Stroke care is a critical aspect of modern medicine, focusing on timely and effective treatment to minimize brain damage and enhance recovery for patients experiencing a stroke. In recent years, stroke treatment advances have transformed the landscape of care, with acute stroke centers emerging as vital hubs for rapid intervention. The establishment of the Brain Attack Coalition has provided a structured framework to address stroke care disparities and improve access to lifesaving treatments across diverse populations. Access to vital procedures like thrombectomy has increased, allowing for better outcomes for stroke victims. However, ongoing challenges remain, and continued efforts are essential to ensure that every individual receives the optimal stroke care they deserve.
Addressing the needs of individuals facing a brain attack involves an intricate web of care, ranging from emergency response strategies to specialized hospital interventions. The evolution of stroke management encompasses various forms of treatment that aim to combat the effects of an acute neurological event. Enhanced emergency medical services (EMS), along with dedicated acute stroke facilities, play a significant role in the speedy detection and intervention of cerebrovascular incidents. As the fight against conditions leading to significant disability continues, it is crucial to recognize the importance of collaboration among healthcare systems to eliminate inequalities and ensure comprehensive support for all stroke patients.
The Evolution of Stroke Care in the United States
Over the past two decades, stroke care in the United States has undergone significant transformation. Initiatives led by organizations like the Brain Attack Coalition (BAC) have initiated a paradigm shift towards evidence-based practices, resulting in the establishment of primary stroke centers (PSCs). In the late 1990s, stroke management was inconsistent, with many hospitals lacking the necessary protocols to diagnose and treat stroke patients quickly. Today, the system is more structured, ensuring that life-saving thrombolytics are administered in a timely manner and that patients receive care based on their specific needs. This evolution has been crucial in reducing the number of stroke-related disabilities and deaths, paving the way for a more organized approach to handling acute strokes.
Moreover, awareness campaigns aimed at the public have significantly improved knowledge regarding stroke symptoms and the importance of seeking immediate medical attention. Healthcare professionals are now better trained to recognize early symptoms of a stroke, a crucial factor since the onset of treatment heavily influences outcomes. Despite this progress, technical obstacles still exist in ensuring equitable access to stroke care, particularly in rural areas where resources are often limited. Continued efforts are vital in sustaining the momentum gained and ensuring that all stroke patients receive the timely intervention they require.
Challenges and Disparities in Stroke Care Access
While the improvements made in stroke care have been commendable, challenges persist, particularly concerning access disparities. Research indicates that stroke care services are often concentrated in urban centers, creating a stark imbalance for patients in rural communities. Many rural hospitals lack the designation of a stroke center, making it difficult for local patients to receive critical care during the initial hours after a stroke occurs. This situation results in inequitable outcomes and amplifies the risks associated with delayed treatment, effectively undermining the advancements achieved over the last two decades in acute stroke management.
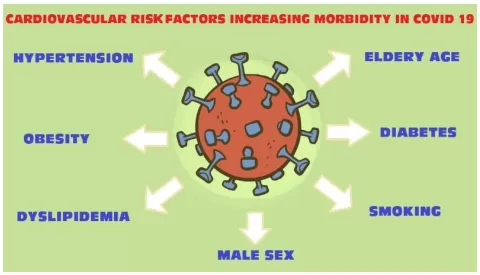
Furthermore, socioeconomic factors heavily influence access to care. Lower-income populations face a higher prevalence of strokes due to risk factors such as hypertension, diabetes, and limited health literacy regarding stroke symptoms. Addressing these disparities necessitates a multi-faceted approach, involving public health campaigns geared towards education, improved emergency medical services training, and enhanced community resources to ensure that all individuals, regardless of their geographic location or socioeconomic status, can access the high-quality stroke care that is crucial for survival.
Innovations in Thrombectomy Access and Techniques
One of the critical advancements in stroke management has been the evolution of thrombectomy techniques, which play an essential role in treating large vessel occlusions. This procedure, which involves the mechanical removal of a clot from the cerebral artery, has been shown to significantly improve outcomes for patients facing ischemic strokes. However, access to thrombectomy remains inconsistent, particularly affecting rural areas where specialized facilities are scarce. A robust mechanism is necessary to streamline patient transfers to comprehensive stroke centers capable of providing these advanced interventions.
Recent studies have highlighted that while many hospitals are equipped for initial stroke assessment, they often lack the resources to perform complex procedures like thrombectomy. This underscores the importance of developing a coordinated care network that not only rapidly identifies candidates for thrombectomy but also ensures they are swiftly transferred to appropriate facilities. Moreover, ongoing education for EMS and healthcare professionals is vital to reduce the time it takes for these patients to reach specialized care, ultimately increasing the likelihood of favorable outcomes following a stroke.
Educational Initiatives for Improved Stroke Awareness
Public education plays a pivotal role in enhancing the recognition of stroke symptoms and ensuring timely response in emergency situations. Initiatives aimed at educating the public about the warning signs of a stroke, such as sudden numbness on one side of the body, confusion, difficulty speaking, and severe headaches, can greatly improve outcomes. The more the population is aware of these symptoms, the better their chances of seeking immediate medical care, leading to quicker treatment and better recovery rates.
