Altitude sickness, often referred to as acute mountain sickness (AMS), is a significant concern for anyone venturing into high altitudes, typically above 8,000 feet. As the body struggles to adapt to the decreased oxygen levels found at these elevations, it may experience a variety of distressing symptoms, including headache, nausea, and fatigue. Understanding the symptoms of altitude sickness is crucial for travelers, as early recognition can lead to timely treatment and prevent serious complications. Moreover, effective strategies for preventing altitude sickness, such as gradual ascent and proper hydration, can greatly enhance high-altitude health. In this article, we delve into the nuances of altitude sickness, offering essential insights on symptoms, prevention, and treatment for those traveling at high altitude.
High-altitude illness, commonly known as altitude sickness, encompasses a range of symptoms that can afflict individuals as they ascend to elevated terrains. This condition arises when the body fails to acclimatize to the lower oxygen levels present in mountainous regions, often leading to discomfort and health risks. Recognizing the signs of high-altitude sickness is vital, as it can manifest quickly after reaching significant elevations. Effective measures for preventing altitude-related ailments include strategic planning and maintaining hydration. Whether you’re trekking through the Himalayas or skiing in the Rockies, understanding the intricacies of altitude sickness will help ensure a safer and more enjoyable experience in elevated landscapes.
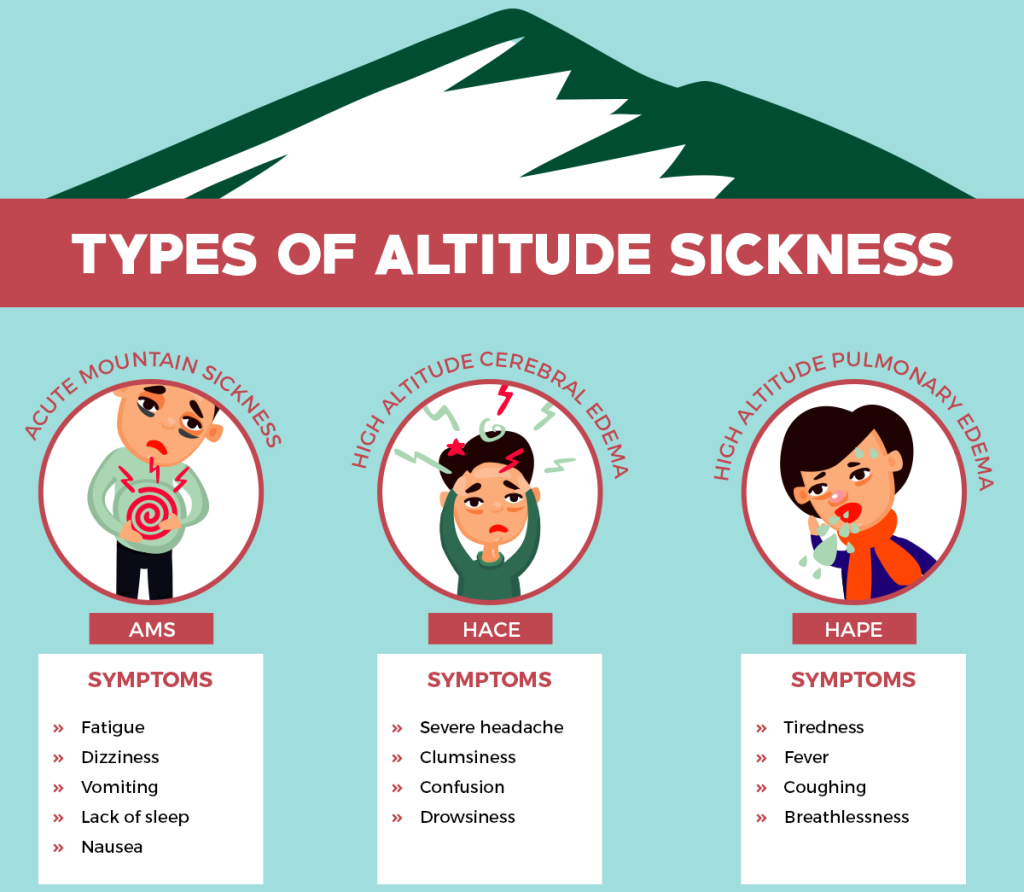
Understanding the Symptoms of Altitude Sickness
Altitude sickness, or acute mountain sickness (AMS), presents a variety of symptoms that can range from mild to severe. Common symptoms include headaches, which can intensify if not addressed, and nausea or vomiting, which may complicate the experience at high elevations. Travelers often report dizziness and lightheadedness, making it challenging to navigate even simple paths. Fatigue and weakness are frequent companions of these symptoms, as individuals may find themselves exhausted with minimal exertion. Insomnia is another prevalent issue, making it difficult to rest adequately while acclimatizing to the altitude.
