Antimicrobial Stewardship is a critical component of modern healthcare, focusing on optimizing the use of antibiotics to combat healthcare-associated infections (HAIs) and prevent the rise of antibiotic-resistant bacteria. With increasing concerns regarding pathogens like Clostridium difficile and the impact of avian flu outbreaks, effective antimicrobial stewardship programs are more crucial than ever. They aim to ensure prescribed antibiotics are appropriate, thereby enhancing infection prevention efforts across various healthcare settings. This proactive approach not only safeguards patient health but also preserves the efficacy of existing antibiotics as vital therapeutic tools. As global health threats such as pandemic influenza loom, strengthening these stewardship initiatives becomes imperative for safeguarding public health.
The practice of responsible antibiotic management, often referred to as antimicrobial stewardship, is essential in controlling the proliferation of drug-resistant infections and enhancing overall patient safety. This approach involves coordinated actions aimed at optimizing the prescribing of antimicrobial medications, particularly in the context of healthcare-associated infections (HAIs). As evidenced by recent studies linking conditions like Clostridium difficile infections to improper antibiotic use, the need for effective strategies in infection control is paramount. Furthermore, initiatives addressing outbreaks related to avian influenza and pandemic influenza underscore the ongoing significance of improving infection prevention measures. By fostering a culture of responsible prescribing, antimicrobial stewardship not only combats the threat of resistance but also contributes to better health outcomes across diverse populations.
The Role of Antimicrobial Stewardship in Infection Control
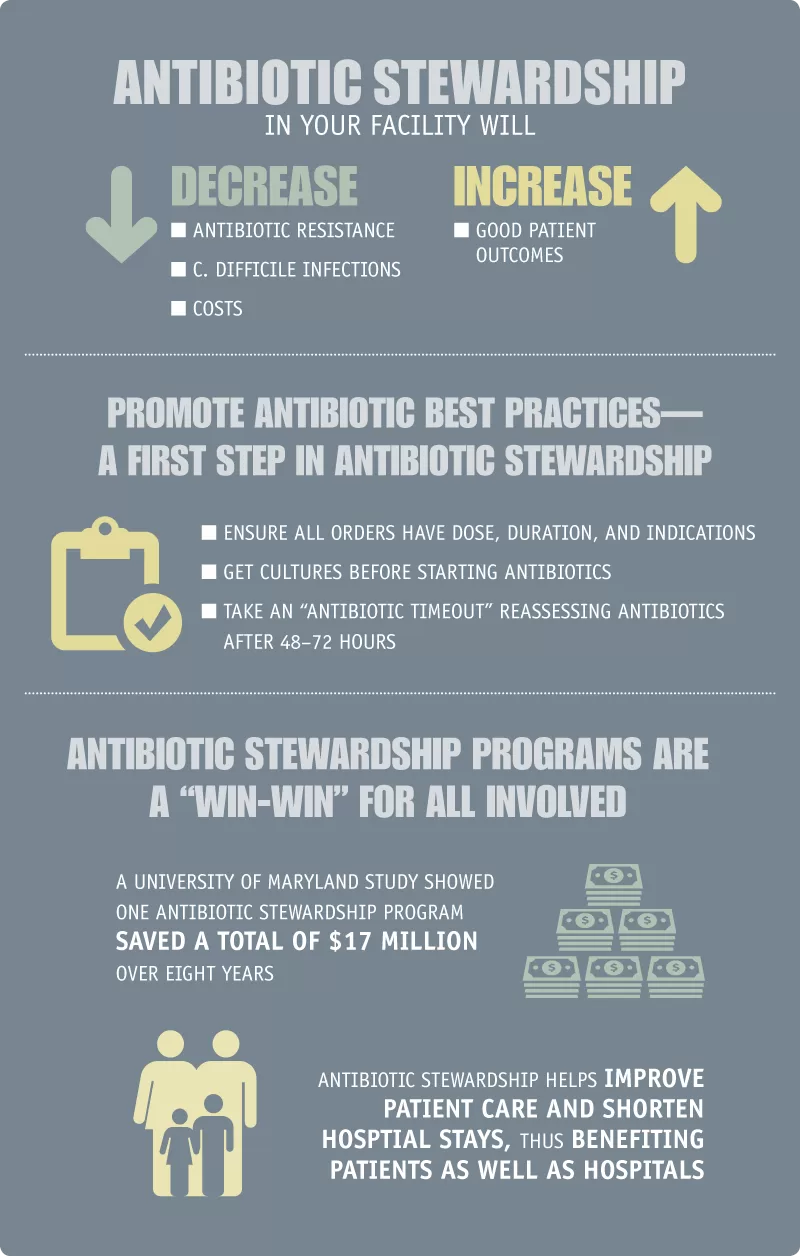
Antimicrobial stewardship plays a crucial role in the battle against healthcare-associated infections (HAIs). The inappropriate use of antibiotics has contributed significantly to the rise of antibiotic resistance, making infections harder to treat and leading to longer hospital stays, higher medical costs, and increased mortality. By implementing effective antimicrobial stewardship programs, healthcare facilities aim to optimize antibiotic use, ensuring that patients receive the right drug, at the right dose, for the right duration. These programs involve rigorous infection prevention practices that are essential in battling infections caused by resistant pathogens and also mitigate the emergence of Clostridium difficile infections, one of the serious consequences of antibiotic misuse.
