Autoimmune disease misdiagnosis remains a pressing concern in the healthcare landscape, as countless individuals grapple with the consequences of delayed or incorrect diagnoses. Autoimmune diseases, such as lupus and vasculitis, often present a complex array of symptoms that can easily be mistaken for psychiatric conditions, leading to a dangerous cycle of misdiagnosis. The ramifications of these misdiagnoses can extend beyond physical health, negatively impacting mental well-being and leading to feelings of inadequacy and distrust in medical professionals. Research has shown that misdiagnosis consequences can leave lasting scars, not just on health, but also on patients’ self-esteem and overall quality of life. As clinicians and patients navigate this intricate relationship, it is essential to raise awareness about the mental health impact of misdiagnosis, emphasizing the need for comprehensive evaluations that prioritize both physical and psychological health.
The diagnosis of chronic autoimmune conditions can be as intricate as it is critical, with many patients facing challenges when their conditions are mistakenly attributed to psychological or psychosomatic disorders. This phenomenon of mislabeling leads to confusion and exacerbates the suffering of individuals who are living with systemic autoimmune diseases. Often, patients experience overlapping symptoms that may mimic mental health disorders, complicating the diagnostic landscape and creating a need for greater awareness among healthcare providers. Understanding the nuances of these conditions and recognizing the potential for mental health implications can transform the patient experience. As such, a holistic approach to diagnosis and treatment is vital to ensure that patients receive not just the right medical care, but also the empathy and understanding they deserve.
Understanding Autoimmune Disease Misdiagnosis
Autoimmune disease misdiagnosis is a critical issue that adversely affects many individuals suffering from systemic autoimmune rheumatic diseases (SARDs). Common conditions such as lupus and vasculitis are particularly prone to misdiagnosis, often being mistaken for psychiatric ailments due to their overlapping symptoms. This oversight can lead to devastating consequences for patients, who may endure unnecessary suffering and deterioration of their health while healthcare practitioners focus on mental health rather than exploring potential autoimmune origins.
The misdiagnosis of autoimmune diseases can create a significant rift between patients and healthcare providers. With autoimmune disease presentations mimicking psychological disorders, it is crucial for clinicians to have a broad understanding of both physical and mental health aspects. Dismissing symptoms as purely psychosomatic can further alienate patients, eroding trust and encouraging them to withdraw from seeking necessary medical assistance. As highlighted by researchers, understanding the nuances of autoimmune diseases is essential for clinicians to avoid the common pitfalls of misdiagnosis.
Consequences of Misdiagnosis in Autoimmune Disorders
The consequences of misdiagnosis for patients with autoimmune disorders are far-reaching and often traumatic. Patients commonly experience an increased sense of hopelessness and a decline in mental well-being when their legitimate physical ailments are attributed incorrectly to psychological sources. This misinterpretation can lead to unnecessary treatments for imagined conditions, further compromising their physical health and exacerbating emotional distress. Consequently, individuals may develop a chronic distrust in medical systems, making them less likely to seek help in the future.
Moreover, being misdiagnosed can result in protracted periods of suffering without effective treatment. Patients who fall victim to such diagnostic errors may endure years of anguish while their autoimmune conditions progress untreated. The significant emotional toll, including heightened anxiety and depression, can lead to a vicious cycle where the effects of misdiagnosis perpetuate a patient’s existing mental health challenges. This compounding impact emphasizes the need for improved diagnostic frameworks that recognize the complexities of autoimmune diseases and their overlapping symptoms.
Psychosomatic Misdiagnosis and Its Mental Health Ramifications
Mislabeling autoimmune conditions as psychosomatic can have severe ramifications for patients’ mental health. When doctors attribute symptoms to psychological causes, patients may internalize these messages, damaging their self-esteem and sense of agency. Comments suggesting ‘it’s all in your head’ can invalidate their suffering, leading to loneliness and despair as they struggle to demonstrate the physical reality of their conditions. Such experiences of being dismissed often lead to heightened anxiety and a mistrust of healthcare providers.
Furthermore, the cycle of misdiagnosis can foster a sense of mental health stigma, particularly when patients are branded with wrong psychiatric diagnoses. As they grapple with the psychological effects of misdiagnosis, many find themselves wondering if their experiences and feelings are legitimate. This questioning can manifest in chronic emotional distress, compounding the challenges faced by those already suffering from complex autoimmune disorders.