In more severe cases, altitude sickness can progress to life-threatening conditions like High Altitude Pulmonary Edema (HAPE) and High Altitude Cerebral Edema (HACE). These serious ailments require immediate medical intervention and can lead to significant health risks if not recognized early. Understanding these symptoms is paramount for travelers, as early recognition and appropriate response can prevent escalation and ensure safety in high-altitude environments.
Preventing Altitude Sickness: Essential Strategies
Preventing altitude sickness is a vital aspect of high-altitude travel that every adventurer should prioritize. The most effective strategy is to ascend gradually, allowing the body ample time to acclimatize. Experts recommend limiting elevation gains to no more than 1,000 feet in a 24-hour period once reaching altitudes above 8,000 feet. Staying hydrated is equally crucial, as the body tends to lose moisture quickly at higher elevations. Consuming hydration-rich foods, such as fruits and vegetables, can support fluid intake and help mitigate dehydration, which exacerbates symptoms.
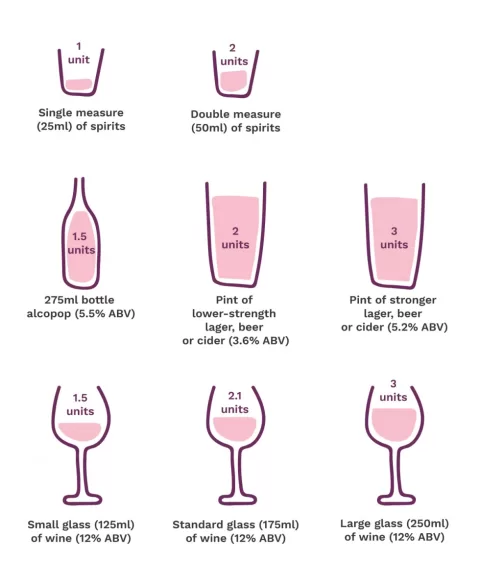
Proper nutrition plays a critical role in preventing altitude sickness as well. A diet rich in carbohydrates can provide the necessary energy for strenuous activities at high altitudes. Moreover, avoiding alcohol is advisable, as it can further dehydrate the body and hinder the acclimatization process. Engaging in moderate physical conditioning before embarking on high-altitude treks can also enhance the body’s ability to adapt, making it easier to enjoy the journey without falling victim to altitude sickness.
Treatment Options for Altitude Sickness
When altitude sickness strikes, immediate action is essential to alleviate symptoms and ensure safety. The most effective treatment is to descend to a lower altitude, as even a drop of 1,000 feet can significantly relieve symptoms. Travelers should prioritize rest and hydration, minimizing physical activity while consuming at least 3-4 liters of water daily to combat dehydration at high elevations. Over-the-counter medications, such as ibuprofen, can provide relief from headaches and muscle pain associated with altitude sickness.
For more severe cases, healthcare professionals may prescribe medications like acetazolamide (Diamox). This drug works to enhance the body’s acclimatization process by increasing breathing rates and improving oxygen levels in the bloodstream. Understanding these treatment options is crucial for travelers, as being prepared with knowledge about altitude sickness management can make a significant difference in the overall experience at high elevations.
High Altitude Health Tips for Travelers
Traveling to high altitudes requires careful planning and awareness of health tips that can enhance your experience. First, gradual ascent is not just a recommendation but a necessity. Allowing your body to acclimatize properly can prevent altitude sickness and help maintain your energy levels. Additionally, staying hydrated is fundamental; drinking water regularly can stave off the symptoms of dehydration, which are common in high-altitude environments. Incorporating hydration-rich foods into your diet can also support your body’s needs.
