Carotid endarterectomy (CEA) is a vital surgical intervention designed to reduce the risk of stroke by addressing stenosis—the narrowing of the carotid arteries that supply blood to the brain. With thousands impacted by stroke each year due to carotid artery diseases, this procedure plays a crucial role in stroke prevention. By effectively performing plaque removal, CEA not only restores blood flow but also significantly diminishes the chances of life-threatening ischemic strokes. Furthermore, this vascular surgery is continuously evolving thanks to recent medical advancements that enhance its safety and efficacy. Understanding CEA and its benefits is essential for anyone at risk, making knowledge in this area a vital part of health management.
Also known as carotid artery surgery, carotid endarterectomy is a procedure focused on alleviating stroke risk derived from carotid artery blockage. This intervention focuses on the surgical removal of atherosclerotic plaque that can hinder blood flow and lead to severe cerebrovascular events. As we delve into the intricate details of vascular surgery, it is essential to recognize the critical role of such operations in stroke prevention. With ongoing medical advancements, patients can expect improved outcomes and better management of their artery health through effective interventions. Understanding these terms and procedures can empower individuals to actively participate in their vascular health journey.
Understanding Carotid Endarterectomy: Procedure Overview
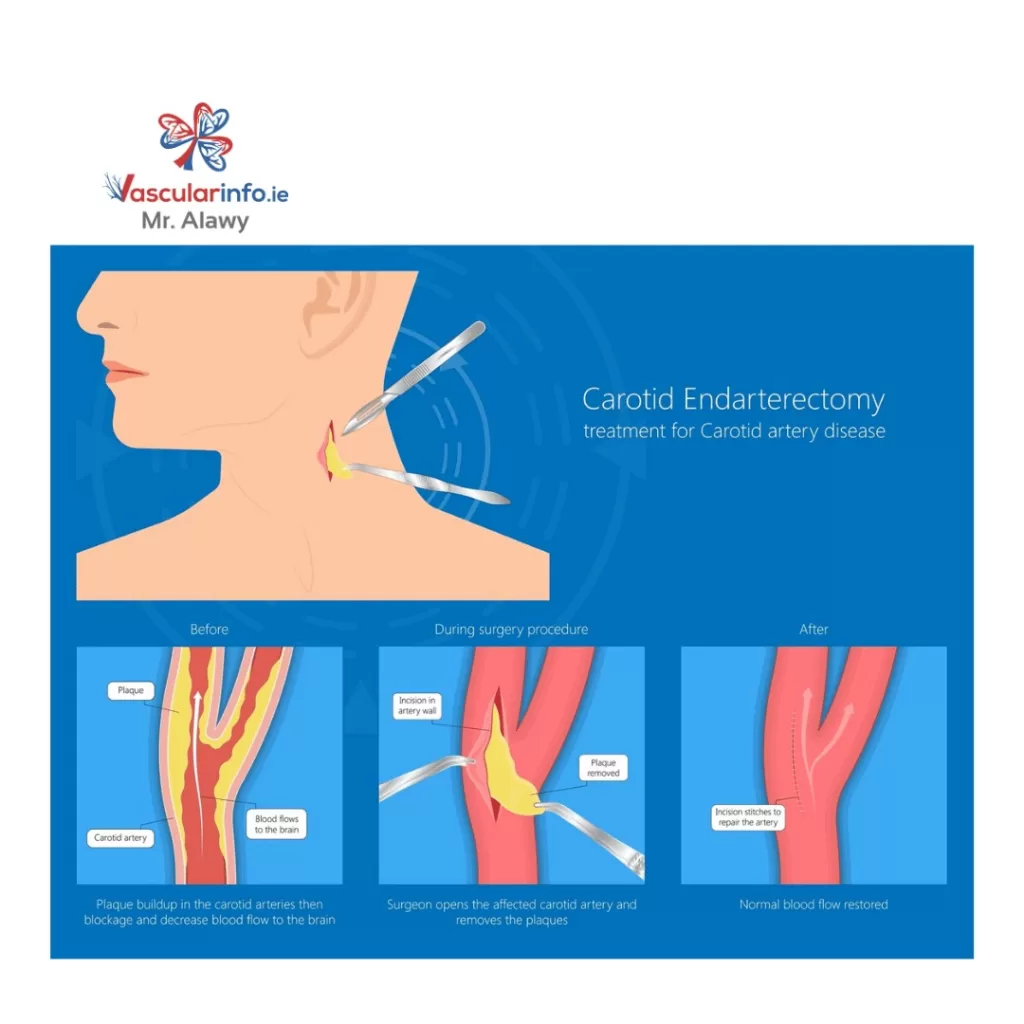
Carotid endarterectomy (CEA) is a vital surgical procedure aimed at reducing the risk of stroke by addressing stenosis, or narrowing, in the carotid arteries. This surgical intervention is performed under general anesthesia and involves making a small incision in the neck to access the affected carotid artery. After carefully clamping the artery, the surgeon removes the plaque buildup that is obstructing normal blood flow to the brain. Once the plaque removal is complete, the artery is stitched back together, allowing for improved circulation. This procedure is particularly critical for individuals showing signs of vascular diseases that could lead to life-threatening strokes.
