in cervical spine health underscores the importance of timely diagnosis and the development of improved surgical techniques for cervical spondylotic myelopathy. Continued investigations into the efficacy of emerging treatments, such as cervical disc arthroplasty, reveal promising trends that prioritize patient mobility and recovery outcomes. This shift towards minimally invasive procedures aims to reduce rehabilitation times and improve post-operative satisfaction.
Furthermore, studies have shown that proactive management, focusing on preventive measures and patient education, plays a critical role in addressing cervical spine issues among aging populations. Initiatives aimed at raising awareness about effective spinal health preservation techniques can empower individuals to seek earlier treatment and ultimately enhance their life quality as they age.
The Growing Impact of Cervical Spondylosis in Aging Populations
The prevalence of cervical spondylosis is projected to rise as the global population ages, leading to increased healthcare burdens associated with spinal health issues. Healthcare systems must adapt to accommodate the growing number of individuals affected by cervical spondylotic conditions, emphasizing the development of multidisciplinary care strategies that incorporate physical therapists, neurosurgeons, and active lifestyle management.
In response to this increase, there is a call for increased research and funding toward innovative treatments and public health initiatives that focus on early detection and management of cervical spondylosis. Ensuring that older adults receive education about the symptoms and available therapies can significantly improve outcomes, allowing individuals to maintain their independence and mobility well into older age.
Frequently Asked Questions
What causes cervical spondylosis and how does it relate to aging?
Cervical spondylosis is primarily caused by age-related changes in the cervical spine, leading to degenerative conditions like osteoarthritis. As individuals age, the wear and tear on the cervical discs and vertebrae results in bone spurs and decreased disc elasticity, contributing to symptoms such as pain and stiffness.
How is cervical myelopathy diagnosed in patients with cervical spondylosis?
Diagnosing cervical myelopathy involves a clinical assessment of symptoms, a detailed medical history, and imaging studies such as MRIs. These help visualize spinal cord compression and assess neurological deficits associated with cervical spondylosis.
What are the common symptoms of cervical spondylosis and its progression to myelopathy?
Common symptoms of cervical spondylosis include neck pain, stiffness, and decreased range of motion. If progression to myelopathy occurs, symptoms may escalate to include weakness in the arms or legs, sensory disturbances, and gait dysfunction due to spinal cord compression.
What treatment options are available for cervical spondylotic myelopathy?
Treatment for cervical spondylotic myelopathy can range from non-surgical methods like physical therapy and pain management ( NSAIDs) to surgical interventions such as decompression surgery or cervical fusion, depending on the severity of symptoms and the degree of spinal cord compression.
How can aging impact spinal health and lead to cervical spondylosis?
Aging significantly impacts spinal health as degenerative changes, including loss of disc hydration and increased risk of osteoarthritis, lead to cervical spondylosis. This decline in cervical spine health can result in conditions such as myelopathy, highlighting the importance of early intervention and management.
| Key Point | Details |
|---|---|
| Cervical Spondylosis | A degenerative condition of the cervical spine, common in individuals over 40, characterized by age-related changes. |
| Causes | Includes osteoarthritis, previous neck injuries, genetic factors, and degeneration of intervertebral discs. |
| Myelopathy | A condition resulting from spinal cord compression, leading to significant neurological deficits. |
| Symptoms | Weakness, gait dysfunction, sensory disturbances, and possible bowel/bladder dysfunction. |
| Diagnosis | Involves clinical assessment, imaging (MRI), and neurological evaluations for compression identification. |
| Treatment Options | Includes non-surgical treatments (physical therapy, pain management) and surgical options (decompression, fusion, arthroplasty). |
| Research Trends | Focuses on improving surgical outcomes through timely interventions and exploring new surgical techniques. |
| Implications for Aging Populations | Increasing incidence of cervical spondylotic myelopathy, highlighting the need for effective management and education. |
Summary
Cervical spondylosis is a prevalent degenerative condition affecting many individuals as they age, particularly those over 40. It is crucial to understand the implications of this condition, especially its association with myelopathy, which can lead to severe neurological complications. Recognizing the symptoms and getting timely diagnosis and treatment plays a significant role in managing cervical spondylotic myelopathy effectively. As the aging population continues to grow, awareness and educational efforts surrounding cervical spondylosis will be vital in ensuring better health outcomes and maintaining quality of life.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.