Thimerosal vaccines, a topic that has stirred controversy for decades, continue to ignite debates within the medical community and public forums alike. Recently, the Centers for Disease Control and Prevention (CDC) found itself in the crosshairs of this ongoing thimerosal controversy as its vaccine advisory panel recommended moving towards flu vaccines that are free from the preservative. This recommendation aligns closely with sentiments expressed by the anti-vaccine movement, fueled by concerns surrounding vaccine safety and the potential risks of additives like thimerosal. While research overwhelmingly indicates that thimerosal poses no significant risks, leading health organizations have taken steps to bolster public trust by eliminating its use in many vaccine formulations. As the CDC navigates the complex landscape of vaccine recommendations, the implications of such policies echo beyond the immediate debate, impacting everything from flu vaccine policy to the availability of RSV monoclonal antibody treatments for infants.
The discussion regarding the use of mercury-based preservatives in immunizations, particularly thimerosal, reflects broader concerns within the medical community and among the public regarding vaccine safety and efficacy. As vaccine experts emphasize the importance of safe immunization practices, alternative terms like ‘thimerosal-free vaccines’ and ‘multidose vials’ become crucial in understanding the intricacies of recommendations made by health authorities like the CDC. The skepticism surrounding these preservatives has fueled movements against vaccines, raising questions about the potential influence of the anti-vaccine ideology on public health policies. Addressing these issues, especially in light of new RSV monoclonal therapies, requires a delicate balance between ensuring community safety and maintaining public trust in vaccination efforts. As such conversations evolve, the healthcare community must remain vigilant in educating the public about sound scientific evidence and the ongoing developments in vaccination policies.
Understanding the Thimerosal Controversy
The thimerosal controversy has been a topic of heated debate within the vaccine community for decades. Thimerosal, a preservative containing ethylmercury, was commonly used in vaccines, particularly in multidose vials, to prevent contamination. However, concerns about the potential risks associated with mercury exposure led to widespread public apprehension regarding its use in childhood vaccinations. This controversy has fueled the anti-vaccine movement, which often cites thimerosal as a significant factor in vaccine safety discussions, despite scientific research showing no credible link between thimerosal and developmental disorders.
Despite the controversies, multiple studies have confirmed the safety profile of thimerosal. The Centers for Disease Control and Prevention (CDC) and the American Academy of Pediatrics (AAP) have reiterated that there is no evidence to support claims that thimerosal in vaccines poses a risk to health. In 1999, as a precautionary measure, the CDC recommended the removal of thimerosal from vaccines not because of proven safety issues but to reinforce public trust in vaccination programs. This illustrates the complex relationship between public perception and scientific evidence, particularly in the context of vaccine safety.
Impact of CDC Vaccine Recommendations
The recent recommendations by the CDC advisory panel indicate a significant shift in vaccine policy, particularly regarding the use of thimerosal in flu vaccines. By recommending only single-dose formulations that do not contain thimerosal, ACIP aims to address growing public concern and reinforce confidence in the safety of vaccines. This decision is pertinent not only for the flu vaccine but also for public health initiatives as it reflects the CDC’s ongoing commitment to adapt its strategies to the evolving landscape of vaccine hesitancy, largely driven by the anti-vaccine movement.
Additionally, the CDC’s vaccine recommendations underscore the importance of maintaining trust in immunization programs. With the resurgence of diseases that were previously controlled, due to misinformation propagated by various anti-vaccine groups, the CDC’s role is paramount in educating the public on the benefits of vaccination. By focusing on scientific evidence and transparency, the CDC strives to dispel fears surrounding vaccine components like thimerosal while encouraging consistent vaccination practices among all eligible populations.
