Acute kidney injury (AKI) is a serious medical condition characterized by a sudden decline in kidney function, which can disrupt the body’s ability to filter waste, maintain electrolyte balance, and regulate blood pressure. This critical condition can develop rapidly, often within hours or days, leading to severe health complications if not promptly addressed. Understanding the symptoms of acute kidney injury, such as decreased urine output, swelling, and fatigue, is essential for early detection and treatment. Additionally, recognizing the acute kidney injury causes—ranging from dehydration to medication effects—can help in preventing its onset. Treatments for AKI are focused on addressing the underlying issues and may include renal replacement therapy for severe cases, making it crucial to monitor kidney health diligently.
Also referred to as acute renal failure, acute kidney injury (AKI) represents a swift deterioration in renal function that can pose significant risks to overall health. This condition can manifest through various stages, where symptoms might not be immediately apparent, emphasizing the importance of awareness among at-risk individuals. Understanding the causes of acute renal failure, including prerenal and intrinsic factors, plays a vital role in prevention and management strategies. Effective treatment options are pivotal in restoring kidney function and ensuring patients regain their kidney health. With advancements in medical research, there is hope for improved outcomes and management protocols for those affected by this critical condition.
Understanding the Symptoms of Acute Kidney Injury
Acute kidney injury (AKI) can present with a wide array of symptoms that vary in severity depending on the underlying causes and the extent of kidney function impairment. Common symptoms include decreased urine output, swelling due to fluid retention, nausea, vomiting, fatigue, confusion, and occasionally shortness of breath. Many patients may not experience noticeable symptoms in the initial stages, particularly if the kidney damage is mild. This lack of overt symptoms emphasizes the importance of routine monitoring for individuals at risk, such as those with chronic diseases or those undergoing certain medical procedures.
It’s crucial for healthcare providers to recognize these symptoms early, as they can indicate a rapid decline in kidney function. For instance, decreased urine output may suggest that the kidneys are not filtering waste effectively, which can lead to dangerous levels of toxins in the body. Additionally, fluid retention can cause swelling and hypertension, creating further complications. Prompt recognition and treatment of these symptoms can significantly improve outcomes and prevent progression to more severe stages of AKI.
Causes and Risk Factors of Acute Kidney Injury
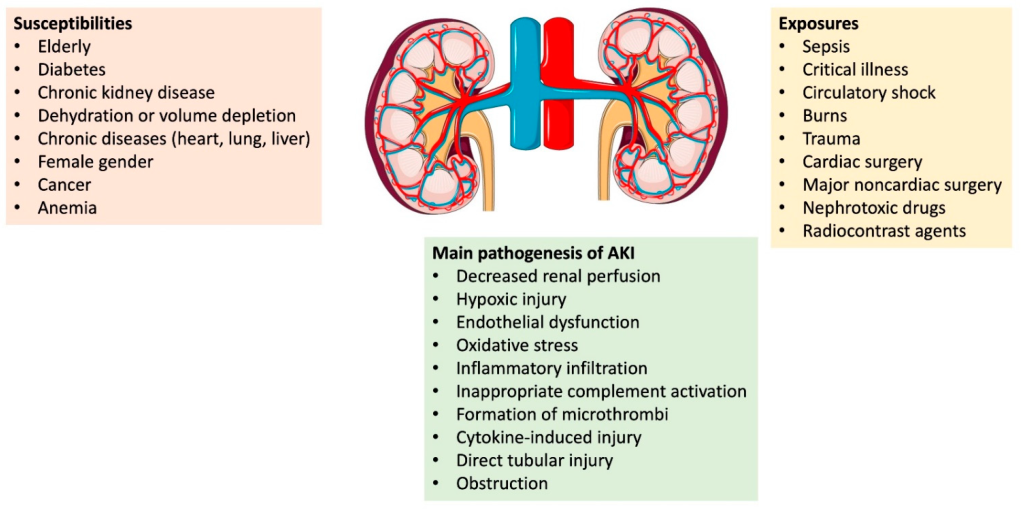
The causes of acute kidney injury can be broadly classified into three categories: prerenal, intrinsic, and postrenal. Prerenal causes typically involve conditions that reduce blood flow to the kidneys, such as dehydration, heart failure, or significant blood loss. This category is often reversible if identified and treated early. Intrinsic causes involve direct damage to the kidney tissue, which can occur due to exposure to nephrotoxins, certain medications, or infections. Postrenal causes arise from obstructions in the urinary tract, which may be due to kidney stones or tumors.
Understanding these causes is essential for implementing effective preventive strategies. For instance, patients undergoing surgeries or those with chronic illnesses should be monitored closely for signs of dehydration and renal impairment. Additionally, awareness of medications that can cause kidney damage is vital for both patients and healthcare providers to mitigate risks. By recognizing these risk factors, proactive measures can be taken to safeguard kidney health and minimize the likelihood of developing acute kidney injury.
Recent Advances in Acute Kidney Injury Treatment
Recent developments in the treatment of acute kidney injury are promising and highlight the importance of innovative approaches in managing this complex condition. For example, studies have shown that novel antidiabetic agents can significantly decrease the risk of AKI in diabetic patients, particularly those undergoing procedures like percutaneous coronary intervention (PCI). This dual benefit not only aids in managing diabetes but also protects kidney function, demonstrating the potential for pharmacological interventions to improve patient outcomes.