Moreover, the partnership between organizations dedicated to genomic surveillance, like the Wellcome Sanger Institute and Stellenbosch University, reinforces the importance of antimicrobial stewardship in managing infectious diseases. By focusing on genomic data, these institutes can better track emerging infectious threats, including those that lead to HAIs, thereby informing stewardship efforts. This coordinated approach ensures that antibiotic use is guided by the latest insights into microbial resistance patterns and outbreak trends, ultimately contributing to more effective infection prevention strategies and reduced healthcare costs.
Recent Avian Flu Outbreaks and Public Health Responses
The recent outbreaks of avian influenza across several states in the US have raised significant public health concerns. These outbreaks highlight the interconnectedness of infectious disease management and the importance of robust surveillance. The swift response from authorities, including the U.S. Department of Agriculture, emphasizes infection prevention strategies to mitigate the risk to poultry and, consequently, human health. Continuous monitoring and rapid identification of avian flu cases are critical in preventing further spread, especially in areas with high poultry density. This situation underlines the need for thorough biosecurity measures and effective communication among health officials.
Public health departments are now actively engaging in infection prevention efforts which align closely with antimicrobial stewardship. By preventing infections at the source, health officials can significantly reduce the need for antibiotics in treating complications that may arise from avian flu exposure. In this context, stakeholder collaboration becomes crucial; the sharing of data and resources allows for a more coordinated response to mitigate the impacts of avian flu outbreaks. Furthermore, as we have seen during recent challenges, health officials must remain vigilant against antibiotic-resistant pathogens, especially when outbreaks occur in conjunction with antibiotic use for treating secondary infections related to primary viral infections like avian influenza.
Just as importantly, coordinated global surveillance efforts, such as those established between prominent research institutions, can aid in early detection and response to similar infectious threats. This partnership approach provides a model for managing future pandemics and influenza outbreaks through improved preparedness and collective action.
Understanding the transmission dynamics of avian flu and its potential impact on public health can inform vaccination strategies and biosecurity measures, ultimately reducing healthcare-associated infections caused by resistant strains of pathogens.
Impact of Clostridium difficile on Healthcare Costs
Clostridium difficile infections (CDI) present a significant challenge to the healthcare system, contributing to prolonged patient hospitalization and escalating treatment costs. Studies indicate that CDI is often associated with the overuse of antibiotics, exacerbating the condition through a cycle of infection and re-infection. The economic burden is not only felt by hospitals but also reflects in increased healthcare costs for patients and insurers. Targeted antimicrobial stewardship initiatives aim to curb the inappropriate prescription of antibiotics, thereby reducing the incidence of CDI and its associated complications. By focusing on better prescribing practices and incorporating education and awareness efforts, healthcare facilities can enforce protocols to minimize the risk of CDI stemming from antibiotic misuse.
Moreover, patient outcomes can be significantly improved through the collaborative efforts of infection prevention teams and antimicrobial stewardship programs. Comprehensive education concerning the risks associated with CDI, particularly the role of proton pump inhibitors and certain antibiotics, is vital for both healthcare providers and patients. As evidenced by studies, the combination of PPIs and antibiotics has been linked to heightened risks of CDI. Therefore, healthcare providers must approach treatment plans with caution, ensuring that the benefits outweigh the risks, particularly in vulnerable patient populations. Advancing our understanding of CDI, implementing best practices in antibiotic stewardship, and promoting effective infection prevention strategies are essential for reducing CDI prevalence and minimizing its impact on healthcare systems.
Healthcare-Associated Infections: The Need for Prevention
The prevalence of healthcare-associated infections (HAIs) remains a critical issue within the medical community. As per the CDC’s estimates, one in 31 patients acquires at least one HAI during their hospital stay, indicating a substantial risk that can lead to increased morbidity and mortality. Effective infection prevention practices are essential to combat HAIs, particularly in hospital settings where patients areoften exposed to antibiotic-resistant organisms. By implementing multifaceted strategies—including better hand hygiene, environmental cleaning, and the use of bundled interventions—healthcare facilities can significantly reduce the incidence of HAIs.