The CEA procedure not only focuses on plaque removal but also aims to reinforce the health and longevity of the vascular system. Advanced techniques in vascular surgery, such as the use of intraoperative ultrasound, allow surgeons to visualize the artery in real-time, ensuring a thorough removal of all plaque and minimizing the risk of complications. Given the high stakes of effective stroke prevention, understanding the CEA procedure can empower patients with knowledge about their treatment options and the importance of timely surgical interventions.
Recent Innovations in Carotid Endarterectomy
In recent years, several medical advancements have transformed the landscape of carotid endarterectomy, enhancing both the efficacy and safety of the procedure. For instance, the implementation of sonolysis techniques is revolutionizing surgical approaches by utilizing high-frequency sound waves to dissolve clots. This innovative method has been shown to significantly decrease the incidence of cerebrovascular events like ischemic strokes shortly after surgery, thereby improving overall patient outcomes and ensuring safer recovery periods.
Furthermore, the use of intraoperative ultrasound, exemplified by the SONOBIRDIE study, represents a benchmark in surgical practice. This technology allows surgeons to actively monitor the operation, thereby increasing precision during plaque removal. By integrating these advanced techniques, vascular surgery can adapt to better meet the needs of patients while minimizing risks associated with traditional methods. Collectively, these innovations underscore the dynamic nature of CEA and its critical role in stroke prevention.
Patient Considerations for Carotid Endarterectomy
Identifying suitable candidates for carotid endarterectomy is crucial for optimizing patient care. Typically, candidates include individuals who exhibit significant narrowing of the carotid artery, demonstrated by imaging tests indicating over 60% stenosis. Additionally, those who have already experienced symptoms of stroke or transient ischemic attacks (TIAs) may benefit greatly from this surgical intervention. It is vital for healthcare providers to thoroughly assess the patient’s overall health and medical history before determining their eligibility for CEA.
Engaging in open discussions with healthcare professionals about the likelihood of stroke risk and the potential benefits of the procedure can empower patients to make informed decisions. Factors such as age, comorbidities, and lifestyle choices also play a significant role in candidate selection. Ultimately, understanding these patient considerations ensures that only those who would most benefit from carotid endarterectomy proceed with the surgery, leading to enhanced stroke prevention outcomes.
Potential Risks Associated with Carotid Endarterectomy
While carotid endarterectomy offers significant benefits in stroke prevention, it is essential to recognize the potential risks associated with this surgery. Among the most critical complications are the possibilities of stroke occurring either during or shortly after the procedure, as well as the risk of heart attack. Other complications may include infection at the surgical site or nerve damage, which could result in temporary or permanent weakness and numbness.
Patients must be well-informed about these risks, allowing them to weigh the potential benefits against the downsides of undergoing the surgery. A comprehensive pre-surgical consultation can help identify any underlying health issues that might increase the likelihood of complications, enabling a tailored and careful approach to each patient’s treatment plan. Education about recognizing warning signs and understanding post-operative care further empowers patients to manage their recovery effectively.
