The role of CT in diagnosing subarachnoid hemorrhage (SAH) is pivotal in emergency medicine, providing rapid and accurate assessment for this life-threatening condition. With the inevitability of complications arising from untreated SAH, early detection through a **Computed Tomography (CT)** scan can dramatically alter patient outcomes. This non-invasive imaging technique exhibits remarkable **CT scan sensitivity**, especially within the first six hours following symptom onset, allowing clinicians to distinguish between SAH and other causes of headaches. In cases where CT results are inconclusive, alternative diagnostic approaches, such as **lumbar puncture for SAH**, may be employed to confirm the presence of blood in cerebrospinal fluid. Understanding the strengths of CT, along with other emergency imaging techniques like **MRI in SAH diagnosis**, underscores the importance of timely interventions in the management of subarachnoid hemorrhage.
In examining the diagnostic protocols for subarachnoid hemorrhage, it’s essential to explore various terminologies associated with this critical condition. Often characterized by a sudden intracranial bleed into the subarachnoid space, SAH necessitates prompt medical evaluation and imaging to ensure swift diagnosis and treatment. Computed tomography serves as the frontline imaging modality, providing essential insights into this potentially fatal ailment. Alternative diagnostic measures, including **lumbar puncture for SAH** and **Magnetic Resonance Imaging (MRI)**, complement CT scans, enhancing overall diagnostic accuracy. A clear understanding of the interplay between these methods is crucial for timely and effective patient care in emergency settings.
The Importance of Early Diagnosis in Subarachnoid Hemorrhage
Subarachnoid hemorrhage (SAH) is a critical condition where timely and accurate diagnosis is essential for patient survival. Early detection can significantly affect prognosis and treatment outcomes. In the emergent healthcare environment, acute presentation of SAH often features symptoms like sudden severe headaches and altered mental status, necessitating rapid diagnostic interventions. Clinicians must prioritize establishing a diagnosis quickly to initiate appropriate management, especially in emergency settings.
To enhance diagnostic accuracy, the application of advanced imaging techniques, especially CT scans, during the initial hours of symptom onset is critical. Utilizing these methods allows healthcare providers to make informed decisions about urgent neurosurgical interventions or other therapeutic strategies, ultimately improving survival rates and reducing the incidence of secondary complications such as vasospasm or rebleeding.
CT Scan Sensitivity for Diagnosing SAH
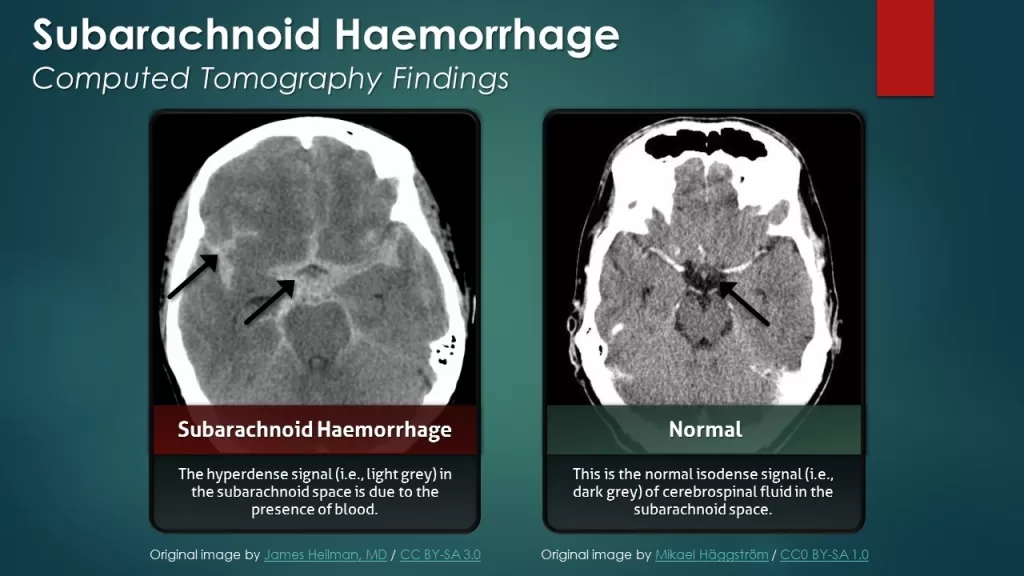
CT imaging, particularly non-contrast CT (NCCT), has proven to be exceptionally sensitive in diagnosing SAH, particularly when scans are performed shortly after symptom onset. Studies indicate that the sensitivity of CT can exceed 95% within the first six hours, making it invaluable in acute settings where time is of the essence. This high sensitivity allows for the rapid exclusion of SAH in many patients, enabling clinicians to proceed with appropriate treatment without unnecessary delays.
However, as time progresses post-symptom onset, the sensitivity of CT diminishes, falling to about 70% by day three. Therefore, understanding the critical window for CT diagnostic effectiveness is vital for healthcare professionals. This knowledge can prevent misdiagnosis and ensure that appropriate follow-up measures, such as lumbar puncture or MRI, are pursued when CT results are inconclusive.
Lumbar Puncture: A Critical Follow-Up Procedure
In cases where CT imaging results are negative yet clinical suspicion for SAH remains high, a lumbar puncture (LP) becomes an essential next step in the diagnostic process. The ability of an LP to identify altered cerebrospinal fluid (CSF) profiles, such as the presence of xanthochromia, plays a key role in confirming or ruling out SAH. Research has shown that failing to perform LP in appropriately selected patients can lead to significant missed diagnoses, potentially endangering patient lives.