Moreover, the funding awarded by organizations such as the National Association of County and City Health Officials (NACCHO) to enhance antimicrobial stewardship and infection control is a step forward in addressing the issue. This funding allows local health departments to develop tailored approaches to minimize infections, assess their practices, and refine their strategies using evidence-based interventions. The two-fold strategy of bolstering infection prevention protocols while enhancing antimicrobial stewardship ensures a synergistic effect in reducing the burden of HAIs. Continuous education and collaboration among healthcare workers, combined with support from public health institutions, are essential for creating a culture that prioritizes safety and patient care.
Effectiveness of Genomic Surveillance in Infection Control
Genomic surveillance has emerged as a pivotal tool in infection control, offering unprecedented insights into the spread of infectious diseases. The collaboration between global institutions, such as the Wellcome Sanger Institute and Stellenbosch University, aims to enhance our understanding of pathogens through advanced genomic data. This partnership enables the identification of viral strains and resistance patterns, which is crucial for timely public health interventions. By tracking the evolution of pathogens, genomic surveillance can inform strategies for vaccination, treatment, and infection prevention.
Incorporating genomic data into public health practices can improve the management of outbreaks, reducing the potential for healthcare-associated infections and enhancing antimicrobial stewardship programs. As we face increasing challenges from antibiotic-resistant bacteria, the knowledge gained from genomic studies facilitates the development of targeted approaches to infection control. These actions can ultimately lead to better patient outcomes and reduced healthcare costs, underscoring the importance of investing in genomic surveillance as a critical component of public health strategy.
Challenges in Managing Pandemic Influenza
The ongoing threat of pandemic influenza necessitates robust public health frameworks capable of rapid response and effective management. Influenza viruses are notorious for their ability to mutate, leading to new strains that can evade existing immunity and vaccines. As we have witnessed during previous pandemic events, such as the H1N1 outbreak, early detection and controlled responses are essential in minimizing transmission and impact. Public health officials are now focusing not only on vaccination but also on integrated infection prevention measures that protect populations from severe influenza outbreaks.
Understanding the epidemiology of pandemic influenza also informs the development of treatment guidelines, particularly regarding the responsible use of antiviral therapies. During severe outbreaks, antimicrobial stewardship must encompass antiviral medications to avoid misuse and further resistance. Educational initiatives aim to equip healthcare professionals with the knowledge to distinguish viral infections from bacterial ones, enabling them to avoid unnecessary prescriptions and ensure that treatments are effective when truly warranted. The complexities of managing infections during pandemics underscore the need for a unified effort in surveillance, prevention, and treatment that prioritizes public health safety.
Healthcare Settings: Reducing Infection Risks Through Research
Research plays a transformative role in enhancing infection control practices within healthcare settings. Recent studies underscore the importance of understanding the dynamics of pathogens, especially concerning healthcare-associated infections (HAIs) and their relation to antibiotic use. Through systematic investigations, healthcare professionals can identify specific risk factors associated with different pathogens, such as Clostridium difficile, and implement evidence-based interventions that significantly reduce infection rates.
The ongoing dialogue regarding the impact of infection prevention strategies on healthcare settings has also spurred interest in examining how genomic data can contribute to more informed decision-making. Collaboration between researchers and healthcare practitioners enables the translation of findings into practical applications that mitigate infection risks. As facilities continue to adapt their protocols based on emerging research, the commitment to improving patient safety through infection control remains a top priority in healthcare.
Importance of Infection Prevention Training in Hospitals
Infection prevention training is a critical component of healthcare quality that directly influences patient outcomes. As the burden of healthcare-associated infections continues to rise, hospitals are investing in comprehensive training programs for staff, focusing on best practices for infection prevention. Such training encompasses hand hygiene, proper use of personal protective equipment, and understanding the transmission dynamics of various pathogens. When healthcare workers are well-versed in infection control methods, they can significantly reduce the risk of pathogen spread within hospital settings.
Additionally, hospitals must recognize the importance of continual education as new research brings forth novel insights into infection risks. Training programs should evolve in response to emerging threats, such as avian flu or resistant strains of bacteria, to ensure that healthcare professionals are prepared to manage these risks effectively. By fostering a culture of safety and awareness, hospitals can not only reduce HAIs but also enhance overall patient care and trust in healthcare systems.
The Impact of Hand Hygiene on Infection Rates
Hand hygiene is one of the most effective methods for preventing healthcare-associated infections and mitigating the spread of resistant pathogens. Studies have consistently shown that proper handwashing techniques can reduce the transmission of infectious agents in healthcare settings, yet compliance among healthcare workers often remains suboptimal. By prioritizing hand hygiene training and making it an integral part of everyday practice, healthcare institutions can foster a culture that emphasizes its significance. This is particularly crucial in preventing infections linked to antibiotic use, as better hygiene practices can minimize the need for antibiotics and the risk of subsequent infections like Clostridium difficile.