Health organizations must continue to prioritize stroke awareness campaigns, focusing on high-risk populations who may not have access to appropriate educational materials. Community outreach programs, social media campaigns, and collaboration with local healthcare providers can help create a more informed public. By elevating stroke education, we not only empower individuals to act quickly when symptoms arise but also foster a culture of proactive health management that could dramatically decrease the incidence of stroke-related complications.
The Role of Telehealth in Stroke Management
Telehealth has emerged as a vital tool in stroke management, particularly in rural areas where access to specialized care may be limited. By utilizing telecommunication technology, healthcare providers can leverage remote expertise to assess and manage stroke patients swiftly. This approach can significantly improve the coordination of care, allowing for rapid diagnosis and treatment recommendations without the immediate need for a patient to travel long distances. It facilitates timely interventions that are crucial for minimizing brain damage during a stroke.
Moreover, telehealth services can enhance the education of local medical staff, providing them with the resources and knowledge necessary to handle stroke situations more effectively. For instance, clinicians in remote areas can consult with experts in real-time during critical moments, ensuring that they are making informed decisions while managing a stroke patient. As the telehealth infrastructure continues to develop, its integration into the stroke care continuum will be crucial for successfully addressing care disparities and enhancing overall treatment outcomes.
Future Directions in Stroke Care Research
Research in stroke care remains a dynamic field, aiming at finding innovative solutions to enhance treatment efficacy and patient outcomes. Current studies focus on understanding the mechanisms of stroke and identifying biomarkers that could lead to more personalized treatment approaches. This research is vital for developing targeted therapies that could significantly improve recovery and rehabilitation outcomes. Furthermore, recognizing that stroke is not a uniform condition, ongoing studies aim to tailor interventions based on individual patient profiles, which could lead to better management strategies.
Additionally, exploring the use of artificial intelligence in stroke diagnosis and treatment is a frontier that could revolutionize stroke care. AI algorithms can analyze imaging data rapidly to assist in detecting strokes more accurately and efficiently than traditional methods. As technology advances, integrating these innovations into existing stroke care protocols will be essential in tackling the current challenges faced by the medical community and fostering a proactive approach toward stroke management.
The Importance of Multidisciplinary Teams in Stroke Care
Effective stroke care relies heavily on the collaboration of multidisciplinary teams that incorporate various healthcare professionals, including neurologists, radiologists, emergency medical personnel, and rehabilitation specialists. Such teams ensure that all facets of stroke management are addressed, from rapid diagnosis and acute treatment to rehabilitation and long-term care planning. By working together, these teams can develop comprehensive care plans that are tailored to the individual needs of stroke patients, maximizing their chances of recovery.
The establishment of multidisciplinary teams has also proven beneficial in reducing treatment delays and improving communication among healthcare providers. With clear protocols, team members can quickly share critical information that affects patient outcomes, leading to better-coordinated care. As the stroke care field continues to evolve, fostering an environment where teamwork and collaboration are prioritized will be essential in further enhancing care standards and addressing the challenges still present in managing stroke patients.
Addressing the Consequences of Stroke on Daily Life
Life after a stroke can be challenging, with many patients facing physical, emotional, and cognitive changes that impact their daily activities. Rehabilitation plays a crucial role in helping individuals regain their independence and improve their quality of life. This often requires an interdisciplinary approach to address the diverse needs of stroke survivors, encompassing physical therapy, occupational therapy, speech-language pathology, and psychological support. By addressing these areas comprehensively, healthcare providers can significantly enhance the recovery trajectory for stroke survivors.
Moreover, ongoing support from healthcare providers and community resources is essential in helping stroke survivors reintegrate into their daily lives. Support groups, educational programs, and access to adaptive technology can empower individuals to navigate their post-stroke challenges effectively. As awareness of the long-term consequences of stroke increases, healthcare systems must prioritize not only acute care but also comprehensive rehabilitation and community support to foster meaningful recovery and improve the overall well-being of stroke survivors.
The Role of Policy in Advancing Stroke Care
Policy development is a key component in advancing stroke care systems and addressing the disparities that exist across the nation. By implementing legislative measures focused on improving access to quality stroke care, policymakers can facilitate necessary funding for stroke centers and enhance the integration of services across hospitals. Advocacy for stroke care must reach governmental and healthcare entities to create a more equitable service landscape that prioritizes timely access to treatment.
Furthermore, policies that promote ongoing education for healthcare professionals, encourage research in stroke treatment advances, and advocate for public awareness initiatives can lead to systemic changes in how stroke care is delivered. Legislative backing for issues such as telehealth expansion can also bridge the gap in rural areas, ensuring that all patients receive timely and appropriate interventions. Collaborative efforts between stakeholders will be essential in shaping a healthcare landscape that supports optimal stroke care for all.
Frequently Asked Questions
What are the latest advances in stroke treatment that enhance patient outcomes?
