Antifungal resistance is an escalating concern in the realm of infectious diseases, particularly in relation to Candida bloodstream infections (BSIs) or candidemia. With a rising prevalence of nonsusceptible Candida strains reported in various studies, it is crucial to address the link between recent antifungal exposure and these resistant infections. In South Africa alone, nearly half of the documented candidemia cases involve nonsusceptible species, with prior antifungal use being a contributing factor. This highlights the urgent need for effective antifungal stewardship strategies to combat this pressing issue and improve patient outcomes. Understanding the patterns and implications of antifungal resistance is pivotal for health professionals tackling the complexities of Candida infections on a global scale.
Addressing the challenges posed by resistance to antifungal medications has become increasingly vital, especially concerning serious fungal infections caused by Candida species. Commonly referred to as persistent Candida infections, these ailments not only complicate treatment but also show alarming trends of resistance among non-albicans strains, such as C. auris. Recent analyses point towards the significant correlation between antifungal treatment history and the occurrence of resistant bloodstream infections, emphasizing the role of previous drug exposure. As cases of candidemia continue to surge in regions like South Africa, the implementation of robust antifungal stewardship initiatives is essential to prevent further escalation of this health crisis. By exploring the underlying causes of antifungal resistance, we can equip healthcare systems with effective strategies to manage and control these infections.
Understanding Nonsusceptible Candida: A Growing Concern
Nonsusceptible Candida strains have emerged as a pivotal challenge in the management of candidemia, particularly in hospitalized patients. As observed in South Africa, the prevalence of these resistant strains underscores the need for urgent action in antifungal treatment protocols. The data indicates that a significant percentage of candidemia cases are linked to nonsusceptible species, which complicates treatment options and contributes to higher morbidity and mortality rates among affected patients.
The factors contributing to this rise in nonsusceptibility include prior systemic antifungal exposure, particularly to fluconazole, as evidenced by the study’s findings. The correlation is stark: patients with recent antifungal treatment have an increased likelihood of harboring nonsusceptible strains of Candida, emphasizing the importance of strategic antifungal stewardship programs to mitigate this risk. Understanding these dynamics is critical for healthcare providers to implement effective treatment and prevention strategies.
Impact of Antifungal Stewardship on Candida Bloodstream Infections
Antifungal stewardship is a proactive approach aimed at optimizing antifungal use, minimizing resistance development, and improving patient outcomes. In the context of Candida bloodstream infections, implementing robust stewardship protocols can significantly reduce the incidence of nonsusceptible species. This is especially crucial given the rising rates of candidemia linked to previous antifungal exposure, which necessitate careful prescribing practices and monitoring of antifungal efficacy.
In South Africa, the findings from the study highlight a critical opportunity for healthcare institutions to reevaluate their antifungal treatment regimens. By incorporating antifungal stewardship initiatives, hospitals can not only lower the rates of infection but also enhance overall patient safety. Continuous education for healthcare staff about the implications of antifungal resistance and the importance of judicious antifungal use is essential to address this public health challenge.
The Epidemiological Shift: Increasing Nonsusceptible Candida Strains
The epidemiological landscape of Candida infections has notably shifted in recent years, with non-albicans strains such as C. auris gaining prevalence. This transition presents a formidable challenge for clinicians, who must adapt their treatment strategies to contend with these evolving pathogens. In South Africa, the study period from 2012 to 2017 reveals a disturbing trend: the increasing incidence of nonsusceptible Candida strains poses risks not just to individual patients but to public health as a whole.
Understanding the epidemiology behind these changes is vital for developing effective interventions. The association between prior antifungal exposure and the emergence of nonsusceptible strains serves as a crucial insight for public health stakeholders. Ongoing surveillance and research are necessary to track these trends and inform targeted prevention measures that address both antifungal resistance and infection control.
Clinical Implications of Antifungal Resistance in Candidemia
Clinically, antifungal resistance in Candida bloodstream infections has profound implications for patient management. When faced with nonsusceptible strains, clinicians may encounter treatment failures, prolonged hospital stays, and increased healthcare costs. Moreover, the high mortality rates associated with untreated or poorly managed candidemia underscore the importance of early detection and targeted therapy, which can be complicated by the presence of resistant species.