Timing is particularly crucial for LP efficiency; conducting the procedure within 6-12 hours after the initial symptoms can yield the most reliable results. Clinicians should conduct a thorough assessment, weighing the risks of complications against the high stakes of missing a SAH diagnosis when symptoms are clinically indicative, highlighting the importance of procedural expertise in emergency settings.
MRI and Its Role in Subarachnoid Hemorrhage Diagnosis
Although CT remains the primary imaging tool for SAH diagnosis, MRI offers supplementary diagnostic value in atypical cases or when CT results are inconclusive. Advanced MRI techniques, including FLAIR and GRE sequences, help detect subtle changes in brain tissue and chronic hemorrhage that a CT scan may overlook. Employing MRI can thus facilitate a more comprehensive evaluation of potential hemorrhagic events.
Moreover, MRI aids in the exploration of post-hemorrhagic complications, such as delayed cerebral ischemia, providing a critical advantage in the management of patients following an SAH. Incorporating MRI into the diagnostic protocol ensures a more thorough assessment, enhancing the likelihood of identifying all potential complications, thereby improving overall patient management and care.
Guidelines for Effective SAH Diagnosis and Management
Establishing robust guidelines for diagnosing subarachnoid hemorrhage is crucial in emergency care settings. Current recommendations emphasize the utilization of non-contrast CT as the first-line imaging modality for suspected SAH, reinforcing its centrality in clinical practice. Following initial CT assessment, clinicians may choose to employ ancillary methods like CT angiography or lumbar puncture, based on individual patient circumstances and clinical judgement.
The development of a systematic approach to SAH diagnosis ensures that practitioners can optimize patient outcomes by enhancing diagnostic precision. By integrating imaging findings with clinical assessments and risk stratification, healthcare providers can effectively tailor interventions for those at high risk of complications, promoting evidence-based decision-making and improving the standard of care in the management of SAH.
Frequently Asked Questions
What is the role of CT in diagnosing subarachnoid hemorrhage (SAH)?
CT plays a critical role in diagnosing subarachnoid hemorrhage (SAH), especially as a first-line imaging modality in emergency settings. Non-contrast CT (NCCT) scans have a high sensitivity of over 95% if performed within the first six hours post-symptom onset, allowing for rapid identification of blood in the subarachnoid space.
How does CT scan sensitivity impact the diagnosis of subarachnoid hemorrhage?
The sensitivity of CT scans for diagnosing subarachnoid hemorrhage is vital for effective treatment. High sensitivity—over 95% within six hours—enables most cases of SAH to be identified early, while sensitivity decreases significantly over time, dropping to around 70% by day three.
When should a lumbar puncture be used in the diagnosis of SAH after a CT scan?
A lumbar puncture (LP) is recommended when a CT scan is negative for SAH but clinical suspicion remains high. Conducting the LP approximately 6-12 hours after symptom onset enhances cerebrospinal fluid (CSF) clarity and can help confirm SAH if CT results are inconclusive.
What are the advantages of using MRI in conjunction with CT for diagnosing subarachnoid hemorrhage?
While CT is the primary tool for diagnosing SAH, MRI can provide additional information, especially when CT results are inconclusive. MRI techniques, such as FLAIR and GRE sequences, can detect subtle or chronic hemorrhages, aiding in comprehensive diagnostic assessments and management planning.
How do emergency imaging techniques like CT contribute to the timely diagnosis of subarachnoid hemorrhage?
Emergency imaging techniques, particularly CT, are crucial for the timely diagnosis of subarachnoid hemorrhage. The rapid acquisition and high sensitivity of CT scans allow healthcare providers to quickly identify SAH, facilitating early intervention and improving patient outcomes in acute clinical scenarios.
| Key Points | Details |
|---|---|
| Subarachnoid Hemorrhage (SAH) | A severe condition caused by bleeding into the subarachnoid space, often from ruptured aneurysms. |
| Importance of Diagnosis | Early detection is crucial to prevent complications like rebleeding and vasospasm. |
| CT as First-Line Modality | CT scans are preferred in emergency settings for rapid diagnosis due to their speed and availability. |
| Sensitivity of CT | NCCT shows over 95% sensitivity within the first six hours but decreases significantly afterwards. |
| Use of Lumbar Puncture (LP) | LP is indicated if CT is negative but clinical suspicion is still high; timing is essential. |
| CT Imaging Characteristics | CT reveals increased density in the subarachnoid space indicating blood presence; Fisher scale aids grading. |
| MRI in Diagnosis | MRI can support diagnosis when CT results are inconclusive, especially for chronic hemorrhages. |
| Guidelines for Diagnosis | NCCT is recommended as the first imaging, with further tests based on clinical judgment. |
Summary
The role of CT in diagnosing subarachnoid hemorrhage is fundamental, as it serves as the primary imaging technique in emergency medicine. With its high sensitivity rates, especially within the critical early hours post-symptom onset, CT effectively assists clinicians in rapid diagnosis and management of this life-threatening condition. The integration of supplementary diagnostic methods, such as lumbar puncture and MRI, further enhances the precision of diagnosing SAH, ensuring timely treatment and improved patient outcomes. By optimizing the use of these diagnostic modalities, healthcare professionals can significantly mitigate the risks associated with delayed recognition and intervention for subarachnoid hemorrhage.
The content provided on this blog (e.g., symptom descriptions, health tips, or general advice) is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the guidance of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you believe you may have a medical emergency, call your doctor or emergency services immediately. Reliance on any information provided by this blog is solely at your own risk.