Recovery Strategies After Carotid Endarterectomy
Recovery from carotid endarterectomy is a crucial phase that helps ensure the long-term success of the procedure. Typically, patients will spend a few days in the hospital for monitoring after surgery to manage any potential complications that may arise. During this time, healthcare providers will assess the patient’s progress, manage pain, and initiate early rehabilitation strategies, which are essential for restoring normal function and mobility.
Once discharged, patients are encouraged to adhere to their prescribed medications and follow specific lifestyle changes to promote vascular health. Engaging in regular follow-up appointments is vital to monitor recovery and assess the status of the carotid arteries. By actively participating in their health decisions and adhering to the recommended recovery protocols, patients can significantly enhance their overall prognosis and reduce the risk of future cerebrovascular incidents.
Frequently Asked Questions
What is the purpose of Carotid Endarterectomy (CEA) in stroke prevention?
Carotid Endarterectomy (CEA) is a surgical procedure designed to prevent strokes by removing plaque buildup from narrowed carotid arteries. This procedure improves blood flow to the brain and significantly reduces the risk of ischemic strokes, making it a critical intervention in vascular surgery.
Who is considered a candidate for Carotid Endarterectomy?
Candidates for Carotid Endarterectomy typically include individuals who have significant carotid artery stenosis (over 60%), have experienced symptoms like strokes or transient ischemic attacks (TIAs), and are medically fit for surgery, ensuring the procedure can safely prevent further vascular complications.
What are the recent advancements in Carotid Endarterectomy techniques?
Recent advancements in Carotid Endarterectomy techniques include the use of intraoperative ultrasound to enhance surgical outcomes and the sonolysis technique, which utilizes sound waves to dissolve clots and improve patient recovery, reducing the risk of cerebrovascular events post-surgery.
What are the potential risks associated with Carotid Endarterectomy?
Potential risks of Carotid Endarterectomy include stroke during or after the procedure, heart attack, infection at the incision site, and nerve injury. Understanding these risks is crucial for patients considering this vascular surgery.
How does recovery from Carotid Endarterectomy impact a patient’s lifestyle?
Recovery from Carotid Endarterectomy typically involves a hospital stay for monitoring, with a return to normal activities expected within a few weeks. Patients are advised to adhere to prescribed medications and implement lifestyle changes to maintain vascular health and minimize future stroke risks.
| Key Points | Details |
|---|---|
| What is CEA? | Carotid endarterectomy (CEA) is a surgical procedure to remove plaque from the carotid artery to prevent strokes. |
| Recent Developments | 1. Ultrasound Enhancements – Intraoperative ultrasound improves safety and reduces complications. 2. Sonolysis Technique – Lowers occurrence of ischemic strokes using sound waves to dissolve clots. 3. Pharmacologic Agents – Anticoagulants like heparin are crucial for minimizing thromboembolic risks during surgery. 4. Diagnostic Ultrasound – Non-invasive imaging for assessing carotid stenosis before and after surgery. |
| Candidate Criteria | Candidates must have significant carotid artery narrowing (usually over 60% stenosis), prior symptoms like strokes or TIAs, and be healthy enough for surgery. |
| Risks and Complications | Risks include stroke, heart attack, infection, and nerve injury. |
| Recovery | Hospital stay for monitoring; normal activities resumed in weeks, with follow-ups for rehabilitation. |
Summary
Carotid Endarterectomy is a vital surgical intervention aimed at preventing strokes caused by carotid artery disease. This procedure involves removing plaque from narrowed carotid arteries to enhance blood flow to the brain, thus significantly reducing the risk of ischemic strokes. As advancements in medical technology continue to enhance the effectiveness and safety of carotid endarterectomy, patients are better equipped to make informed decisions about their vascular health. By understanding the procedure, including potential risks and recovery processes, individuals can collaborate effectively with their healthcare providers to achieve optimal results and a healthier life.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.