Moreover, clinical trials are ongoing to evaluate new therapies specifically designed for AKI management. For instance, SeaStar Medical’s pivotal trial aims to assess the effectiveness of emerging treatments for adult AKI. Such advancements not only offer hope for better recovery but also contribute to a deeper understanding of the condition’s pathophysiology. As research continues to unfold, the potential for more targeted and effective treatments for acute kidney injury becomes increasingly apparent.
Stages of Acute Kidney Injury and Their Implications
Acute kidney injury is classified into three stages based on serum creatinine levels and urine output, which are critical for guiding treatment decisions and assessing prognosis. Stage 1 signifies a mild increase in serum creatinine with a urine output of less than 0.5 mL/kg/h for six hours. In contrast, Stage 3 indicates a severe condition requiring intensive care, with significant increases in serum creatinine and markedly reduced urine output. Recognizing the stage of AKI is crucial for healthcare providers to determine the urgency of intervention and the appropriate treatment strategies.
The implications of these stages extend to patient management and outcomes. For example, patients in the early stages may respond well to conservative management, while those in advanced stages may require renal replacement therapy. Understanding these stages also helps healthcare professionals communicate effectively with patients and their families about the seriousness of the condition and the expected course of treatment. By closely monitoring kidney function and recognizing the signs of deteriorating health, timely and appropriate interventions can be initiated to improve recovery chances.
The need for multidisciplinary approaches in managing acute kidney injury cannot be overstated. Regular monitoring, early intervention, and a comprehensive understanding of the stages of AKI are essential in improving patient outcomes and minimizing long-term complications.
Promoting Kidney Health and Preventing Acute Kidney Injury
Promoting kidney health is a critical aspect of preventing acute kidney injury. Key lifestyle modifications can significantly reduce the risk of developing AKI, particularly among high-risk populations. Maintaining proper hydration is essential, as dehydration can lead to prerenal AKI. Additionally, a balanced diet low in sodium and rich in fruits and vegetables can help support kidney function and overall health. Regular physical activity is also beneficial, as it promotes better circulation and can prevent conditions like hypertension and diabetes that contribute to kidney damage.
Moreover, regular health screenings for those at risk—such as individuals with diabetes, hypertension, or a family history of kidney disease—can aid in early detection of potential kidney issues. Educating patients about the importance of medication management, particularly regarding nephrotoxic drugs, can also play a significant role in protecting kidney health. By fostering awareness and implementing preventive measures, we can work towards reducing the incidence of acute kidney injury and enhancing the quality of life for individuals at risk.
Frequently Asked Questions
What are the common symptoms of acute kidney injury (AKI)?
Common symptoms of acute kidney injury (AKI) include decreased urine output, swelling due to fluid retention, nausea, vomiting, fatigue, confusion, and shortness of breath. It’s important to note that some patients may not exhibit symptoms in the early stages, making regular monitoring essential for those at risk.
What are the main causes of acute kidney injury?
Acute kidney injury (AKI) can be caused by several factors categorized as prerenal, intrinsic, or postrenal. Prerenal causes often involve decreased blood flow to the kidneys, such as dehydration or heart failure. Intrinsic causes typically result from direct damage to kidney tissues due to toxins or medications, while postrenal causes are related to obstructions in the urinary tract, like kidney stones or tumors.
How is acute kidney injury treated?
The treatment for acute kidney injury (AKI) focuses on addressing the underlying cause, providing supportive care, and ensuring adequate blood flow to the kidneys. In severe cases, renal replacement therapy, such as dialysis, may be necessary to assist with kidney function. Recovery time can vary significantly based on the severity of AKI and the promptness of treatment.
What are the stages of acute kidney injury?
Acute kidney injury (AKI) is classified into three stages based on serum creatinine levels and urine output. Stage 1 indicates a mild increase in serum creatinine, while Stage 3 indicates a severe condition requiring intensive care. Understanding these stages is crucial for guiding treatment decisions and assessing patient prognosis.
How can I maintain kidney health to prevent acute kidney injury?
Maintaining kidney health is essential to prevent acute kidney injury (AKI). Key strategies include staying hydrated, managing blood pressure and blood sugar levels, avoiding nephrotoxic medications, and maintaining a healthy diet. Regular check-ups and monitoring kidney function, especially for those at risk, can help in early detection and prevention of AKI.
| Key Topics | Details |
|---|---|
| Acute Kidney Injury (AKI) Overview | AKI signifies a rapid decline in kidney function, impacting waste filtration, electrolyte balance, and blood pressure regulation. |
| Key Symptoms | Decreased urine output, swelling, nausea, fatigue, confusion, shortness of breath. |
| Causes of AKI | Prerenal (decreased blood flow), Intrinsic (direct kidney damage), Postrenal (obstruction in urinary tract). |
| Recent Developments | Studies on AKI in cardiac surgery, decongestion in heart failure, novel antidiabetic agents reducing AKI risk, and ongoing clinical trials. |
| Treatment Approaches | Focus on addressing underlying causes, supportive care, and possibly renal replacement therapy like dialysis. |
| Stages of AKI | Classified into stages 1 to 3 based on serum creatinine levels and urine output. |
Summary
Acute Kidney Injury is a serious health condition that poses significant risks to patient health. Understanding its symptoms, causes, and latest treatment developments is crucial for effective management. Recent advancements in research have improved strategies for monitoring and treating AKI, particularly in high-risk patient populations. Awareness of the key symptoms such as decreased urine output and swelling, along with knowledge of potential causes, can help in early detection and intervention. With ongoing research and clinical trials, healthcare providers are better equipped to manage AKI, enhancing recovery prospects and patient outcomes.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.