The Role of RSV Monoclonal Antibodies
Merck’s RSV monoclonal antibody, clesrovimab, has recently gained attention as a preventative measure for infants, marking a significant advancement in combating respiratory syncytial virus (RSV). The recommendation of clesrovimab by the ACIP symbolizes a proactive approach to safeguarding vulnerable populations, particularly those who are at greater risk due to age or health conditions. RSV poses a serious threat to infants, and public health officials are keen on implementing solutions that can mitigate the virus’s impact during critical seasons.
The integration of clesrovimab into the CDC’s Vaccines for Children program highlights the importance of innovative treatments alongside traditional vaccines. By providing this monoclonal antibody as an additional preventive strategy, health policy can better address the multifaceted challenges associated with RSV. This proactive measure complements vaccination efforts, ensuring that the most susceptible infants receive adequate protection against significant respiratory illnesses.
Navigating the Anti-Vaccine Movement
The anti-vaccine movement poses unique challenges to public health, often leveraging misinformation to sway public opinion against vaccines. The emphasis on thimerosal, despite scientific evidence to the contrary, underscores the need for proactive communication strategies from health organizations. By comprehensively addressing misconceptions surrounding vaccine safety, particularly in the context of thimerosal debates, public health agencies can work to dismantle the myths that contribute to vaccine hesitancy.
Moreover, engaging with communities directly affected by vaccine misinformation can foster a collaborative environment where concerns can be acknowledged and addressed. Public health campaigns aimed at educating citizens about the benefits and safety of vaccines, as well as transparently discussing the scientific consensus on issues like thimerosal, are crucial steps in countering the narrative espoused by anti-vaccine advocates. Understanding the underlying fears of vaccine hesitancy can help tailor messaging that resonates with concerned individuals, ultimately driving higher vaccination rates.
Seasonal Flu Vaccine Policy Changes
The ACIP’s recent recommendations for seasonal flu vaccines reflect an evolving understanding of public health needs amidst ongoing concerns regarding vaccine safety. The recommendation for single-dose flu vaccine formulations without thimerosal signifies a shift that aims to increase vaccination rates by aligning with the public’s preferences for safer vaccine options. This approach not only acknowledges past controversies but also seeks to create a more supportive environment for vaccine uptake in diverse populations.
Additionally, the introduction of new vaccine formulations, including FluMist for self-administration and updated age indications for the Flublok vaccine, illustrates a proactive stance in accommodating varying preferences and demographics. Such changes in the flu vaccine policy signal a commitment to improving public health outcomes through increased accessibility and acceptability of vaccines, crucial in reinforcing herd immunity against seasonal influenza.
Future of the MMRV Vaccine Discussion
The future discussions surrounding the MMRV vaccine for children are closely watched due to the combined administration concerns with measles, mumps, rubella, and varicella viruses. While this vaccine has been a staple in childhood immunization schedules, slight risks such as febrile seizures associated with its administration have raised questions. ACIP’s decision to review its recommendations highlights the advisory panel’s commitment to evidence-based decision-making in vaccine distribution.
Moreover, ongoing debates regarding the best practices for immunization, especially concerning combinations of vaccines, emphasize the importance of vigilant monitoring and research. The cascading effects of any policy changes regarding the MMRV vaccine could have implications not only for individual health but also for broader public health outcomes, which is why the ACIP intends to evaluate its use thoroughly, balancing safety with efficacy for young children.
Frequently Asked Questions
What is the thimerosal controversy related to vaccines?
The thimerosal controversy involves concerns raised primarily by anti-vaccine groups about the safety of thimerosal, a mercury-containing preservative used in some multidose vaccine vials. Despite over 40 studies showing no link to developmental delays, the CDC recommended its removal in 1999 to improve public confidence in vaccines. The topic resurfaced during recent ACIP meetings, prompting discussions around its continued use in flu vaccines.
How does thimerosal affect CDC vaccine recommendations?
Thimerosal has affected CDC vaccine recommendations, particularly with the Advisory Committee on Immunization Practices (ACIP) voting to recommend that only thimerosal-free, single-dose flu vaccines be used for certain demographics, including children and pregnant women. This decision reflects ongoing public concerns influenced by the anti-vaccine movement, despite the scientific consensus on thimerosal’s safety.