The study highlights that patients with a history of antifungal exposure are at higher risk of developing nonsusceptible strains. Therefore, clinicians must thoroughly assess the antifungal history of their patients to guide therapy choices effectively. The integration of rapid diagnostics to identify resistance patterns in Candida species could lead to more personalized treatment plans and better outcomes.
Infection Control Strategies to Combat Antifungal Resistance
To combat the rising tide of antifungal resistance, robust infection control strategies must be employed alongside antifungal stewardship initiatives. In hospital settings, effective hygiene practices, routine screening for candidemia, and strict protocols for the use of antifungal medications are essential components of a comprehensive approach to infection prevention. Such strategies help mitigate the risk of transmission of nonsusceptible Candida strains among patients, particularly in high-risk populations.
Enhanced surveillance systems should be established to monitor the prevalence of antifungal resistance in different regions, especially in areas like South Africa where the burden of candidemia is significant. By implementing timely infection control measures, healthcare facilities can reduce the incidence of nosocomial infections and protect vulnerable patients from the devastating effects of antifungal-resistant Candida.
Antifungal Exposure and Its Role in Candidemia Among Different Age Groups
The impact of prior antifungal exposure on candidemia differs significantly across age groups, highlighting the need for tailored interventions. In the study, a notable association was found between antifungal treatment and nonsusceptibility in older patients, whereas neonates and young infants did not exhibit the same correlation. This suggests that, in younger populations, other factors such as hospital transmission dynamics may play a more critical role in the incidence of candidemia.
Healthcare providers must recognize these differences when developing prevention strategies for candidemia. For older patients, minimizing unnecessary antifungal exposure can be crucial in preventing the emergence of nonsusceptible strains. Conversely, pediatric care requires a distinct focus on infection transmission pathways to effectively manage and prevent Candida infections in vulnerable infants.
The Need for Enhanced Research on Antifungal Resistance
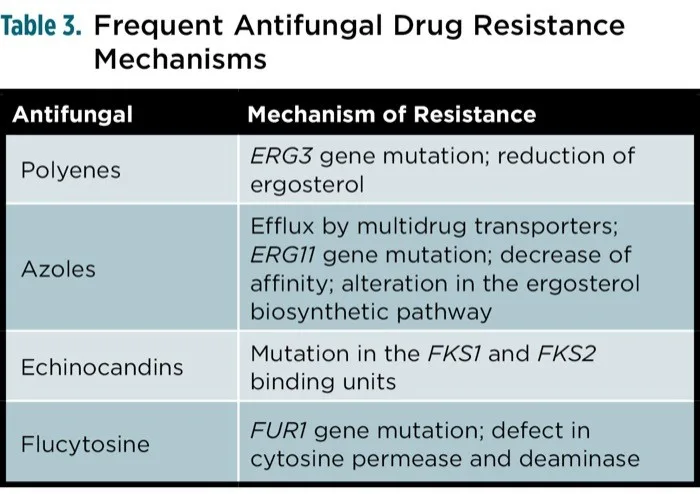
The ongoing challenge of antifungal resistance necessitates further research to understand the mechanisms driving nonsusceptibility in Candida species. Comprehensive studies that explore genetic, environmental, and treatment-related factors can help elucidate the reasons behind the rising rates of resistant infections. Additionally, research focusing on the comparison of different antifungal agents’ effectiveness against nonsusceptible strains is vital for optimizing treatment protocols.
In South Africa and globally, investing in antifungal resistance research is essential not only for improving clinical outcomes but also for shaping public health policies. As the landscape of fungal infections evolves, ongoing research will provide the foundation needed to inform clinicians and healthcare systems on best practices for managing candidemia and ensuring effective antifungal therapies.
Long-term Outcomes of Antifungal Resistance in Healthcare Settings
The long-term outcomes of antifungal resistance in healthcare settings extend beyond immediate clinical implications; they also encompass broader public health concerns. Rising rates of nonsusceptible Candida infections threaten the efficacy of current antifungal therapies and set a concerning precedent for future patient care. The implications of prolonged and more intensive treatments often magnify healthcare costs and resource utilization, leading to increased strain on healthcare systems.
