Androgen Insensitivity Syndrome (AIS) is a fascinating genetic condition that significantly impacts an individual’s development and gender identity. This syndrome occurs due to androgen receptor mutations, which prevent the body from responding to male hormones, despite possessing a genetic male karyotype of 46,XY. As a result, individuals with AIS often develop external female characteristics, leading to complex discussions around gender identity and societal norms. Understanding the genetic causes of AIS, alongside its treatment options and societal implications, is crucial for fostering awareness and acceptance of those affected. This article will delve into the multifaceted aspects of AIS, shedding light on its prevalence, management strategies, and the experiences of individuals living with this condition.
Also known as testicular feminization syndrome, Androgen Insensitivity Syndrome (AIS) presents a unique intersection of genetics, gender identity, and societal perceptions. This condition arises from genetic anomalies, particularly mutations in the androgen receptor gene, which disrupt normal male development processes. Individuals diagnosed with this syndrome often grapple with complex issues related to their gender identity, as their physical traits may not align with traditional male or female classifications. The treatment for AIS typically involves a combination of medical interventions and psychological support, emphasizing the importance of understanding gender nuances and societal acceptance. By exploring the implications of AIS, we can better appreciate the rich diversity of human experiences and foster a more inclusive environment for those affected.
Understanding the Genetic Causes of Androgen Insensitivity Syndrome
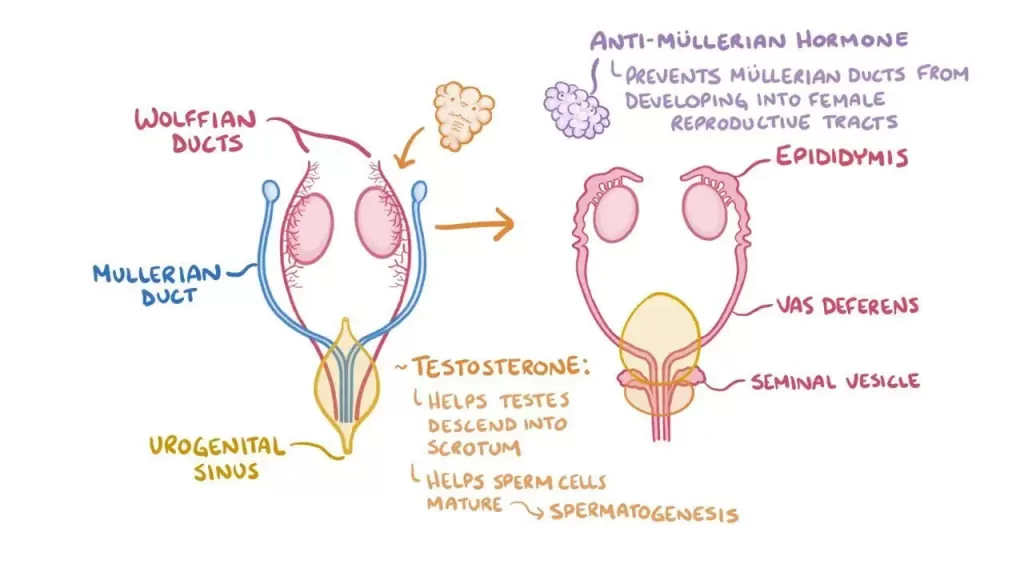
Androgen Insensitivity Syndrome (AIS) is primarily caused by mutations in the androgen receptor gene located on the X chromosome. These genetic anomalies affect how the body responds to androgens, which are crucial hormones for male development. Individuals with AIS typically have a 46,XY karyotype, indicating they are genetically male, but due to the mutations in the androgen receptor, their bodies cannot respond effectively to testosterone. This results in a spectrum of physical manifestations, ranging from complete feminization in cases of complete AIS (CAIS) to mixed traits in partial cases.
Research has identified various mutations that lead to dysfunctional androgen receptors, which can disrupt normal sexual differentiation during fetal development. The severity of AIS can vary significantly based on the nature of the mutation; some may lead to complete insensitivity, while others may allow for partial responsiveness to androgens. Understanding these genetic causes is crucial for developing targeted therapies and improving diagnostic accuracy for individuals affected by AIS.
The Impact of Androgen Receptor Mutations on Development
The mutations in the androgen receptor gene have profound implications on the development of individuals with AIS. In the absence of a functional androgen receptor, the typical male characteristics fail to develop, resulting in a female phenotype. This phenomenon challenges traditional notions of gender, as individuals diagnosed with AIS often present as female despite having male chromosomes. The developmental impact of these mutations not only alters physical characteristics but also affects psychological and social aspects of gender identity.
Individuals with AIS may experience a disconnect between their genetic makeup and their gender identity, leading to complex emotional and social challenges. The experience of growing up with a gender identity that does not align with biological expectations can lead to feelings of confusion and isolation. Understanding the impact of androgen receptor mutations is vital for providing appropriate support and counseling to those affected, as it fosters a better understanding of their unique experiences.
Treatment Options for Individuals with AIS
The management of Androgen Insensitivity Syndrome typically involves a multi-faceted approach tailored to the individual’s needs. For those diagnosed with complete AIS, hormone replacement therapy (HRT) is often utilized to align hormone levels with the individual’s gender identity. Surgical interventions, such as gonadectomy, may also be recommended to mitigate health risks associated with retained non-functional testes. These treatments aim to not only address physical health concerns but also enhance the individual’s quality of life.