What role does thimerosal play in the anti-vaccine movement?
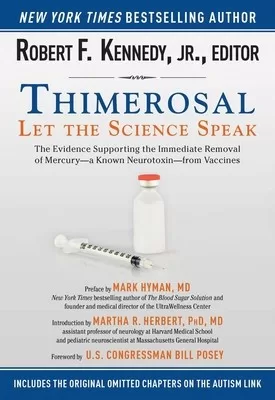
Thimerosal plays a significant role in the anti-vaccine movement, with groups arguing that it poses risks to children’s health. Leaders like Robert F. Kennedy Jr. have fueled this narrative, despite numerous studies debunking these claims. The CDC and other health organizations assert that thimerosal is safe, but these opposing views continue to contribute to vaccine hesitancy.
Are thimerosal-containing vaccines still recommended by the CDC?
The CDC typically does not recommend thimerosal-containing vaccines for children and pregnant women, encouraging the use of thimerosal-free formulations. However, the FDA has established that thimerosal in low amounts poses no harm, leading to some debates about its necessity in multidose vaccine vials.
How does the thimerosal debate impact the flu vaccine policy?
The thimerosal debate significantly impacts flu vaccine policy, as recent ACIP votes have moved towards recommending only thimerosal-free, single-dose flu vaccines for children, pregnant women, and adults. Such policies reflect an effort to reduce public fear and confusion surrounding vaccine safety, heavily influenced by the anti-vaccine narrative surrounding thimerosal.
What are the implications of the thimerosal vaccine discussions for RSV monoclonal antibodies?
While discussions about thimerosal have dominated recent vaccine meetings, the ACIP has also endorsed monoclonal antibodies like clesrovimab for preventing RSV in infants. This suggests that despite the thimerosal focus, the committee is actively working on solutions to critical health issues, including RSV, demonstrating an ongoing commitment to child health beyond the controversies.
Why did the CDC remove its thimerosal safety statement from its website?
The CDC removed its statement on thimerosal’s safety due to a lack of authorization, as noted by ACIP members during a recent meeting. This action raised concerns among committee members about transparency and the implications for public trust in vaccine safety, especially given the ongoing thimerosal controversies.
What can parents do regarding thimerosal vaccines for their children?
Parents concerned about thimerosal in vaccines should discuss their options with healthcare providers, who can recommend thimerosal-free formulations. Understanding the facts about thimerosal’s safety can also help alleviate worries. Additionally, staying informed about CDC vaccine updates is crucial in making educated decisions about vaccinations.
| Key Points |
|---|
| ACIP recommended single-dose flu shots without thimerosal. |
| Thimerosal has been used since the 1930s and is primarily found in multidose flu vaccines. |
| Over 40 studies found no link between thimerosal and developmental delays. |
| The CDC previously asked to remove thimerosal in 1999 to enhance public confidence, not due to safety concerns. |
| ACIP votes on thimerosal included children, pregnant women, and adults only receiving single-dose, thimerosal-free flu vaccines. |
| Cody Meissner, a seasoned MD, argued against concerns regarding thimerosal, citing lack of evidence of harm. |
| ACIP also discussed and voted on RSV monoclonal antibody and MMRV vaccine topics. |
Summary
Thimerosal vaccines have been the subject of controversy and debate over the years, particularly regarding their association with potential health risks. However, the recent recommendations by the Advisory Committee on Immunization Practices (ACIP) to advocate for single-dose flu vaccines that exclude thimerosal highlights the ongoing tension between scientific evidence and public perception. Despite numerous studies showing no link between thimerosal and developmental issues, the ruling reflects the influence of anti-vaccine sentiments in shaping vaccination policies. As discussions continue, it’s vital for public health communications to clarify the scientific consensus on thimerosal and its safety in vaccines.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.