Recent advances in stroke treatment include improved methodologies for thrombolysis and the rise of thrombectomy access, which allows for the removal of blood clots in acute stroke patients. Technologies for brain imaging have also progressed, enabling faster and more accurate diagnosis. Furthermore, the establishment of comprehensive stroke centers ensures that patients receive timely and evidence-based care, significantly improving outcomes.
How do acute stroke centers function to provide optimal stroke care?
Acute stroke centers are designed to rapidly diagnose and treat stroke patients by employing trained teams available 24/7. They utilize protocols for administering emergency treatments like thrombolytics directly at the site. Additionally, these centers are equipped for immediate transfer to higher-level facilities, such as comprehensive stroke centers, if necessary, ensuring a seamless continuum of care for all stroke patients.
What is the role of the Brain Attack Coalition in improving stroke care?
The Brain Attack Coalition plays a vital role in developing guidelines and frameworks to enhance stroke care across the United States. Their initiatives focus on establishing primary stroke centers, promoting equitable access to treatment, and improving education about stroke symptoms and responses. By addressing stroke care disparities, the Brain Attack Coalition aims to improve treatment outcomes and reduce stroke-related mortality.
What disparities exist in stroke care access, particularly in rural areas?
Stroke care disparities are pronounced in rural areas, where many hospitals lack the necessary resources and recognition as stroke centers. As highlighted by recent studies, a significant proportion of rural emergency departments do not have any level of stroke care designation, making it difficult for residents to access timely treatment. Efforts are being made to bridge these gaps through telehealth and improved transport protocols.
How can telehealth improve access to stroke care for patients in remote locations?
Telehealth enhances access to stroke care by connecting emergency services and remote hospitals with specialized neurologists through video conferencing. This allows for rapid assessments and decision-making regarding patient transfers to comprehensive stroke centers. By utilizing telehealth, even patients in isolated areas can receive timely consultations, significantly reducing delays in treatment.
What critical factors contribute to the distribution of stroke centers in the United States?
The distribution of stroke centers in the U.S. is influenced by geographical population density, local health statistics, and available resources. Coastal areas typically have a higher concentration of stroke centers, while many rural regions lack sufficient facilities. Addressing these imbalances requires targeted policies to enhance stroke care availability, particularly in underserved areas.
What are the benefits of mechanical thrombectomy in stroke care?
Mechanical thrombectomy is a critical intervention for acute ischemic stroke, as it can effectively restore blood flow to the brain when performed promptly. Studies indicate that patients who undergo thrombectomy have higher chances of better outcomes and reduced disability. However, access to this procedure remains limited, particularly in rural areas, necessitating ongoing improvements in treatment accessibility.
What strategies are being implemented to educate the public about stroke symptoms and care?
Public health initiatives are focusing on increasing awareness of stroke risk factors and symptoms through community outreach programs and educational campaigns. By promoting the importance of recognizing stroke symptoms early and the necessity of calling emergency services, these strategies aim to reduce the delay in seeking medical care, ultimately improving stroke outcomes.
How is stroke care evolving to meet the needs of diverse populations?
Evolving stroke care involves addressing health disparities through targeted educational outreach, integrating cultural competency in care delivery, and enhancing access to services in underserved communities. Initiatives aimed at public health education, particularly within at-risk populations, are crucial for improving recognition of stroke symptoms and ensuring that all individuals have equitable access to timely stroke care.
How do stroke care protocols enhance emergency response for patients?
Stroke care protocols streamline the emergency response process by ensuring that trained personnel know the exact steps to take when a stroke patient arrives. These protocols include rapid patient assessment, immediate neuroimaging, and timely administration of thrombolytics or transfer to a higher-level care facility if needed. This organized approach minimizes delays and improves the overall efficacy of stroke treatment.
| Key Points | Details |
|---|---|
| Fragmented Stroke Care | Historically, stroke care was disjointed, with hospitals often failing to follow evidence-based guidelines. |
| Public Awareness | Most people were unaware of stroke symptoms, delaying necessary medical attention. |
| Brain Attack Coalition (BAC) Formation | Established in 2000 to create a framework for Primary Stroke Centers (PSCs) across the U.S. |
| Advancements in Stroke Care | The establishment of stroke centers significantly increased adherence to treatment protocols and improved patient outcomes. |
| Inequities in Care | Access to stroke care is still uneven, especially in rural areas where facilities are limited. |
| Importance of Public Education | Enhancing public awareness of stroke symptoms and risks remains a priority. |
| Barriers to Thrombectomy | Timely access to thrombectomy is crucial, yet disparities exist, particularly in rural settings. |
| Ongoing Challenges | Despite advancements, disparities and challenges in logistics and resources persist for stroke care. |
Summary
Stroke care has seen substantial improvements over the past 25 years, transitioning from a fragmented system to a more coordinated framework that prioritizes timely treatment and patient education. Nevertheless, challenges remain, particularly in ensuring equitable access to specialized care in rural areas. As stroke continues to be a leading cause of disability and death, it is vital for healthcare systems to focus on enhancing stroke care to bridge these gaps and further improve patient outcomes.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.