Furthermore, the increased mortality associated with resistant infections may have lasting effects on population health metrics and quality of care. Therefore, addressing antifungal resistance should be a priority for healthcare policymakers and providers alike, ensuring that adequate resources are allocated to research, prevention, and treatment strategies that can safeguard against these emerging threats.
Global Perspectives on Antifungal Resistance and Candidemia
Antifungal resistance is not solely a localized issue but a global concern that transcends borders and impacts healthcare systems worldwide. The emergence of nonsusceptible Candida strains highlights the interconnected nature of public health and the need for a coordinated global response. International collaborations aimed at tracking resistance patterns and sharing best practices can significantly contribute to combating antifungal resistance.
In aligning global efforts, regional studies such as those conducted in South Africa can provide valuable insights into local epidemiology and resistance trends. By fostering a collective understanding of antifungal resistance through global data sharing, healthcare professionals worldwide can better equip themselves to address this pressing challenge in infectious disease management.
Frequently Asked Questions
What is antifungal resistance and why is it a concern in Candida bloodstream infections?
Antifungal resistance refers to the ability of fungi, like nonsusceptible Candida species, to withstand treatment with antifungal medications. This is a growing concern in Candida bloodstream infections (candidemia) as it complicates treatment options and is associated with increased mortality rates. In South Africa, studies have shown a significant rise in nonsusceptible Candida infections, emphasizing the urgent need for effective antifungal stewardship.
How does recent antifungal exposure affect nonsusceptible Candida infections in South Africa?
Recent studies in South Africa indicate that prior systemic antifungal exposure, especially to fluconazole, increases the risk of nonsusceptible Candida infections among hospitalized patients. Approximately 20% of patients with candidemia had this history, with 48% of cases linked to resistant strains. This highlights the critical impact of antifungal usage on resistance development and underscores the need for enhanced antifungal stewardship.
What role does antifungal stewardship play in managing the risk of antifungal resistance in Candida bloodstream infections?
Antifungal stewardship involves implementing strategies to optimize antifungal use and minimize resistance in pathogens like nonsusceptible Candida. By carefully monitoring antifungal prescriptions and promoting appropriate usage, particularly in at-risk populations, healthcare facilities in South Africa can mitigate the emergence of antifungal resistance and improve patient outcomes in candidemia.
Why are older patients more affected by nonsusceptible Candida bloodstream infections?
Research has shown that older patients, particularly those over 90 days old, exhibit higher rates of nonsusceptible Candida bloodstream infections. This correlates with recent antifungal exposure and possibly other underlying health conditions. In contrast, younger patients, such as neonates, may be affected by different transmission dynamics, suggesting that tailored approaches in infection control are necessary.
What measures can be taken to improve infection prevention regarding antifungal resistance in South Africa?
To enhance infection prevention relating to antifungal resistance in South Africa, it’s essential to implement strict antifungal stewardship protocols, improve surveillance of candidemia cases, educate healthcare providers on appropriate antifungal use, and adopt comprehensive infection control practices in healthcare settings. These measures can help limit the spread of nonsusceptible Candida species.
| Key Points | Details |
|---|---|
| Study Purpose | To examine the impact of prior antifungal exposure on nonsusceptible Candida bloodstream infections (BSIs) in hospitalized patients in South Africa from 2012 to 2017. |
| Study Findings | Approximately 48% of the candidemia cases were due to nonsusceptible Candida species. 20% of patients had a history of antifungal exposure, predominantly to fluconazole. An association was found between antifungal usage and nonsusceptibility, especially in patients over 90 days of age. |
| Publication Information | Published in the Emerging Infectious Diseases journal, Volume 31, Number 10, October 2025. |
| Statistics | The study analyzed 2,443 culture-confirmed cases out of 8,647 identified candidemia cases. |
| Implications | Highlights the need for improved antifungal stewardship and infection prevention strategies to combat antifungal resistance in South Africa. |
Summary
Antifungal resistance is an increasing concern in global healthcare, as evidenced by the study of Candida bloodstream infections in hospitalized patients in South Africa. The research illuminates the critical link between recent antifungal exposure and the rise of nonsusceptible Candida species. With 48% of cases identified as nonsusceptible, and significant associations found particularly in older patients, the urgency for effective antifungal stewardship and infection control strategies cannot be overstated. This calls for heightened awareness and action to mitigate the threats posed by antifungal resistance in clinical settings.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.