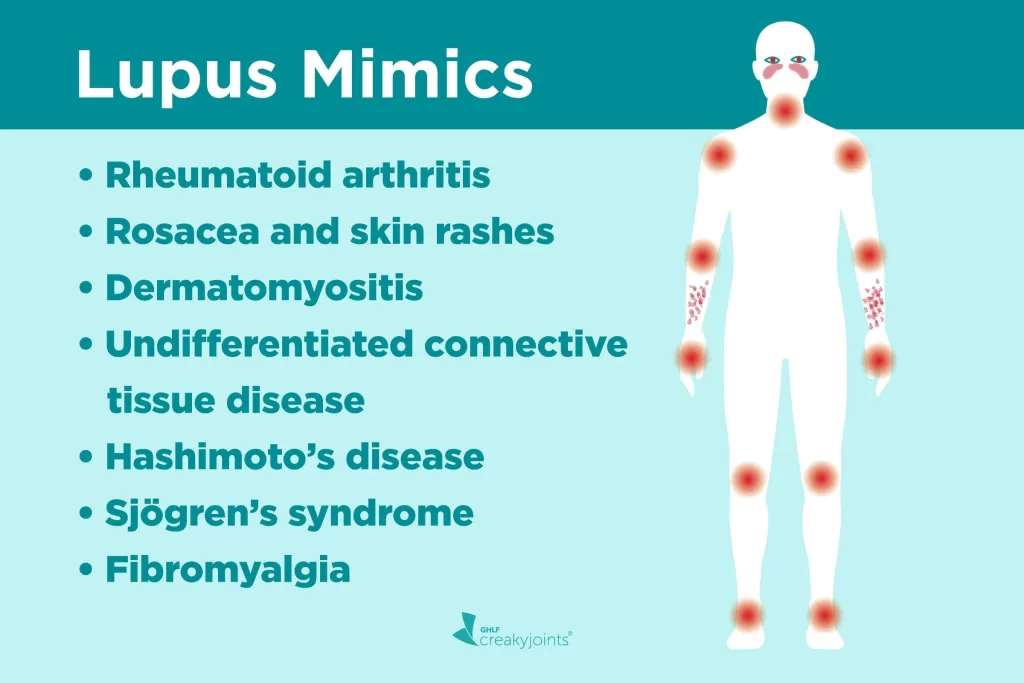
A Closer Look at Lupus Misdiagnosis
Lupus misdiagnosis is a particularly troubling aspect of autoimmune disease management, as it can significantly delay crucial treatment. Many patients with lupus initially present with nonspecific symptoms that lend themselves to misinterpretation as psychological or psychosomatic issues. As a result, they may undergo years of misdiagnosis involving incorrect treatments for conditions like depression or chronic fatigue syndrome, rather than receiving timely interventions for lupus.
The implications of lupus misdiagnosis extend beyond immediate physical health concerns. Patients report feelings of frustration and despair after years of navigating a fragmented healthcare system that failed to recognize the underlying autoimmune condition. By highlighting these realities, healthcare professionals can begin to shift their perspectives, ensuring lupus and other autoimmune diseases are prioritized in diagnostic assessments, regardless of initial presentations.
The Role of Trust in Healthcare Relationships
Trust is foundational to the patient-clinician relationship, especially for those navigating chronic illnesses like autoimmune diseases. Misdiagnosis can severely undermine this trust, leading patients to feel misunderstood and neglected by the healthcare system. Consequently, patients may become increasingly reluctant to share symptoms or seek medical attention, fearing dismissal and further misinterpretation of their conditions. Building a trusting rapport becomes essential for effective diagnosis and treatment.
To restore and maintain trust, healthcare providers must engage in active listening and validate their patients’ experiences. Acknowledging the complexities of autoimmune symptoms and ensuring clear communication can significantly enhance the patient experience. This collaborative approach fosters an environment where patients feel heard and respected, which is vital to improving adherence to treatment plans and ultimately better health outcomes.
Navigating the Diagnostic Challenge of Autoimmune Diseases
Diagnosing autoimmune diseases presents unique challenges, often requiring specialty knowledge and consideration of rare symptoms. Clinicians must be diligent in evaluating a comprehensive range of symptoms and potential overlaps with psychosomatic presentations. This diagnostic complexity is particularly relevant in illnesses characterized by diverse manifestations, such as Systemic Lupus Erythematosus and other SARDs. The failure to accurately diagnose can lead to mismanagement and prolonged patient suffering.
To combat the diagnostic challenge, intensified training and awareness for healthcare professionals about the multifaceted nature of autoimmune diseases are crucial. Emphasizing the early identification of autoimmune conditions, even in seemingly unrelated symptoms, can reduce instances of misdiagnosis. Encouraging a multidisciplinary approach—including rheumatologists, mental health specialists, and primary care physicians—can facilitate more accurate assessments and timely interventions.
The Psychological Impact of Autoimmune Misdiagnoses
The psychological impact of autoimmune disease misdiagnosis cannot be understated. Patients who experience misdiagnosis often undergo severe emotional turmoil, questioning the validity of their symptoms and their self-worth. This mislabeling as psychosomatic can lead to an overwhelming sense of isolation and despair, which is compounded by the inadequate understanding of their physical health needs. Recognizing and addressing these mental health challenges is vital to improve overall patient care.
Additionally, misdiagnosis can lead to significant increases in anxiety and depression rates among patients. The disconnect between a person’s lived experiences and the diagnosis received can foster feelings of disempowerment and frustration. It is essential for healthcare providers to be attuned to these profound effects, approaching each patient as a whole and recognizing the psychological aspects of their suffering along with their physical health needs.