Moreover, leveraging technology to promote hand hygiene compliance can further enhance infection prevention efforts. Implementing electronic monitoring systems provides real-time feedback to healthcare workers regarding their hand hygiene habits. Coupled with educational initiatives, these practices can create an environment where infection control is a shared responsibility. By strengthening the commitment to hand hygiene, healthcare facilities can effectively combat the rising challenge of HAIs and prioritize patient safety.
Frequently Asked Questions
How does antimicrobial stewardship relate to healthcare-associated infections?
Antimicrobial stewardship is a critical practice in healthcare aiming to optimize the use of antibiotics to combat healthcare-associated infections (HAIs). By responsibly prescribing antibiotics, healthcare providers can reduce the incidence of HAIs caused by antibiotic-resistant pathogens, ultimately enhancing patient safety and health outcomes.
What role does antimicrobial stewardship play in preventing Clostridium difficile infections?
Antimicrobial stewardship plays a vital role in preventing Clostridium difficile infections (CDI) by promoting the judicious use of antibiotics. By minimizing unnecessary antibiotic prescriptions, healthcare providers can decrease the risk of CDI, as antibiotic therapy is a major risk factor for developing this infection.
Why is antimicrobial stewardship important during avian flu outbreaks?
During avian flu outbreaks, antimicrobial stewardship is essential to ensure that antibiotics are used appropriately and judiciously. Misuse of antibiotics can lead to increased antibiotic resistance, complicating treatment options for bacterial infections that may arise in poultry or potentially transition to humans.
How does pandemic influenza highlight the need for antimicrobial stewardship?
Pandemic influenza raises awareness of the importance of antimicrobial stewardship as it emphasizes the need for effective infection prevention strategies. During pandemic situations, there may be increased antibiotic use, which can contribute to antibiotic resistance, making stewardship efforts crucial in safeguarding public health.
What are the benefits of implementing antimicrobial stewardship programs in healthcare settings?
Implementing antimicrobial stewardship programs in healthcare settings leads to the reduction of healthcare-associated infections (HAIs), improved patient outcomes, and decreased healthcare costs associated with the treatment of antibiotic-resistant infections. These programs ensure that antibiotics are prescribed only when necessary and in the correct dosages.
How can healthcare facilities improve antimicrobial stewardship to reduce infection risks?
Healthcare facilities can improve antimicrobial stewardship by conducting regular audits of antibiotic prescriptions, providing education and training for healthcare staff, and implementing evidence-based guidelines for antibiotic use. This proactive approach helps to minimize the risk of infections, including Clostridium difficile and other HAIs.
What challenges do antimicrobial stewardship programs face in combating healthcare-associated infections?
Challenges faced by antimicrobial stewardship programs in combating healthcare-associated infections (HAIs) include the prevalence of antibiotic resistance, variations in antibiotic prescribing practices, and the need for ongoing education among healthcare professionals regarding best practices in antibiotic use.
Can antimicrobial stewardship impact the management of infections in pandemic influenza scenarios?
Yes, antimicrobial stewardship can significantly impact the management of infections in pandemic influenza scenarios by ensuring that antibiotics are reserved for bacterial superinfections rather than viral infections, which helps to preserve the effectiveness of existing antibiotics and mitigate the rise of antibiotic resistance.
| Topic | Details |
|---|---|
| Genomic Surveillance Partnership | Collaboration between Wellcome Sanger Institute and Stellenbosch University to enhance global genomic tracking of infectious diseases. |
| Antimicrobial Stewardship Funding | NACCHO announced $1.29 million funding to improve infection control and antimicrobial stewardship in local health departments across 11 states. |
| Avian Influenza Outbreaks | Increased avian flu outbreaks reported in California, Kansas, South Carolina, and South Dakota with commercial poultry farms affected. |
| Measles Alert | CDC warns of rising measles cases, urging vigilance among healthcare providers due to recent importations. |
| Clostridium Difficile Risk | Study links recent use of antibiotics and PPIs to increased risk of CDI, highlighting the necessity for careful prescription practices. |
| Global Flu Activity | Overall flu activity is declining globally, although certain regions report increases in detections. |
| Childhood Obesity Post-COVID | Research shows significant increase in preschool obesity rates in the UK during the COVID-19 pandemic. |
| Toilet Hygiene and Viral Spread | Research suggests closing toilet lids does not prevent viral contamination, emphasizing the importance of regular disinfection. |
Summary
Antimicrobial Stewardship is critical in the fight against antibiotic resistance and healthcare-associated infections. The recent collaboration between public health organizations to enhance infection prevention efforts and the funding initiatives highlight the ongoing commitment to improving healthcare outcomes. Ensuring effective antimicrobial stewardship not only benefits public health but serves as a proactive step in managing and preventing outbreaks of antibiotic-resistant pathogens.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.