Additionally, psychological support is a critical component of treatment for individuals with AIS. Counseling services can provide a safe space for individuals to explore their gender identity and navigate the societal pressures they may face. Support networks, including peer groups and educational resources, play an essential role in fostering a sense of community and acceptance, further aiding in the emotional well-being of those affected by AIS.
Societal Attitudes and Gender Identity in AIS
As societal understanding of gender continues to evolve, the experiences of individuals with Androgen Insensitivity Syndrome gain increasing visibility. The dialogue surrounding gender identity has broadened, allowing for a more inclusive perspective that recognizes the complexities of conditions like AIS. This shift encourages acceptance and understanding, which can significantly impact the lives of those affected, fostering a sense of belonging and validation in their gender identity.
However, challenges remain as societal norms and expectations may not always align with the realities of individuals with AIS. Increased awareness and education about the condition can help reduce stigma and promote inclusivity. Advocacy efforts aimed at informing the public about the genetic basis of AIS and its implications on gender identity are essential for creating a supportive environment for those living with this condition.
Recent Developments in AIS Research and Treatment
Ongoing research into Androgen Insensitivity Syndrome has revealed significant insights into the genetic underpinnings and potential therapeutic avenues for those affected. Recent studies have focused on identifying specific mutations in the androgen receptor gene and their correlation with the clinical manifestations of AIS. This research is paving the way for innovative approaches, including gene therapy, which may offer more effective treatment options tailored to individual genetic profiles.
Furthermore, advancements in understanding the psychosocial aspects of living with AIS are equally important. Research highlights the necessity for early intervention and comprehensive support systems to improve emotional and psychological outcomes for individuals with AIS. As the medical community continues to explore the genetic and societal dimensions of AIS, the goal remains to enhance the quality of life for those affected while fostering a more informed and compassionate society.
Frequently Asked Questions
What are the genetic causes of Androgen Insensitivity Syndrome (AIS)?
Androgen Insensitivity Syndrome is primarily caused by mutations in the androgen receptor gene located on the X chromosome. These mutations disrupt the body’s ability to respond to androgens, leading to the development of female physical characteristics in genetically male individuals (46,XY).
How do androgen receptor mutations affect individuals with Androgen Insensitivity Syndrome?
Androgen receptor mutations prevent the normal action of androgens like testosterone, resulting in incomplete or complete androgen insensitivity. This leads to a spectrum of physical presentations, ranging from female external genitalia in complete AIS (CAIS) to mixed traits in partial AIS (PAIS).
What treatment options are available for individuals diagnosed with Androgen Insensitivity Syndrome?
Treatment for Androgen Insensitivity Syndrome often includes hormone replacement therapy (HRT) to align hormone levels with the individual’s gender identity. Surgical interventions, such as gonadectomy for CAIS, may also be recommended to mitigate health risks, alongside psychological support to address emotional and social challenges.
How does society’s understanding of gender identity relate to Androgen Insensitivity Syndrome?
Society’s evolving perspective on gender identity plays a crucial role in the experiences of individuals with Androgen Insensitivity Syndrome. As awareness increases, discussions surrounding gender diversity and inclusivity become essential, promoting acceptance for people with AIS and recognizing their unique gender identities.
What recent developments have emerged in the study of Androgen Insensitivity Syndrome?
Recent research into Androgen Insensitivity Syndrome has focused on the genetic underpinnings of androgen receptor mutations, paving the way for potential advancements in gene therapy. Such developments aim to enhance the quality of life for individuals with AIS and emphasize the importance of early interventions and supportive care in addressing their psychological and emotional well-being.
| Key Point | Details |
|---|---|
| Definition | Androgen Insensitivity Syndrome (AIS) is a genetic condition affecting sexual differentiation. |
| Genetic Cause | Mutations in the androgen receptor gene on the X chromosome lead to AIS. |
| Prevalence | AIS affects approximately 1 in 20,000 to 1 in 64,000 live births. |
| Karyotype | Individuals with AIS typically have a karyotype of 46,XY. |
| Diagnosis | Diagnosis often occurs during puberty or when fertility issues arise. |
| Treatment Options | Management may include hormone replacement therapy and surgeries for CAIS. |
| Recent Developments | Research is advancing into gene therapy for AIS. |
| Societal Implications | Increased awareness of AIS promotes inclusivity and understanding of gender identity. |
Summary
Androgen Insensitivity Syndrome (AIS) is a complex genetic condition that profoundly impacts individuals’ gender identity and physical development. This condition arises from mutations in the androgen receptor gene, leading genetically male individuals (46,XY) to develop female physical traits due to their bodies’ inability to respond to male hormones. The prevalence of AIS is relatively low, yet it can often go unrecognized, particularly in its partial forms. Diagnosis typically occurs around puberty when secondary sexual characteristics are assessed. Treatment for AIS may involve hormone replacement therapy and surgical options to align physical traits with gender identity. Ongoing research into AIS is crucial for enhancing understanding and improving treatment options, highlighting the need for societal awareness and acceptance of diverse gender identities.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.