Breaking the Cycle of Autoimmune Misdiagnosis
Breaking the cycle of autoimmune misdiagnosis requires a systemic shift in how healthcare providers approach patient evaluations. This involves thorough training that emphasizes the potential overlap between autoimmune and psychological symptoms, ensuring that clinicians maintain an open mind when assessing complex cases. By employing a more integrative approach, healthcare professionals can improve the accuracy of their diagnoses and subsequently, the quality of care provided.
Engaging patients in their diagnostic process is another crucial step. Patients should be encouraged to advocate for their health and voice any concerns regarding possible misdiagnosis. By fostering an environment where patients feel empowered, clinicians can better understand the full scope of the patient’s experiences and create tailored treatment approaches that address both physical and mental health needs.
Recommendations for Improving Diagnostic Accuracy
Improving diagnostic accuracy for autoimmune diseases mandates a multifaceted approach involving enhanced education and awareness among healthcare practitioners. This includes adopting new assessment protocols that value patient feedback and symptom reports, focusing on the historical presentation of symptoms over time. Employing validated assessment tools can help clinicians bridge the gaps in understanding autoimmune presentations and their psychosomatic counterparts.
Furthermore, fostering interdisciplinary collaboration amongst healthcare teams can cultivate a more comprehensive understanding of autoimmune conditions. Regular case discussions and training sessions can prepare teams to recognize and assess the possibility of autoimmune diseases, even in the presence of psychological symptoms. Encouraging open communication among specialists will contribute to a more integrated approach to diagnosing and treating autoimmune patients.
Frequently Asked Questions
What are the consequences of autoimmune disease misdiagnosis?
Autoimmune disease misdiagnosis can lead to significant long-term harm, affecting both physical and mental health. Incorrectly attributing symptoms to psychological causes can result in inadequate treatment and increased depression and anxiety in patients. Trust in healthcare systems may erode, leading patients to avoid seeking care, and worsening their overall well-being.
How does mental health impact the diagnosis of autoimmune diseases?
Mental health issues often complicate the diagnosis of autoimmune diseases. Symptoms such as depression and anxiety may emerge before clear autoimmune indicators, leading to misdiagnoses as psychiatric disorders. This overlap not only hampers accurate diagnoses but can also exacerbate the patient’s mental health problems, creating a cycle of misinterpretation and mistreatment.
Why are conditions like lupus frequently misdiagnosed?
Conditions like lupus are often misdiagnosed due to their diverse symptomatology that can mimic psychiatric issues. Studies have shown that approximately 50% of lupus patients are misdiagnosed before receiving proper treatment. The complexity of symptoms and lack of awareness among clinicians about autoimmune manifestations can result in misdiagnosis as psychosomatic or psychological, delaying effective care.
What role does trust play in the healthcare experiences of those with autoimmune disease misdiagnosis?
Trust is crucial in healthcare, and autoimmune disease misdiagnosis can severely undermine it. Patients who experience dismissive comments or misdiagnoses may become distrustful of healthcare providers, leading them to minimize their symptoms and avoid seeking necessary treatment. This distrust can negatively impact their health outcomes and overall well-being.
Can psychosomatic misdiagnosis affect long-term mental health?
Yes, psychosomatic misdiagnosis can have lasting mental health effects. When patients are incorrectly told their symptoms are ‘all in their head,’ it can damage their self-worth and lead to chronic emotional distress. The negative impacts on mental health can persist for years, reinforcing feelings of anxiety and depression as patients struggle to receive valid diagnoses and care.
How can healthcare providers improve the diagnosis of autoimmune diseases?
Healthcare providers can enhance the diagnosis of autoimmune diseases by prioritizing patient history and symptoms, and avoiding premature psychiatric labels. Better education about the complex presentations of autoimmune diseases and encouraging open communication with patients can help to ensure timely and accurate diagnoses, minimizing the risk of misdiagnosis.
| Key Point | Details |
|---|---|
| Autoimmune Disease Misdiagnoses | Misdiagnosing autoimmune diseases can lead to serious long-term health issues, both physically and mentally. |
| Common Misdiagnoses | Conditions such as lupus and vasculitis are frequently misdiagnosed as psychiatric conditions. |
| Impact on Patients | Patients often experience a loss of self-worth and long-term mental health impacts after being dismissed. |
| Trust Issues with Healthcare | Misdiagnoses contribute to distrust in healthcare providers, leading to worse health outcomes. |
| Complexity of Diagnosis | Diagnosing autoimmune diseases is complicated due to overlapping symptoms with psychiatric conditions. |
| Clinician Awareness | Many clinicians underestimate the severity and long-term effects of misdiagnoses. |
| Call for Change | There is a need for healthcare providers to correct previous misdiagnoses and better recognize autoimmune conditions. |
Summary
Autoimmune disease misdiagnosis can lead to significant long-term effects on patients’ health and well-being. As highlighted by a recent study, the misunderstanding and miscommunication surrounding these diseases can result in dismissive attitudes from healthcare professionals, often attributing symptoms to psychological rather than autoimmune causes. This not only impacts patients’ physical health but also their mental health, leading to distrust in healthcare systems. The complexity of diagnosing autoimmune diseases requires a more nuanced understanding from clinicians to avoid perpetuating misdiagnoses that can harm patients for years.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.