Another crucial tip is to listen to your body and recognize when symptoms of altitude sickness appear. If you start feeling unwell, do not hesitate to descend to a lower altitude. Engaging in light exercise before your trip can also prepare your body for the rigors of high-altitude travel, ensuring that you have the stamina needed for exploration. Lastly, consider consulting with healthcare professionals before your trip to discuss preventive medications that can aid acclimatization and overall health during your adventure.
Personal Experiences: Insights into Altitude Sickness Management
Personal accounts from climbers and travelers provide valuable insights into altitude sickness and its unpredictable nature. Many trekkers share stories of experiencing symptoms unexpectedly, emphasizing the importance of preparation and awareness. For instance, trekkers on routes like Mount Kilimanjaro often highlight the need to acclimatize thoroughly and to be ready to adjust plans based on how their bodies respond to the altitude. Listening to one’s body can be the key to preventing severe complications.
These firsthand experiences underline that altitude sickness does not discriminate based on fitness levels or previous hiking experience. Each individual may respond differently to high altitudes, making it essential to approach high-altitude adventures with caution and preparedness. By learning from others’ experiences and prioritizing safety measures, travelers can enhance their chances of enjoying high-altitude excursions while minimizing health risks.
Frequently Asked Questions
What are the common symptoms of altitude sickness?
Altitude sickness, or acute mountain sickness (AMS), can present various symptoms, including headache, nausea and vomiting, dizziness, fatigue, and insomnia. Recognizing these symptoms of altitude sickness early is crucial for effective management and safety at high altitudes.
How can I prevent altitude sickness when traveling to high altitudes?
Preventing altitude sickness involves several strategies: ascend gradually to allow your body time to acclimatize, stay hydrated, eat nutritious high-carb foods, avoid alcohol, and ensure you are physically conditioned before your trip. These high altitude health tips can significantly reduce the risk of altitude sickness.
What treatments are available for altitude sickness?
For treating altitude sickness, the most effective approach is to descend to a lower altitude. Additionally, rest, hydration, and over-the-counter medications like ibuprofen can alleviate symptoms. In severe cases, prescription medications such as acetazolamide (Diamox) may be recommended to assist with acclimatization.
What should I do if I experience symptoms of altitude sickness during my trip?
If you experience symptoms of altitude sickness, it is crucial to descend to a lower altitude immediately. Rest and hydrate while minimizing physical activity. If symptoms persist, seek medical attention, as severe altitude sickness can lead to life-threatening conditions like HAPE or HACE.
Are there specific tips for traveling at high altitude?
Yes, when traveling at high altitude, consider these tips: ascend slowly, stay well-hydrated, consume high-carb foods, avoid alcohol, and listen to your body. Always be aware of the symptoms of altitude sickness and be prepared to adjust your plans if necessary.
| Key Points | Details |
|---|---|
| What is Altitude Sickness? | A condition affecting those at high altitudes (above 8,000 feet) due to rapid ascent without acclimatization. |
| Symptoms | Headache, nausea, dizziness, fatigue, insomnia; severe cases can lead to HAPE or HACE. |
| Prevention Strategies | Gradual ascent, hydration, proper nutrition, avoid alcohol, and moderate exercise. |
| Immediate Treatment | Descend to a lower altitude, rest, stay hydrated, and take over-the-counter medication for symptom relief. |
| Prescription Medications | Acetazolamide (Diamox) can be prescribed to aid acclimatization. |
| Personal Experiences | Travelers emphasize the importance of awareness and preparedness for altitude sickness. |
Summary
Altitude sickness is a significant concern for anyone traveling to high elevations, typically above 8,000 feet. It occurs when the body struggles to adapt to reduced oxygen levels, often leading to uncomfortable symptoms such as headache, nausea, and dizziness. To prevent altitude sickness, it’s essential to ascend gradually, stay hydrated, and maintain proper nutrition while avoiding alcohol. If symptoms arise, descending to a lower elevation is the most effective treatment. By understanding altitude sickness and employing preventive strategies, travelers can enjoy their high-altitude adventures safely.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.